Acute Myeloid Leukemia
Original Editors - Kevin Mooney & Erik Rice from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Kevin Mooney, Erik Rice, Lucinda hampton, Elaine Lonnemann, Vidya Acharya, Kim Jackson, Shaimaa Eldib, WikiSysop, Wendy Walker, George Prudden and Sarah Haerinck
Definition/Description[edit | edit source]
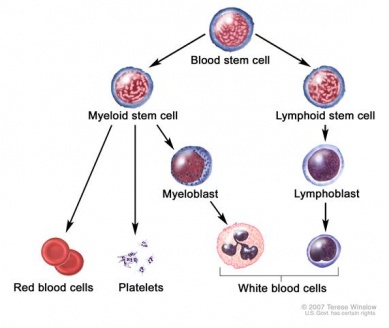
Acute Myeloid Leukemia (AML) is a type of cancer involving the blood and bone marrow. The main cell involved in this disorder is myeloid stem cells which can become either red blood cells, white blood cells, or platelets. In this disorder, Myeloid stem cells become a type of immature white blood cell called myeloblasts. These myeloblasts never become healthy white blood cells. Abnormal red blood cells, white blood cells, or platelets begin to crowd in the bone marrow to prevent healthy cells from forming.[1]
Prevalence[edit | edit source]
Acute Myeloid Leukemia is the most common leukemia in adults, comprising 80% of adult acute leukemias. The other 20% of AML patients are children. The incidence of AML increases with each decade of life with the median age of onset at 63 years old. People over the age of 70 are 12 times more likely to develop AML. Acute Myeloid Leukemia remains a rare condition with 12,000 new cases per year.[2]
Characteristics/Clinical Presentation[edit | edit source]
Initial clinical presentations of AML are related to pancytopenia, the reduction of all cell counts, reflecting the leukemic cell replacement of bone marrow. These signs and symptoms include:
- Infections due to lack of neutrophils
- Increased bleeding secondary to platelet deficiency
- Bleeding due to minor trauma, bleeding of the gums, mid-cycle menstrual bleeding, or heavy bleeding with menstruation
- Petechiae (small purplish spots caused by intradermal bleeding)
- Fatigue, loss of energy, and shortness of breath upon exertion due to low red blood cell count (anemia).
- Leukemia cutis (multiple purplish papules or diffuse rash)
- Splenomegaly occurs in 50% of patients
- Bone discomfort (especially in ribs, sternum, and tibia)
- Older adults may experience delirium, progressive weakness, and pallor.[2]
Associated Co-morbidities[edit | edit source]
Other co-morbidities associated with AML include:
- Anemia- Low numbers of red blood cells
- Thrombocytopenia- low platelet counts
- Neutropenia- low white blood cell counts
- Diabetes- Metabolic disorder characterized by increased blood glucose levels resulting from defects with insulin secretion and/or utilization
- Lupus- Chronic inflammatory disease of connective tissue in which the bodys immune system malfunctions and attacks healthy tissue
- Multiple Sclerosis- Progressive inflammatory disease of the CNS
- Rheumatoid Arthritis- Chronic inflammatory autoimmune disease that targets the joint synovium[3]
Medications[edit | edit source]
Medications used to treat AML include:
- Chemotherapy drugs (most common)- Cytarabine (cytosine arabinoside) and anthracycline drugs such as daunorubicin, idarubicin, and mitoxantrone
- Other chemotherapy drugs- Methotrexate, hydroxyurea, cladribine, fludarabine, and topotecan
- ATRA- A form of Vitamin A
- Arsenic Trioxide
- Corticosteroid drugs- Prednisone and dexamethasone[4][1]
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
Diagnostic tests for AML include:
- History and Physical Examination
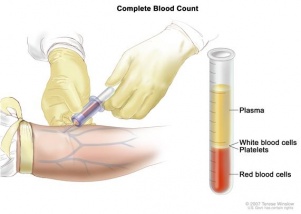
- Blood Test: Tests of patients with AML will commonly reveal increased leukocyte count initially with excessive immature cells as well as low red blood cell and platelet counts.
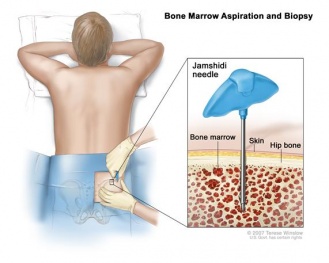
- Bone marrow biopsy and aspiration: The removal of bone marrow, blood, and bone will be looked at by the pathologist under a microscope for signs of cancer.
- Immunophenotyping: It is the process used to determine the subtype of AML by comparing the cancer cells to normal cells in the immune system. [1][2]
Etiology/Causes[edit | edit source]
Although the exact causes of AML are unknown, there are many risk factors associated with AML including:
- Smoking
- Chemical exposure (especially long term exposure to high levels of benzene)
- Cancer treatment in the form of chemotherapy drugs called alkylating agents and platinum agents
- Radiation exposure
- Blood disorders- polycythemia vera, essential thrombocythemia, and idiopathic myelofibrosis
- Genetic Syndromes- Fanconi anemia, Bloom syndrome, Ataxia-telangiectasia, Blackfan-diamond syndrome, Schwachman syndrome, Li-Fraumeni syndrome, Neurofibromatosis I, Kostmann syndrome, Down syndrome, and Trisomy 8
- Family history of a close relative with AML
- Male gender [5]
Systemic Involvement[edit | edit source]
Patients with AML can develop a variety of systemic complications including:
- Headache/disorientation- due to abnormal white blood cells infiltrating the CNS
- Anemia which is accompanied by pallor, fatigue, malaise, hypoxia, and bleeding- Caused by rapidly proliferating leukocytes inhibiting formation of erythrocytes and thrombocytes.
- Infections (pneumonia) and mouth/throat ulcerations- Caused by increased numbers of immature or abnormal leukocytes which are unable to fight off infections
- Increased metabolic rate with weakness, pallor, and weight loss- Caused by increased leukocyte production which require increased nutrient production; destruction of cells also increases metabolic waste
- Hyperuricemia which may lead to renal pain, obstruction, and infection; later development includes renal insufficiency with uremia- Caused by a great number of leukocytes being destroyed which releases large amounts of uric acid; in late stages, leukocytes infiltrate the kidneys
- Enlarged organs (spleen,liver)- Caused by increased number of white blood cells accumulating within liver and spleen causing tissue distension
- Lymphadenopathy and bone pain- Caused by excessive number of white blood cells accumulating in lymph nodes and bone marrow[2]
Medical Management (current best evidence) [edit | edit source]
The primary treatment of Acute Myeloid Leukemia is chemotherapy. The treatment of AML can be divided into three phases which include:
- Induction- This is the first phase which clears the blood of leukemia cells and reduces the number of blasts in the bone marrow. The goal is to return blood counts to a normal level over time. This should rid the body of signs of the disease for an extended period of time.
- Consolidation- This is administered after a rest period where the patient recovers from the induction phase. This phase is meant to kill the small number of leukemia cells that are still present. These cells cannot be seen because there are so few left after the induction phase.
- Maintenence- This phase is necessary in only certain types of leukemia and includes giving low doses of a chemo drug for months or years after the consolidation phase.
There are 4 types of standard treatments for AML which include:
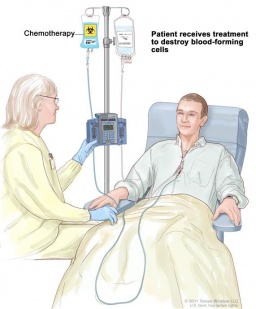
- Chemotherapy- Uses drugs to stop the gorwth of cancer cells either by killing the cells or stopping them from dividing. Chemo can be administered by mouth or injected into a vein or muscle to enter the blood stream to reach the cancer cells throughout the body (systemic chemotherapy). Chemo can also be administered directly into the Cerebrospinal fluid (intrathecal chemotherapy). This technique can be utilized when adult AML has spread or may spread to the brain or spinal cord. Chemotherapy can also be administered into a body cavity such as the abdomen or organ affecting only the specified region (regional chemotherapy). The way the chemotherapy is administered depends on the subtype of AML.
- Radiation Therapy- Uses high energy X-rays or other types of radiation to kill cancer cells or keep them from growing. There are 2 types of radiation therapy, external and internal radiation. External radiation utilizes a machine outside the body to direct radiation towards the cancer. Internal radiation uses radioactive material encapsulated in needles, seeds, wires, or catheters placed directly into the affected region. The type of radiation therapy depends on the subtype of AML.
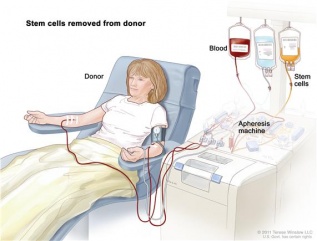
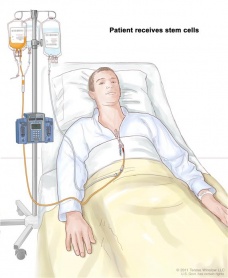
- Stem Cell Transplant- Method of administering chemo and replacing blood forming cells that are affected or destroyed by the cancer treatment. Stem cells are removed from the patients (or donors) blood or bone marrow. These cells are then frozen and stored. After chemotherapy has completed, the cells are thawed and reinfused into the patients bloodstream. These reinfused stem cells restore the body's blood cells.
- Targeted Therapy- Uses drugs or other substances to destroy specific cancer cells without harming the patients's normal cells. Monoclonal antibody therapy is a type of targeted therapy being studied for adult AML treatment. This therapy uses antibodies made in a laboratory from a single type of immune cell. These antibodies identify structures on cancer cells or normal substances that help cancer cells grow. The antibodies destroy, block, or prevent the cancer cells from spreading. These antibodies are administered via an infusion. They may be used alone or with other types of drugs.[2][1]
Physical Therapy Management (current best evidence)[edit | edit source]
Physical Therapy and exercise are indicated for patients with Acute Myeloid Leukemia undergoing cancer treatments. These interventions are aimed at symptom management, preservation of muscle function, pain control, and increased quality of life. Physical Therapy interventions for the patient with AML include:
- Aerobic Training- Studies have shown that 12 minutes of walking 5x per week can reduce fatigue, symptom distress, anxiety, and depressive status while maintaining cardiovascular health. This also can help reduce secondary effects of bedrest including contractures, bed sores, GI dysfunction, pulmonary hygeine, etc. [6](LoE:1b)
- Strength Training- Studies have shown that strength training combined with aerobic exercises 3x per week, twice daily, for 30 minutes improves cardiorespiratory endurance, reduces total fatigue and depression, maintains quality of life, and may reduce inflammatory markers. Strength training can include UE and LE resistive activities with a theraband, active range of motion against gravity, gripping activities, etc.[7](LoE:4)
- Pain Management- Modalities including TENS, hot packs, cold packs, massage, and positioning can be utilized in order to manage pain associated with AML treatments.
- Stretching- Daily stretching routines including sustained stretch, active and passive ROM, splinting, or orthotics may help offset the adverse affects of bedrest, especially contractures due to prolonged immobilization and fatigue. Stretching should be done at least 5x per week and repeated 4x for 12-15 seconds per muscle group.
All of the above interventions can be done throughout the cancer treatments; however, the following precautions should be taken:
- No exercise if patient is extremely fatigued, has low red cell counts (anemia), or has become ataxic.
- Avoid public areas if white blood cell counts are below 3,500 due to increased risk for infection.
- If patient is experiencing neuropathy be aware of increased risk of falls due to impaired sensation and pain.
- Be aware of adverse affects of medications
- Practice universal precautions due to the patient being immunocompromised.[8](LoE:5)
Differential Diagnosis[edit | edit source]
AML is a medical emergency and needs to be differentiated from other conditions that may mimic its presentation. The best way to avoid a misdiagnosis is for the doctor to review a patient's peripheral blood smear at the time of initial evaluation for all patients with a hematologic disease. The following conditions are other possible diagnostic considerations for patients with AML:
- Acute Lymphoblastic Leukemia (ALL)
- Agnogenic Myeloid Metaplasia with Myelofibrosis
- Anemia
- Aplastic Anemia
- Bone Marrow Failure
- Chronic Myelogenous Leukemia
- Lymphoma, B-cell
- Lymphoma, Lymphoblastic
- Myelodysplastic Syndrome
- Agranulocytosis (severe subset of neutropenia)
- Myelophthisic Anemia[9]
Case Reports/ Case Studies[edit | edit source]
1. Acute Myeloid Leukemia Case Study
2. Battaglini CL, Hackney AC, Garcia R, Groff D, Evans E, Shea T. The effects of an exercise program in leukemia patients. Integr Cancer Ther. 2009;8(2):130-8.
3. Tan SY, Poh BK, Chong HX, et al.Physical activity of pediatric patients with acute leukemia undergoing induction or consolidation chemotherapy. Leuk Res. 2013;37(1):14-20.
4. Chang PH, Lai YH, Shun SC, et al. Effects of a walking intervention on fatigue-related experiences of hospitalized acute myelogenous leukemia patients undergoing chemotherapy: a randomized controlled trial. J Pain Symptom Manage. 2008;35(5):524-34.
5. Liu RD, Chinapaw MJ, Huijgens PC, Van mechelen W. Physical exercise interventions in haematological cancer patients, feasible to conduct but effectiveness to be established: a systematic literature review. Cancer Treat Rev. 2009;35(2):185-92.
Resources
[edit | edit source]
References[edit | edit source]
see adding references tutorial.
- ↑ 1.0 1.1 1.2 1.3 National Cancer Institute. Adult Acute Myeloid Leukemia Treatment. National Cancer Institute at the National Institute of Health. December 26, 2013. Available at http://www.cancer.gov/cancertopics/pdq/treatment/adultAML/Patient/page1, Accessed March 11, 2014
- ↑ 2.0 2.1 2.2 2.3 2.4 Goodman CC, Fuller KS: Pathology: implications for the physical therapist, ed 3, Philadelphia, 2009, WB Saunders.
- ↑ Goodman C, Snyder T. Differential Diagnosis for Physical Therapists: Screening for Referral. Saunders, St. Louis, Missouri. 5th edition. 2013.
- ↑ American Cancer Society. Chemotherapy for acute myeloid leukemia. American Cancer Society. February 7, 2014. Available at http://www.cancer.org/cancer/leukemia-acutemyeloidaml/detailedguide/leukemia-acute-myeloid-myelogenous-treating-chemotherapy. Accessed March 17, 2014
- ↑ American Cancer Society. What are the risk factors for acute myeloid leukemia? American Cancer Society. February 7, 2014. Available at http://www.cancer.org/cancer/leukemia-acutemyeloidaml/detailedguide/leukemia-acute-myeloid-myelogenous-risk-factors. Accessed March 17, 2014
- ↑ Chang PH, Lai YH, Shun SC, et al. Effects of a walking intervention on fatigue-related experiences of hospitalized acute myelogenous leukemia patients undergoing chemotherapy: a randomized controlled trial. J Pain Symptom Manage. 2008;35(5):524-34.
- ↑ Battaglini CL, Hackney AC, Garcia R, Groff D, Evans E, Shea T. The effects of an exercise program in leukemia patients. Integr Cancer Ther. 2009;8(2):130-8.
- ↑ Breastcancer.org. Exercise during and after chemotherapy or targeted therapies. Breastcancer.org. January 26, 2014. Available at http://www.breastcancer.org/tips/exercise/treatment/chemo_targeted. Accessed March 25, 2014
- ↑ Seiter K. Acute Myelogenous Leukemia Differential Diagnosis. Medscape. http://emedicine.medscape.com/article/197802-differential. March 9, 2012. Accessed March 18, 2014.