Acromioclavicular Joint Disorders
Original Editors - Mathilde De Dobbeleer
Top Contributors - Mostafa Mataich, Kim Jackson, Mathilde De Dobbeleer, Scott Cornish, Ilona Malkauskaite, Lien Hennebel, Admin, Yuli-Karisma Borremans, Rachael Lowe, WikiSysop, 127.0.0.1, Fasuba Ayobami, Simisola Ajeyalemi, Vidya Acharya, Borms Killian, Wanda van Niekerk, Venus Pagare, George Prudden, Kai A. Sigel, Tony Lowe, Oyemi Sillo, Amanda Ager, Naomi O'Reilly, Lucinda hampton, Olajumoke Ogunleye and Tarina van der Stockt - Killian Borms, Haytem Mkichri, Anna Jansma, Yassin Khomsi.
Search Strategy
[edit | edit source]
We searched for information in search engines such as Pubmed and Google Scholar, Pedro and the Cochrane Library.
We used keywords “acromioclavicular joint injuries”, “disorders”, “rehabilitation”, “conservative care”.
We gave priority to Randomised Controlled Trials.
Cochrane Library: 65 references
Pedro: 3 references (systematic revieuws)
Pubmed: 24 RCTs (5 free)
Definition/Description[edit | edit source]
The term 'disorders' is a very generalized term and includes several aspects. It can be caused by a trauma (for example joint dislocation) of the acromioclavicular joint or some degenerative conditions (for example osteoarthritis).[1] An acromioclavicular dislocation is a traumatic dislocation of the acromioclavicular joint in which a displacement of the clavicle occurs relative to the shoulder.[2]
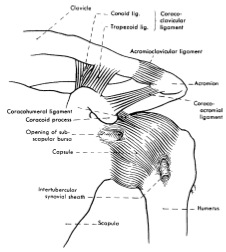
The acromioclavicular joint is a diarthrodial joint that connect the clavicle with the acromion, it has an intra-articular synovium and an articular cartilage interface[3]. It is characterized by the various angles of inclination in the sagittal and coronal planes and by a discus. In anatomical studies, De Palma [4] and Salter et al. [5] observed two types of disk: a complete disk (very rare) and a meniscoid-like disk. The acromioclavicular joint is surrounded by a capsule and the anterior/posterior AC joints and the superior/inferior AC joints. Also the coracoclavicular ligaments (trapezoid and conoid) are important for the stabilization.[6]
Clinically Relevant Anatomy[edit | edit source]
The acromioclavicular joint is a diarthrodial joint with an interposed fibrocartilagninous meniscal disk that connect the clavicle with the acromion. It is characterized by the various angles of inclination in the sagittal and coronal planes and by a discus. The acromioclavicular joint is surrounded by a capsule and the anterior/posterior AC joints and the superior/inferior AC joints. Also the coracoclavicular ligaments (trapezoid and conoid) are important for the stabilization.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
The acromioclavicular (AC) ligament and coracoclavicular (CC) ligaments are part of the statoc stabilisers of the joint. The AC ligament controls horizontal stability in the anteriorposterior plane. The CC ligaments (conoid and trapezoid ligaments) serves to control the vertical stability. The conoid portion of this ligament attaches posterior and medial on the clavicle while the trapezoid portion attaches anterior and lateral. The trapezius and deltoid muscles have also been shown to function as dynamic stabilizers of the AC joint.[7]
Epidemiology /Etiology[edit | edit source]
Injuries to the AC-joint account for 9% to 10% of acute injuries to the shoulder girdle. Seperations of the AC-joint account for 40% of shoulder girdle injuries in athletes. Common injury happens when they include falls on an outstretched hand or elbow, direct blows to the shoulder, or falling onto the point of the shoulder.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
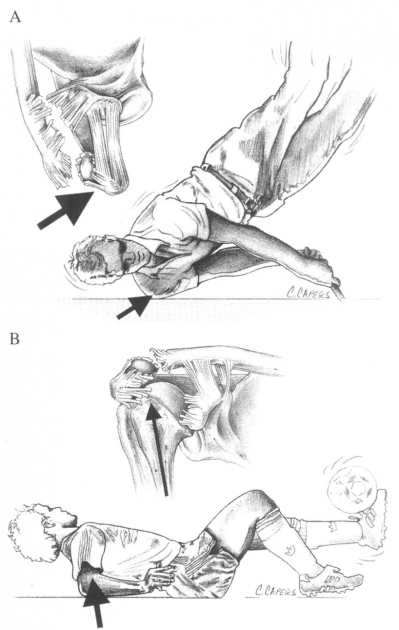
In figure 2 below we can see the common mechanism of in jury:
(A) is from a direct force onto the point of the shoulder
(B) Indirect forces to the AC joint can also cause injury. For example ,a fall on to the elbow can drive the humerus proximally, thus disrupting the AC joint. In this case, the strain is referred only to the AC ligaments and not the coracoclavicular ligaments.[6]
The injury frequently frequently to hockey players and rugby players, but they also happen in alpine skiing, snowboarding, football, bicycling and motor vehicle accidents. [8][9]
Characteristics/Clinical Presentation[edit | edit source]
People who sustain an AC joint injury may complain of pain radiating to their neck and deltoid.The AC joint may also be swollen, the upper extremity often held in adduction with the acromion depressed which may cause the clavicle to be elevated.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
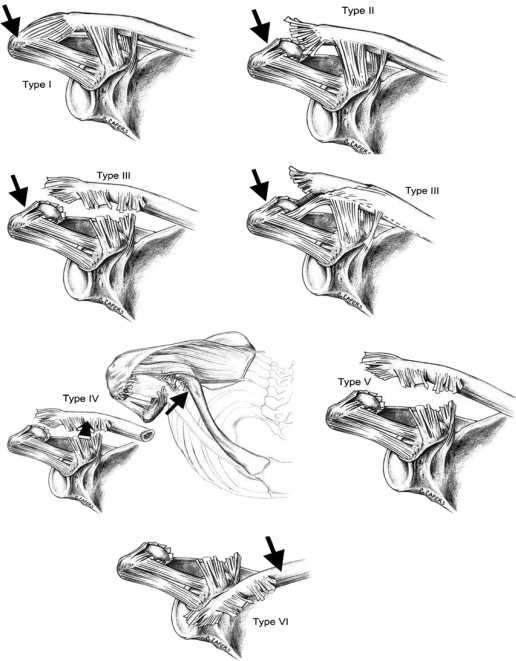
Allman, Tossy and colleagues described a three-grade classification. Rockwood and Green expanded this to a six grade classification model (known as the Rockwood grades). This classification of AC joint injuries is important to understand as it helps dictate treatment options and helps to avoid complications by failure to recognize the pattern of injury. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
| Grade |
Description |
Observation/Testing |
|---|---|---|
| I |
Sprain of AC ligaments. The AC and CC ligaments are intact |
No instability of clavicle detected on stress tests |
| II |
AC ligaments are ruptured, CC ligaments are intact. Often described as a subluxation. |
Clavicle is unstable to direct stress tests |
| III |
Complete disruption of both the AC and CC ligaments without significant disruption of the delto-trapezial fascia. This is often described as a dislocation. |
Deformity present with clavicle appearing elevated (acromion depressed), clavicle unstable in both vertical and horizontal plane |
| IV |
Distal clavicle is posteriorly displaced into trapezius muscle |
Posterior deformity present. |
| V |
More severe form of grade III. Complete disruption of both the AC and CC ligaments with disruption of the delto- trapezial fascia. |
Pseudo lateral clavicle elevation, downward displacement of the scapular. |
| VI |
Inferior displacement of the distal clavicle, either subacrominal or subcoracoid |
Severe trauma, usually accompanied by other significant injuries. |
A study reported that using a digital measurment instead of a sole visual diagnosis is recomended because of the higher intra- and interobserver reliability.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Differential Diagnosis[edit | edit source]
- Most dislocations are situated in the Glenohumeral Joint and 90% of this dislocations are anterior what can cause some concomitant pathologies such as a Hill sachs lesion, injury of the brachial plexus...[10]
- Pain in the AC joint from osteoarthritis or disc diseaseCite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - Osteolysis of the distal clavicle Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - Instability of the AC joint Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - Rotator-cuff impingement or tear Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - Adhesive capsulitis Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - Thoracic outlet syndrome Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - Superior labral tears Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - Complex pain syndrome Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - Shoulder dislocation Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - Anterior humerus subluxation Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title
Diagnostic Procedures[edit | edit source]
- The diagnosis of acromioclavicular dislocation is often made after taken radiography. Only a problem occurs with patients suffering from a type I dislocation, because on a radiography we can’t see anything out of the ordinary. These patients are therefore diagnosed by the mechanism of injury and tenderness over the AC joint.[11]
Outcome Measures[edit | edit source]
- DASH: Disabilities of the Arm, Shoulder and Hand questionnaires.Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title
- Simple Shoulder Test questionnaires: Purpose is to assess functional disability of the shoulder. Total score of 12 items : 2 about function related to pain; 7 about function/ strength and 3 about range of motion Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title
- Shoulder Pain and Disability Index (SPADI): The primary outcome measure is the patients’ perceived level of pain and disability. It consists of 2 subscales, pain and disability, which are combined to produce a total score ranging from 0 (no pain or functional difficulty) to 100 (highest level of pain and functional difficulty). The SPADI is reliable, valid, and responsive for shoulder pain of musculoskeletal, neurogenic, or undetermined origin. Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title
- American Shoulder Elbow Surgeon (ASES) : Is an instrument that measures functional limitations and pain in people with musculoskeletal shoulder pathologies. The function score is calculated from the sum of 10 questions questioning function using a 4-point ordinal scale.Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title
Examination[edit | edit source]
- O’brien test: Examination using the O’Briens test tightens the posterior capsule and posteriorly translates the humeral head, stressing the labrum resulting in pain and weakness.
- Paxinos sign: Provocative testing for acromioclavicualr joint injuryCite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title Cite error: Invalid<ref>tag; name cannot be a simple integer. Use a descriptive title. A prospective study of Walton and colleagues found out that the Paxinos test is a good clinical diagnostic tool, and bone-scanning is the best imaging modality for the diagnosis of acromioclavicular joint pain. When both of these tests are positive in a patient with shoulder pain, we have high degree of confidence for the diagnosis of acromioclavicular joint painCite error: Invalid<ref>tag; name cannot be a simple integer. Use a descriptive title. - Test of Stenvers 4: Clavicular Roll
- Resisted AC Joint Extension Test
To differ type I from type II, we must check the mechanism of injury and feel the tenderness over the AC joint. If there is a slight deformity present in the AC joint, chances are high it is a type II injury. In a type I injury, there is swelling present and especially pain in abduction of the arm. In Type II the patient has pain with every movement he makes with the arm. If there is a type III injury it is quite clear there is an obvious deformity of the AC joint and the patient will support his injured arm as close as possible to his body.[12]
Medical Management
[edit | edit source]
The treatment of injuries of the AC joint will vary depending on the severity or degree of the injury. The first treatment that is best used is ice application within 24 hours to 48 hours and anti-inflammatories. Also used is a atella that is tied to the shoulder, but a high quality atella should be used which unable the patient to use arm holding the arm against the abdomen(add illustration), this will provide a temporary but strict immobilization. Nonoperative treatment is recommended for type I and type II AC separations. In this treatment anti-inflammatory medications and ice application and the use of a sling for comfort are used. Depending on the type the treatment will last for 1 week or 2 weeks. If it is type I it will last 1 week and if it is type II it will last for 2 weeks. For the treatment of type III injury there is a lot of discussion, the treatment with the best results is nonoperative treatment. In this case the same treatment of type I and type II will just last longer, it may extend to 3 to 4 weeks. A surgical treatment is possible but is not so much recommended. For type IV and type V a surgical method has shown better results and is highly recommended.
There are several methods for treating a severe dislocation of the AC joint with a surgery. There are more than 75 methods, but the 4 most common surgical options are (1) AC joint fixation, hook-plates are very popular to fixate the AC joint, (2) coracoacromial ligament transfer, (3) coracoclaviculair interval fixation and (4) a coracoclaviculair ligament reconstruction.[13][14]
Physical Therapy Management
[edit | edit source]
Non-operative type I and II
Non-operative treatment is recommended for type I and Type II AC separations. Treatment typically includes the use of a simple sling for comfort in addition to icing and NSAID for pain relief. The sling is used until the pain subsides. Usually 1 week for type I injuries and 2 to 3 weeks for type 2 injuries.
Once the pain resolves, a physical therapy program is initiated with passive and active ROM exercise. Once full ROM is restored, patients begin strengthening exercises. Return to athletics is delayed until full, painless ROM is achieved. Normally 2 weeks for Type I and 2 to 3 weeks for Type II.[15]
Post-operative Type III - VI</u
Almost every case of type III-VI is treated surgically. This is the therapy that follows the surgical therapy(note that here is a lot of controversy about this topic):
<u>Post-operative therapy Hook plate
Postoperatively , the arm is immobilized in a sling for 4 weeks. The patients are instructed not to do tasks that will bring their arm above their head. During this time, the patient engages in physical therapy, including passive motion twice a week. After 4 weeks, the patient is allowed to elevate and abduct the arm actively to a level of 90°. The plate is removed after 12 weeks.[16]
The treatment is almost the same as Type I and II injuries but the duration of the sling is longer, 3 to 4 weeks. The therapy always consist initially ROM exercises, followed by progressive strengthening. Rehabilitations protocols should be followed diligently because inadequate rehabilitation can be a source of persistent pain and instability of the AC joint.[17][18]
Studies comparing the results of non-operative and surgical treatment of type III AC separations have shown that surgical interventions do not have a substantial benefit. In a RCT patients with type III AC injuries whom were treated non-operatively obtained full shoulder motion more quickly.[19]
For type IV and V injuries there is no evidence based literature recommending a specific treatment for these injuries. With surgery being the preferred treatment, there is one treatment that reported the successful use of manual reductions. With manual reduction the injuries were converted to a type II injury.[20]
Key Research[edit | edit source]
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
1. Gloria M. Beim, MD, ‘Acromioclavicular joint injuries’, Journal of Athletic Training, 2000, p.261- 267
<span style="line-height: 1.5em;" />
2. A Lizaur, L Marco, R cebrian,’Acute dislocation of the arcomioclavicular joint’, Journal of Bone and Joint Surgery, 1994, p.602-606
3. K Takase, K Yamamoto, A Imakiire, ‘Therapeutic result of acromioclavicular joint dislocation complicated by rotator cuff tear’, Journal of Orthopaedic Surgery, 2004, p.96-101
4. Cem Zeki ESENYEL, Kahraman ÖZTÜRK, etal., ‘Coracoclavicular ligament repair and screw fixation in acromioclavicular dislocations’, Acta Orthop Traumatol Turc, 2009, p.194 -198
5. Acromioclavicular Joint Injuries by Upender Satelli
Clinical Bottom Line[edit | edit source]
add text here
Recent Related Research (from Pubmed)[edit | edit source]
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
Kraeutler MJ, Williams GR Jr, Cohen SB, Ciccotti MG, Tucker BS, Dines JS, Altchek DW, Dodson CC. Inter- and intraobserver reliability of the radiographic diagnosis and treatment of acromioclavicular joint separations. Orthopedics. 2012;35(10) p.1483-1487
Verdano MA, Pellegrini A, Zanelli M, Paterlini M, Ceccarelli F. Modified Phemister procedure for the surgical treatment of Rockwood types III, IV, V acute acromioclavicular joint dislocation. Musculoskelet Surg. 2012;96(3) p.213-222
References
[edit | edit source]
- ↑ 1. J. Codsi, M.,' the painful shoulder: when to inject and when to refer', Cleveland clinic journal of medicine, VOL. 74 (2007), July, nr7, p.473-482 (level of evidence 1A)
- ↑ 2. Ewout Heijmans, Just Eekhof, Arie Knuistingh Neven, Acromioclaviculaire luxatie, huisarts &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; wetenschap, november 2010(level of evidence 1A)
- ↑ Saccomanno MF. Acromioclavicular joint instability: anatomy, biomechanics and evaluation. Joints 2014; 2(2): 87–92.
- ↑ De Palma AF. Surgical anatomy of the acromioclavicular and sternoclavicular joints. Surg Clin North Am. 1963;43:1541–1550.
- ↑ Salter EG, Jr, Nasca RJ, Shelley BS. Anatomical observations on the acromioclavicular joint in supporting ligaments. Am J Sports Med 1987;15(3):199-206.
- ↑ 6.0 6.1 Beim GM. Acromioclavicular joint injuries. Journal of Athletic Training 2000;35(3):261-267.
- ↑ Suezie K, Blank A, Strauss E. Management of Type 3 Acromioclavicular Joint Dislocations Current Controversies. Bulletin of the Hospital for Joint Diseases 2014; 72(1): 5360. [Level of evidence 4]
- ↑ Johansen JA, Grutter PW, McFarland EG, Petersen SA. Acromioclavicular joint injuries: indications for treatment and treatment options. J Shoulder Elbow Surg 2011;20:70-82.
- ↑ Culp LB, Romani WA. Physical Therapist Examination, Evaluation, and Intervention Following the Surgical Reconstruction of a Grade III Acromioclavicular Joint Separation. Journal of the American physical therapy association 2006; 86:857-869.(level of evidence 3B)
- ↑ 7. V. Nepola, J., E. Newhouse, K., 'Recurrent shoulder dislocation', The iowa orthopaedic journal, VOL. 13 (1993), p. 97-106 (level of evidence 2A)
- ↑ 4. Johansen JA, Grutter PW, McFarland EG, Petersen SA. Acromioclavicular joint injuries: indications for treatment and treatment options. J Shoulder Elbow Surg. 2011;20 p.S70-82 (level of evidence 2A)
- ↑ Culp LB, Romani W. Physical Therapist Examination, Evaluation, and Intervention Following the Surgical Reconstruction of a Grade III Acromioclavicular Joint Separation. Journal of the American physical therapy association 2006; 86:857-869.( level of evidence 3B)
- ↑ 4. Johansen JA, Grutter PW, McFarland EG, Petersen SA. Acromioclavicular joint injuries: indications for treatment and treatment options. J Shoulder Elbow Surg. 2011;20 p.S70-82 (level of evidence 2A)
- ↑ 9. Jennifer M. Hootman. Acromioclavicular Dislocation: Conservative or Surgical Therapy. Athl Train. 2004; 39(1). p 10–11. (level of evidence 2A)
- ↑ 9. Jennifer M. Hootman. Acromioclavicular Dislocation: Conservative or Surgical Therapy. Athl Train. 2004; 39(1). p 10–11. (level of evidence 2A)
- ↑ 10. Gstettner C, Tauber M, Hitzl W, Resch H. Rockwood type III acromioclavicular dislocation: surgical versus conservative treatment. J Shoulder Elbow Surg. 2008;17(2), p.220-225. (level of evidence 2A)
- ↑ 4. Johansen JA, Grutter PW, McFarland EG, Petersen SA. Acromioclavicular joint injuries: indications for treatment and treatment options. J Shoulder Elbow Surg. 2011;20 p.S70-82 (level of evidence 2A)
- ↑ 12. Glick JM, Milburn LJ, Haggerty JF, Nishimoto D. Dislocated acromioclavicular joint: follow-up study of 35 unreduced acromioclavicular dislocations. Am J Sports Med 1977;5:264-70. doi:10.1177/ 036354657700500614 fckLR(hyperlink: http://www.deepdyve.com/lp/sage/dislocated-acromioclavicular-joint-follow-up-study-of-35-unreduced-68pKcCF6qC )
- ↑ 11. Bannister GC, Wallace WA, Stableforth PG, Hutson MA.The management of acute acromioclavicular dislocation. A randomised prospective controlled trial. Bone Joint Surg Br. 1989;71(5)p.848-850. (level of evidence 1B)
- ↑ 4. Johansen JA, Grutter PW, McFarland EG, Petersen SA. Acromioclavicular joint injuries: indications for treatment and treatment options. J Shoulder Elbow Surg. 2011;20 p.S70-82 (level of evidence 2A)
- ↑ Dr. Nabil Ebraheim. SHOULDER SEPARATION /AC JOINT - Everything You Need To Know. Available from: https://www.youtube.com/watch?v=OfcSvG-dgbY [last accessed 28/3/15]
- ↑ Fergus Tilt. How To Best Test for an AC Joint Injury. Available from: https://www.youtube.com/watch?v=BAkmLrOOihk [last accessed 28/3/15]
- ↑ KT Tape. KT Tape: AC Joint. Available from: https://www.youtube.com/watch?v=DJEhxOkg8Pg [last accessed 28/3/15]