Acromioclavicular Joint Disorders: Difference between revisions
No edit summary |
No edit summary |
||
| Line 10: | Line 10: | ||
== <span style="line-height: 1.5em;">Definition/Description</span> == | == <span style="line-height: 1.5em;">Definition/Description</span> == | ||
The term 'disorders' is a very generalized term and includes several aspects. It can be caused by a trauma (for example joint dislocation) of the [[Acromioclavicular Joint|acromioclavicular joint]] or some degenerative conditions (for example [[Osteoarthritis|osteoarthritis]]).<ref>1. J. Codsi, M.,' the painful shoulder: when to inject and when to refer', Cleveland clinic journal of medicine, VOL. 74 (2007), July, nr7, p.473-482 (level of evidence 1A)</ref> An acromioclavicular dislocation is a traumatic dislocation of the acromioclavicular joint in which a displacement of the clavicle occurs relative to the shoulder.<ref>2. Ewout Heijmans, Just Eekhof, Arie Knuistingh Neven, Acromioclaviculaire luxatie, huisarts &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; wetenschap, november 2010(level of evidence 1A)</ref><br> | The term 'disorders' is a very generalized term and includes several aspects. It can be caused by a trauma (for example joint dislocation) of the [[Acromioclavicular Joint|acromioclavicular joint]] or some degenerative conditions (for example [[Osteoarthritis|osteoarthritis]]).<ref>1. J. Codsi, M.,' the painful shoulder: when to inject and when to refer', Cleveland clinic journal of medicine, VOL. 74 (2007), July, nr7, p.473-482 (level of evidence 1A)</ref> An acromioclavicular dislocation is a traumatic dislocation of the acromioclavicular joint in which a displacement of the clavicle occurs relative to the shoulder.<ref>2. Ewout Heijmans, Just Eekhof, Arie Knuistingh Neven, Acromioclaviculaire luxatie, huisarts &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; wetenschap, november 2010(level of evidence 1A)</ref><br> | ||
The acromioclavicular joint is a diarthrodial joint that connect the clavicle with the acromion, it has an intra-articular synovium and an articular cartilage interface<ref>Saccomanno MF. Acromioclavicular joint instability: anatomy, biomechanics and evaluation. Joints 2014; 2(2): 87–92.</ref>. It is characterized by the various angles of inclination in the sagittal and coronal planes and by a discus. In anatomical studies, De Palma <ref>De Palma AF. Surgical anatomy of the acromioclavicular and sternoclavicular joints. Surg Clin North Am. 1963;43:1541–1550.</ref> and Salter et al. <ref>Salter EG, Jr, Nasca RJ, Shelley BS. Anatomical observations on the acromioclavicular joint in supporting ligaments. Am J Sports Med 1987;15(3):199-206.</ref> observed two types of disk: a complete disk (very rare) and a meniscoid-like disk. The acromioclavicular joint is surrounded by a capsule and the anterior/posterior AC joints and the superior/inferior AC joints. Also the coracoclavicular ligaments (trapezoid and conoid) are important for the stabilization.<ref name="Beim">Beim GM. Acromioclavicular joint injuries. Journal of Athletic Training 2000;35(3):261-267.</ref><br> | |||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
Revision as of 17:49, 9 October 2016
Original Editors - Mathilde De Dobbeleer
Top Contributors - Mostafa Mataich, Kim Jackson, Mathilde De Dobbeleer, Scott Cornish, Ilona Malkauskaite, Lien Hennebel, Admin, Yuli-Karisma Borremans, Rachael Lowe, Kai A. Sigel, WikiSysop, 127.0.0.1, Fasuba Ayobami, Simisola Ajeyalemi, Vidya Acharya, Borms Killian, Wanda van Niekerk, Venus Pagare, George Prudden, Tony Lowe, Oyemi Sillo, Amanda Ager, Naomi O'Reilly, Lucinda hampton, Olajumoke Ogunleye and Tarina van der Stockt - Killian Borms, Haytem Mkichri, Anna Jansma, Yassin Khomsi.
Search Strategy
[edit | edit source]
We searched for information in search engines such as Pubmed and Google Scholar, Pedro and the Cochrane Library.
We used keywords “acromioclavicular joint injuries”, “disorders”, “rehabilitation”, “conservative care”.
We gave priority to Randomised Controlled Trials.
Cochrane Library: 65 references
Pedro: 3 references (systematic revieuws)
Pubmed: 24 RCTs (5 free)
Definition/Description[edit | edit source]
The term 'disorders' is a very generalized term and includes several aspects. It can be caused by a trauma (for example joint dislocation) of the acromioclavicular joint or some degenerative conditions (for example osteoarthritis).[1] An acromioclavicular dislocation is a traumatic dislocation of the acromioclavicular joint in which a displacement of the clavicle occurs relative to the shoulder.[2]
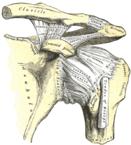
The acromioclavicular joint is a diarthrodial joint that connect the clavicle with the acromion, it has an intra-articular synovium and an articular cartilage interface[3]. It is characterized by the various angles of inclination in the sagittal and coronal planes and by a discus. In anatomical studies, De Palma [4] and Salter et al. [5] observed two types of disk: a complete disk (very rare) and a meniscoid-like disk. The acromioclavicular joint is surrounded by a capsule and the anterior/posterior AC joints and the superior/inferior AC joints. Also the coracoclavicular ligaments (trapezoid and conoid) are important for the stabilization.[6]
Clinically Relevant Anatomy[edit | edit source]
The acromioclavicular joint is a diarthrodial joint that connect the clavicle with the acromion. It is characterized by the various angles of inclination in the sagittal and coronal planes and by a discus. The acromioclavicular joint is surrounded by a capsule and the anterior/posterior AC joints and the superior/inferior AC joints. Also the coracoclavicular ligaments (trapezoid and conoid) are important for the stabilization.[7]
Epidemiology /Etiology[edit | edit source]
Injuries to the acromioclavicular (AC) joint are common, representing about 9% of all shoulder injuries and are even more common in athletes. These injuries often occur as a result of a traumatic lateral blow, due to running into someone, tackling or fall on the shoulder with the arm in some degree of adduction. They are the third most common injury seen in college hockey players and account for 41% of all shoulder injuries seen in elite college rugby players, but they also happen in alpine skiing, snowboarding, football, bicycling and motor vehicle accidents.[8][9][10]
Characteristics/Clinical Presentation[edit | edit source]
AC joint injuries often occur when falling on the shoulder, collision with another player or while being tackled. During the fall the shoulder will hit the ground and the scapulae will be pushed down. The clavicle can only partially follow this movement and there will be a great deal of strain on the ligaments causing them to rupture or dislocate.The acromioclavicular joint injuries are divided into three groups, this classification is the most common:
- Type I: In a type I is a partial injury to the joint capsule. Paired whit an incomplete tear of the acromioclavicular ligaments and joint capsule.
- Type II: A type II injury is a moderate injury. A partial tear of the ligament coracoclavicular (ligament between coracoideus and clavicle) with a rupture of the capsule and the acromioclavicular ligament. Often described as a subluxation.
- Type III: A type III injury is a severe injury. Complete rupture of the acromioclavicular ligament but also the coracoclavicular ligament. This can lead to displacement of the clavicle and are therefore very unstable.
This is often described as a dislocation.
Type III dislocation problems, which are very complex and therefore further divided into 3.
- Type IV: Dislocation with posterior dislocation of the clavicle.
- Type V: Dislocation whit severe upward displacement of the clavicle into or through the Trapezius.
- Type VI: This is a rare injury. Dislocation of the clavicle inferiorly, locked under the coracoids process.
Rockwood classification.[11]
Differential Diagnosis[edit | edit source]
Most dislocations are situated in the Glenohumeral Joint and 90% of this dislocations are anterior what can cause some concomitant pathologies such as a Hill sachs lesion, injury of the brachial plexus...[12]
Diagnostic Procedures[edit | edit source]
The diagnosis of acromioclavicular dislocation is often made after taken radiography. Only a problem occurs with patients suffering from a type I dislocation, because on a radiography we can’t see anything out of the ordinary. These patients are therefore diagnosed by the mechanism of injury and tenderness over the AC joint.[13]
Outcome Measures[edit | edit source]
Outcome measures which are used are the Disabilities of the Arm, Shoulder and Hand and Simple Shoulder Test questionnaires.[14]
Examination[edit | edit source]
Most common complaints are often pain, numbness and swelling in the AC joint. In type I lesions swelling and pain are the most common, especially in the abduction of the arm.
In type II injuries we find a moderate (45 to 74 mm) to severe pain(75 to 100 pain scale).[15] In both cases, the movement of the affected limp is very restricted due to the pain. In type III injuries we find the same symptoms, but in addition also very pronounced deformations can occur. In these types the clavicle moves out of the normal range. The displacement of the clavicle can better be seen in adduction of both arms. Also the different shoulder movements will be greatly reduced. We can try to differ the different types of pathologies by examining the shoulder of the patients. To differ type I from type II, we must check the mechanism of injury and feel the tenderness over the AC joint. If there is a slight deformity present in the AC joint, chances are high it is a type II injury. In a type I injury, there is swelling present and especially pain in abduction of the arm. In Type II the patient has pain with every movement he makes with the arm. If there is a type III injury it is quite clear there is an obvious deformity of the AC joint and the patient will support his injured arm as close as possible to his body.[16]
Medical Management
[edit | edit source]
The treatment of injuries of the AC joint will vary depending on the severity or degree of the injury. The first treatment that is best used is ice application within 24 hours to 48 hours and anti-inflammatories. Also used is a atella that is tied to the shoulder, but a high quality atella should be used which unable the patient to use arm holding the arm against the abdomen(add illustration), this will provide a temporary but strict immobilization. Nonoperative treatment is recommended for type I and type II AC separations. In this treatment anti-inflammatory medications and ice application and the use of a sling for comfort are used. Depending on the type the treatment will last for 1 week or 2 weeks. If it is type I it will last 1 week and if it is type II it will last for 2 weeks. For the treatment of type III injury there is a lot of discussion, the treatment with the best results is nonoperative treatment. In this case the same treatment of type I and type II will just last longer, it may extend to 3 to 4 weeks. A surgical treatment is possible but is not so much recommended. For type IV and type V a surgical method has shown better results and is highly recommended.
There are several methods for treating a severe dislocation of the AC joint with a surgery. There are more than 75 methods, but the 4 most common surgical options are (1) AC joint fixation, hook-plates are very popular to fixate the AC joint, (2) coracoacromial ligament transfer, (3) coracoclaviculair interval fixation and (4) a coracoclaviculair ligament reconstruction.[17][18]
Physical Therapy Management
[edit | edit source]
Non-operative type I and II
Non-operative treatment is recommended for type I and Type II AC separations. Treatment typically includes the use of a simple sling for comfort in addition to icing and NSAID for pain relief. The sling is used until the pain subsides. Usually 1 week for type I injuries and 2 to 3 weeks for type 2 injuries.
Once the pain resolves, a physical therapy program is initiated with passive and active ROM exercise. Once full ROM is restored, patients begin strengthening exercises. Return to athletics is delayed until full, painless ROM is achieved. Normally 2 weeks for Type I and 2 to 3 weeks for Type II.[19]
Post-operative Type III - VI</u
Almost every case of type III-VI is treated surgically. This is the therapy that follows the surgical therapy(note that here is a lot of controversy about this topic):
<u>Post-operative therapy Hook plate
Postoperatively , the arm is immobilized in a sling for 4 weeks. The patients are instructed not to do tasks that will bring their arm above their head. During this time, the patient engages in physical therapy, including passive motion twice a week. After 4 weeks, the patient is allowed to elevate and abduct the arm actively to a level of 90°. The plate is removed after 12 weeks.[20]
The treatment is almost the same as Type I and II injuries but the duration of the sling is longer, 3 to 4 weeks. The therapy always consist initially ROM exercises, followed by progressive strengthening. Rehabilitations protocols should be followed diligently because inadequate rehabilitation can be a source of persistent pain and instability of the AC joint.[21][22]
Studies comparing the results of non-operative and surgical treatment of type III AC separations have shown that surgical interventions do not have a substantial benefit. In a RCT patients with type III AC injuries whom were treated non-operatively obtained full shoulder motion more quickly.[23]
For type IV and V injuries there is no evidence based literature recommending a specific treatment for these injuries. With surgery being the preferred treatment, there is one treatment that reported the successful use of manual reductions. With manual reduction the injuries were converted to a type II injury.[24]
Key Research[edit | edit source]
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
1. Gloria M. Beim, MD, ‘Acromioclavicular joint injuries’, Journal of Athletic Training, 2000, p.261- 267
<span style="line-height: 1.5em;" />
2. A Lizaur, L Marco, R cebrian,’Acute dislocation of the arcomioclavicular joint’, Journal of Bone and Joint Surgery, 1994, p.602-606
3. K Takase, K Yamamoto, A Imakiire, ‘Therapeutic result of acromioclavicular joint dislocation complicated by rotator cuff tear’, Journal of Orthopaedic Surgery, 2004, p.96-101
4. Cem Zeki ESENYEL, Kahraman ÖZTÜRK, etal., ‘Coracoclavicular ligament repair and screw fixation in acromioclavicular dislocations’, Acta Orthop Traumatol Turc, 2009, p.194 -198
5. Acromioclavicular Joint Injuries by Upender Satelli
Clinical Bottom Line[edit | edit source]
add text here
Recent Related Research (from Pubmed)[edit | edit source]
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
Kraeutler MJ, Williams GR Jr, Cohen SB, Ciccotti MG, Tucker BS, Dines JS, Altchek DW, Dodson CC. Inter- and intraobserver reliability of the radiographic diagnosis and treatment of acromioclavicular joint separations. Orthopedics. 2012;35(10) p.1483-1487
Verdano MA, Pellegrini A, Zanelli M, Paterlini M, Ceccarelli F. Modified Phemister procedure for the surgical treatment of Rockwood types III, IV, V acute acromioclavicular joint dislocation. Musculoskelet Surg. 2012;96(3) p.213-222
References
[edit | edit source]
- ↑ 1. J. Codsi, M.,' the painful shoulder: when to inject and when to refer', Cleveland clinic journal of medicine, VOL. 74 (2007), July, nr7, p.473-482 (level of evidence 1A)
- ↑ 2. Ewout Heijmans, Just Eekhof, Arie Knuistingh Neven, Acromioclaviculaire luxatie, huisarts &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; wetenschap, november 2010(level of evidence 1A)
- ↑ Saccomanno MF. Acromioclavicular joint instability: anatomy, biomechanics and evaluation. Joints 2014; 2(2): 87–92.
- ↑ De Palma AF. Surgical anatomy of the acromioclavicular and sternoclavicular joints. Surg Clin North Am. 1963;43:1541–1550.
- ↑ Salter EG, Jr, Nasca RJ, Shelley BS. Anatomical observations on the acromioclavicular joint in supporting ligaments. Am J Sports Med 1987;15(3):199-206.
- ↑ Beim GM. Acromioclavicular joint injuries. Journal of Athletic Training 2000;35(3):261-267.
- ↑ 3. Gloria M. Beim, MD, ‘Acromioclavicular joint injuries’, Journal of Athletic Training, 2000, p.261- 267 (level of evidence 2A)
- ↑ 2. Ewout Heijmans, Just Eekhof, Arie Knuistingh Neven, Acromioclaviculaire luxatie, huisarts &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; wetenschap, november 2010(level of evidence 1A)
- ↑ 4. Johansen JA, Grutter PW, McFarland EG, Petersen SA. Acromioclavicular joint injuries: indications for treatment and treatment options. J Shoulder Elbow Surg. 2011;20 p.S70-82 (level of evidence 2A)
- ↑ 5. Lisa B Culp and William A Romani, Physical Therapist Examination, Evaluation, and Intervention Following the Surgical Reconstruction of a Grade III Acromioclavicular Joint Separation, journal of the American physical therapy association. 2006; 86:857-869.( level of evidence 3B)
- ↑ 6. Rockwood CA Jr, Young DC. Disorders of the acromioclavicular joint. In: Rockwood CA Jr, Matsen FA Hi, eds. The Shoulder. Philadelphia, PA: WB Saunders; 1990:413-476.
- ↑ 7. V. Nepola, J., E. Newhouse, K., 'Recurrent shoulder dislocation', The iowa orthopaedic journal, VOL. 13 (1993), p. 97-106 (level of evidence 2A)
- ↑ 4. Johansen JA, Grutter PW, McFarland EG, Petersen SA. Acromioclavicular joint injuries: indications for treatment and treatment options. J Shoulder Elbow Surg. 2011;20 p.S70-82 (level of evidence 2A)
- ↑ 8. Lizaur A, Sanz-Reig J, Gonzalez-Parreño S. Long-term results of the surgical treatment of type III acromioclavicular dislocations: an update of a previous report. J Bone Joint Surg Br. 2011;93(8)p.1088-1092 (level of evidence 3B)
- ↑ 13. Jensen MP, Chen C, Brugger AM., interpretation of visual analog scale ratings and change scores: a reanalysis of two clinical trials of postoperative pain , Journal of Pain, 4(7): 407 – 414 SEP 2003
- ↑ 5. Lisa B Culp and William A Romani, Physical Therapist Examination, Evaluation, and Intervention Following the Surgical Reconstruction of a Grade III Acromioclavicular Joint Separation, journal of the American physical therapy association. 2006; 86:857-869.( level of evidence 3B)
- ↑ 4. Johansen JA, Grutter PW, McFarland EG, Petersen SA. Acromioclavicular joint injuries: indications for treatment and treatment options. J Shoulder Elbow Surg. 2011;20 p.S70-82 (level of evidence 2A)
- ↑ 9. Jennifer M. Hootman. Acromioclavicular Dislocation: Conservative or Surgical Therapy. Athl Train. 2004; 39(1). p 10–11. (level of evidence 2A)
- ↑ 9. Jennifer M. Hootman. Acromioclavicular Dislocation: Conservative or Surgical Therapy. Athl Train. 2004; 39(1). p 10–11. (level of evidence 2A)
- ↑ 10. Gstettner C, Tauber M, Hitzl W, Resch H. Rockwood type III acromioclavicular dislocation: surgical versus conservative treatment. J Shoulder Elbow Surg. 2008;17(2), p.220-225. (level of evidence 2A)
- ↑ 4. Johansen JA, Grutter PW, McFarland EG, Petersen SA. Acromioclavicular joint injuries: indications for treatment and treatment options. J Shoulder Elbow Surg. 2011;20 p.S70-82 (level of evidence 2A)
- ↑ 12. Glick JM, Milburn LJ, Haggerty JF, Nishimoto D. Dislocated acromioclavicular joint: follow-up study of 35 unreduced acromioclavicular dislocations. Am J Sports Med 1977;5:264-70. doi:10.1177/ 036354657700500614 fckLR(hyperlink: http://www.deepdyve.com/lp/sage/dislocated-acromioclavicular-joint-follow-up-study-of-35-unreduced-68pKcCF6qC )
- ↑ 11. Bannister GC, Wallace WA, Stableforth PG, Hutson MA.The management of acute acromioclavicular dislocation. A randomised prospective controlled trial. Bone Joint Surg Br. 1989;71(5)p.848-850. (level of evidence 1B)
- ↑ 4. Johansen JA, Grutter PW, McFarland EG, Petersen SA. Acromioclavicular joint injuries: indications for treatment and treatment options. J Shoulder Elbow Surg. 2011;20 p.S70-82 (level of evidence 2A)
- ↑ Dr. Nabil Ebraheim. SHOULDER SEPARATION /AC JOINT - Everything You Need To Know. Available from: https://www.youtube.com/watch?v=OfcSvG-dgbY [last accessed 28/3/15]
- ↑ Fergus Tilt. How To Best Test for an AC Joint Injury. Available from: https://www.youtube.com/watch?v=BAkmLrOOihk [last accessed 28/3/15]
- ↑ KT Tape. KT Tape: AC Joint. Available from: https://www.youtube.com/watch?v=DJEhxOkg8Pg [last accessed 28/3/15]