Ventricular Extrasystole
Original Editor - Elyssa Abou Jamra
Top Contributors - Elyssa Abou Jamra, Kim Jackson and Lucinda hampton
Introduction[edit | edit source]
Premature ventricular contractions (PVCs) are early depolarizations of the myocardium originating in the ventricule. During a premature ventricular contraction (PVC), the heartbeat is initiated by the Purkinje fibers rather than the SA node. [1] [2]
- In the vast majority of cases, PVCs have no known cause and occur spontaneously. [1]
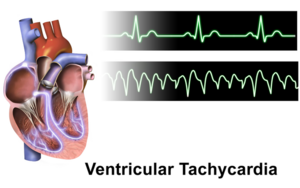
- The most common forms of premature ectopic ventricular impulse formation are ventricular extrasystoles and ventricular tachycardia. [3]The manifestation of the ectopic rhythm may be an expression of underlying disease. [4]
- Overall, the presence of PVCs in young people is a benign finding but in older patients with underlying heart disease, there is a risk of ventricular arrhythmias and cardiac arrest.[1]
Epidemiology[edit | edit source]
PVCs are common among the general population.
- The estimated prevalence ranges from 1% to 4% on electrocardiogram and 40% to 75% on a 24 or 48-hour Holter monitor.
- Young and healthy adults have shown a highly similar frequency rate of PVCs in contrast to the older segments of the general population[1].
Etiology[edit | edit source]
Common known etiologies include:
- Excess caffeine consumption, excess catecholamines (released in response to emotional or physical stress),[5] high levels of anxiety, and electrolyte abnormalities.
- Specific electrolyte:
- low blood potassium
- low blood magnesium
- high blood calcium.
- Alcohol, tobacco, and illicit drugs
- Patients suffering from sleep deprivation
- There are numerous cardiac and non-cardiac pathologies that are causative,examples:
- Any structural heart disease that alters conduction pathways due to tissue alterations
- Non-cardiac examples :
Patient populations with higher risks of cardiovascular disease and clinically poor cardiovascular markers have a higher occurrence of PVCs.[6]
Triggering Factors[edit | edit source]
- Stress
- dehydration,
- poor sleep,
- alcohol,
- medication
- health changes,
- stimulant or recreational drug use,
- temporal relationship between phases of hormonal cycles [7]
Pathophysiology[edit | edit source]
There are three mechanisms for the development of the disease: disruption of automatism, trigger activity, circular passage of the excitation wave (re-entry).
- Violation of automatism is carried out in the direction of increasing heart rate: due to the subthreshold potential of the pathological focal point located in the ventricles. Under the action of a normal rhythm, its transition to a threshold occurs, resulting in premature contraction. Characteristic of arrhythmias that develop from myocardial ischemia, electrolyte dysfunctions, and excess catecholamines.
- Trigger activity - is the emergence of an extraordinary pulse under the action of post-de-polarization, which is associated with the previous action potential. Characteristic of bradycardia, myocardial ischemia, electrolyte disorders, intoxication with certain drugs (for example, digitalis).
- The circular passage of the excitation wave (re-entry ) is formed at various organic disorders, when the myocardium becomes inhomogeneous, which prevents the normal passage of the impulse. In the area of scar or ischemia, areas with different conductive and restoring rates are formed. As a result, there appear both single ventricular extrasystoles and paroxysmal attacks of tachycardia.[8]
Assessment[edit | edit source]
History:
- Detailed history of the presenting symptom - including onset, duration, associated symptoms and recovery.
- Check for other cardiac symptoms including chest pain, breathlessness, syncope or near syncope (eg, dizziness), and arrhythmia symptoms (eg, sustained fast palpitations).
- If there is history of syncope, note that:
- Exertional syncope should always raise alarm of a sinister cause.
- Rapid recovery after the syncopal event, without confusion or drowsiness, is characteristic of cardiac syncope.
- Family history - for early cardiac disease or sudden death.
- Previous cardiac disease or coronary heart disease (CHD) risk factors.
Symptoms[edit | edit source]
Many patients are entirely asymptomatic, whereas other describe symptoms of:
- palpitations (heart pounding, irregular, skipped, or paused heartbeat)
or they may convey more generalized symptoms such as
- dizziness
- near-syncope
- dyspnea
- chest pain
- fatigue.
Symptoms can be due to the ventricular extrasystole itself, to the compensatory pause followed by a hypercontractile beat (Starling effect), or to a reduction in effective cardiac output .[7]
Examination
- Blood pressure
- Pulse
- Pulse oximetry
- Cardiac findings
- Cardiopulmonary findings
- Neurologic findings
Investigations
- Resting 12-lead ECG.
- FBC and TFTs.
- Electrolytes.
Other investigations:
- Serum calcium and magnesium.
- If symptoms have a long duration (many hours), advise the patient to attend their GP surgery or A&E for a 12-lead ECG during the next episode.
- Ambulatory ECG monitoring:
- If symptoms are short-lived but frequent (>2-3 times per week), use a 24-hour Holter monitor.
- If symptoms are short-lived and infrequent (<1 per week), use an event monitor or transtelephonic recorder.
- Echocardiography - to assess LV function and heart structure.
- Exercise stress testing - the relation of extrasystoles to exercise may have prognostic importance.
- Further non-invasive cardiac imaging may be required.[9]
Treatment[edit | edit source]
Patients with no symptoms/minor symptoms only - no heart disease, ventricular extrasystoles which reduce in frequency on exercise testing, and no documented ventricular tachycardia:
- These patients can be reassured.
- Reducing caffeine intake (if high) can be tried to see if this reduces symptoms.
- If treatment is desired, consider beta-blockers.
Patients with no heart disease, but with frequent ventricular extrasystoles (>1,000 per 24 hours):
- No treatment is required, but these patients may merit long-term follow-up, with periodic reassessment of LV function, particularly for those with very high-frequency extrasystoles.
Patients with no heart disease, with frequent unifocal ventricular extrasystoles and particularly if ventricular tachycardia or salvos are induced on exercise:
- Consider catheter ablation - this may be curative and results are often good.
Patients with cardiac disease:
- Ventricular extrasystoles may indicate either an arrhythmia risk or the severity of the underlying disease; therefore, consider the level of risk for sudden cardiac death.
- Beta-blockers may be indicated either for the underlying cardiac disease, or because they may reduce the frequency or symptoms of ventricular extrasystoles.
- Consider implantable cardiac defibrillators if at high risk of serious ventricular arrhythmia.
- Consider catheter ablation as adjunctive treatment.
Also treat any underlying cardiac disease and contributing factors - eg, hypertension, electrolyte abnormalities, ischaemia or cardiac failure.[10]
Summary[edit | edit source]
- Ventricular ectopic beats (PVCs) are frequently seen in daily clinical practice and are usually benign.
- Presence of heart disease should be sought and, if absent, indicates good prognosis in patients with PVCs.
- Unifocal PVCs arising from the right ventricular outflow tract are common and may increase with exercise and cause non-sustained or sustained ventricular tachycardia. Catheter ablation is effective and safe treatment for these patients.
- B-blockers may be used for symptom control in patients where PVCs arise from multiple sites. It should also be considered in patients with impaired ventricular systolic function and/or heart failure.
- Risk of sudden cardiac death from malignant ventricular arrhythmia should be considered in patients with heart disease who have frequent PVCs. An implantable cardioverter defibrillator may be indicated if risk stratification criteria are met.
- PVCs have also been shown to trigger malignant ventricular arrhythmias in certain patients with idiopathic ventricular fibrillation and other syndromes. Catheter ablation may be considered in some patients as adjunctive treatment.[12]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Farzam K, Richards JR. Premature Ventricular Contraction. StatPearls [Internet]. 2021 Aug 12. Available: https://www.ncbi.nlm.nih.gov/books/NBK532991/(accessed 28.2.2022)
- ↑ Ahn MS. Current Concepts of Premature Ventricular Contractions. J Lifestyle Med. 2013;3(1):26-33.
- ↑ Leo Schamroth (1980). Ventricular extrasystoles, ventricular tachycardia, and ventricular fibrillation: Clinical-electrocardiographic considerations. , 23(1), 13–32. doi:10.1016/0033-0620(80)90003-1
- ↑ Scherf D, Schott A: Extrasystoles and Allied Arrhythmias. London, William Heinemann, 1953
- ↑ Frigy, Attila; Csiki, Endre; Caraşca, Cosmin; Szabó, István Adorján; Moga, Victor-Dan (2018). Autonomic influences related to frequent ventricular premature beats in patients without structural heart disease. Medicine, 97(28), e11489–. doi:10.1097/MD.0000000000011489
- ↑ Ribeiro WN, Yamada AT, Grupi CJ, da Silva GT, Mansur AJ. Premature atrial and ventricular complexes in outpatients referred from a primary care facility. PLoS One. 2018;13(9):e0204246.
- ↑ 7.0 7.1 Gorenek, Bulent; Fisher, John D.; Kudaiberdieva, Gulmira; Baranchuk, Adrian; Burri, Haran; Campbell, Kristen Bova; Chung, Mina K.; Enriquez, Andrés; Heidbuchel, Hein; Kutyifa, Valentina; Krishnan, Kousik; Leclercq, Christophe; Ozcan, Emin Evren; Patton, Kristen K.; Shen, Win; Tisdale, James E.; Turagam, Mohit K.; Lakkireddy, Dhanunjaya (2019). Premature ventricular complexes: diagnostic and therapeutic considerations in clinical practice. Journal of Interventional Cardiac Electrophysiology, (), –. doi:10.1007/s10840-019-00655-3
- ↑ Arrhymia centre Ventricular extrasystoleshttps://arrhythmia.center/en/zheludochkovaya-ekstrasistoliya/ (accessed 28.2.2022)
- ↑ Robinson KJ, Sanchack KE; Palpitations. StatPearls Publishing 2019.
- ↑ (2015). 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. European Heart Journal, (), ehv316–. doi:10.1093/eurheartj/ehv316
- ↑ Alila Medical Media. Premature Ventricular Contractions (PVCs), Animation . Available from: https://www.youtube.com/watch?v=wBs4fowZmzs [last accessed 22/11/2021]
- ↑ Ng, G A. (2006). Treating patients with ventricular ectopic beats. Heart, 92(11), 1707–1712. doi:10.1136/hrt.2005.067843