Skier's thumb
Original Editors - Alicia Keefe and Brenna Rutledge as part of the Temple University EBP Project
Top Contributors - Brenna Rutledge, Evi Peeters, Alicia Keefe, Khloud Shreif, Kim Jackson, Admin, Lieselot Longe, WikiSysop, Max Louis, Claire Knott, Wanda van Niekerk, Lucinda hampton, Wendy Snyders and Scott A Burns
This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work!
Definition/Description[edit | edit source]
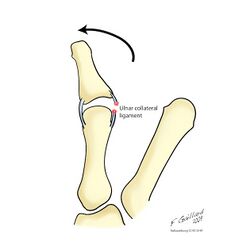
Skier's thumb is an acute partial or complete rupture of the ulnar collateral ligament (UCL) of the thumb’s metacarpophalangeal joint (MCPJ) due to a hyperabduction trauma of the thumb.
Whilst both terms are often used interchangeably, the skier’s thumb refers to the cause as being acute injury. Gamekeeper’s thumb specifically refers to the cause being associated with a chronic injury to the UCL in which it became attenuated through repetitive stress.
UCL damage caused by Chronic injury may have a serious risk of disabling instability, pinch strength, and pain-free motion if not treated adequately.[1][2][3][4][5]
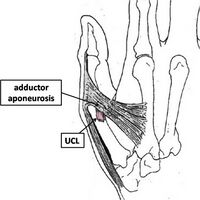
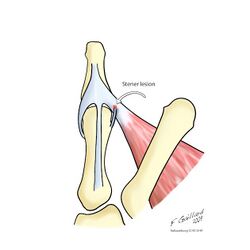
In 64–87% of total UCL tears, a Stener lesion can occur. A Stener lesion occurs when the adductor aponeurosis becomes interposed between the ruptured UCL and its site of insertion at the base of the proximal phalanx. Hence making it impossible for the loosened ligament to reconnect with the site of insertion, necessitating surgery.[7]
Clinically Relevant Anatomy[edit | edit source]
The metacarpophalangeal joint of the thumb is a diarthrodial joint, reinforced by a capsule and by other soft tissue structures. The surrounding soft tissue offers both dynamic and static stability.[9]
The passive stability is provided by the following structures:
- Proper collateral ligament
- Accessory collateral ligament
- Volar plate
- Dorsal capsule[10]
The proper collateral ligament extends from a point slightly dorsal to the mid-axis of the metacarpal head to the palmar aspect of the proximal phalanx. It prevents palmar subluxation of the proximal phalanx and serves as the primary restraint to valgus stress with the metacarpophalangeal joint in flexion. The accessory collateral ligament courses are palmary to insert onto the volar plate. The accessory collateral ligament is contiguous with the proper collateral ligament proximally. The volar plate and the accessory collateral ligament function as the principal restraints to valgus stress with the metacarpophalangeal joint in extension. [10]
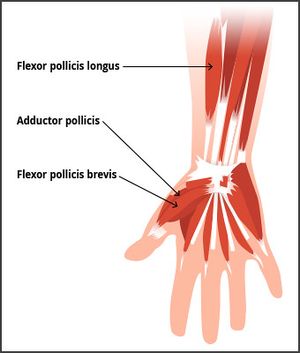
Dynamic stabilizers to valgus stress consist of the intrinsic and extrinsic muscles of the thumb:
- Extensor pollicis brevis
- Extensor pollicis longus
- Flexor pollicis longus
- Adductor pollicis
- Flexor pollicis brevis
The adductor mechanism presents as an aponeurosis superficial to the metacarpophalangeal joint capsule and ulnar collateral ligament. The superficial insertion of the adductor mechanism is the extensor expansion via the adductor aponeurosis while the deep insertion extends to the palmar aspect of the proximal phalanx via the ulnar sesamoid of the metacarpophalangeal joint [9][3]. There are two main supporting ligaments traversing the MCPJ of the thumb:
- The ulnar collateral ligament (UCL)
- The radial collateral ligament (RCL)
The UCL and RCL arise from the medial and lateral tubercles of the metacarpal condyles and insert into the base of the proximal phalanx on their respective sides, beneath the adductor aponeurosis.[9][11] The UCL prevents the thumb from pointing too far away from the hand.[1]
Etiology[edit | edit source]
Skier’s thumb is caused by forced abduction and hyperextension of the thumb. [12] The UCL tears mostly find a place at the distal attachment of the proximal phalange. But proximal avulsion, proximal and distal bony avulsion, isolated mid-substance tears, and mid-substance tears with bony avulsion do also occur. [13]
Mechanism of Injury.[edit | edit source]
It is important to note that this injury is not exclusive to skiers and can occur to anyone where there is an extreme valgus stress force applied to the thumb in abduction and extension [14]or small repetitive valgus stress force. This type of injury is also seen in other sports, especially those that use a stick or ball, such as hockey or basketball.
An acute UCL injury occurs following a sudden, hyperabduction and hyperextension forces[13] at the MCP joint, whereas a forced adduction movement would cause injury to the RCL.[9] With regards to skiing, the injury often occurs when a person lands on an outstretched hand while holding a ski pole, which causes forced abduction of the thumb with extension.[15] It is called skier’s thumb but can also occur in football, handball, basketball, rugby, soccer, and even a handshake. [13] If the injury to the UCL is not treated properly this can lead to chronic laxity, joint instability, pain, weakness, and arthritis in the MCPJ.
Epidemiology[edit | edit source]
It concerns 86% of all injuries to the base of the thumb and about 200,000 patients per year in the USA. Skier’s thumb is the second most common ski-related injury after knee injury, and more common in males than females. Prevalence of this injury during skiing varies from 7% up to as high as 32% of all skiing injuries and is the most frequent injury of the upper extremity that skiers experience[14][16][4]. Only an estimated 10% of the patients diagnosed with a skier’s thumb had acquired this injury skiing.
A fall on the hand, usually from a bicycle or motorcycle (in which the thumb gets stuck behind the handlebars), is a much more common cause of skier’s thumb, seen in approximately 40 % of all patients. Other sports such as soccer or fighting are responsible for another estimated 30% of the causes.
In children, who still have an immature skeleton, hyperabduction trauma mostly leads to a Salter-Harris III avulsion of the UCL insertion and rarely to a true rupture of the UCL. [4]
Prevention[edit | edit source]
Preventive measures should include instruction in proper pole technique for powder skiing, avoidance of pole dragging and deep pole plants, and downsizing baskets from the standard 4-inch diameter to 2.5-inches. Pole length should be 2 inches shorter than the recommended length for that skier. [17]
Strapless poles do not reduce the chance of injuries, but if skiers are trained to discard the pole during a fall the risk might be reduced. [18]
The risk of injury can be further reduced by wearing a properly designed ski-glove which not only prevents extreme movement of the thumb but also incorporates a mechanism for the ejection of the ski-pole[19][20].
Characteristics/ Clinical Presentation[edit | edit source]
The most common presentation is pain over the ulnar aspect of the MCPJ of the thumb. If the injury is acute there will be bruising and inflammation. There may be tenderness with palpation, which localizes the injury to the ulnar aspect of the thumb where the UCL is lesioned. In more chronic cases the patients typically complain of pain and weakness when using a pincer grip. There also can be instability of the thumb while doing these tasks[13][9]. In the instance of a Stener lesion, there may also be a palpable mass proximal to the adductor aponeurosis[15].
Symptoms[edit | edit source]
These symptoms may occur minutes to hours after the fall that created the injury:[21]
- Pain at the base of the thumb in the webspace between thumb and index finger.
- Swelling of your thumb.
- Inability to grasp or weakness of grasp between your thumb and index finger.
- Tenderness to the touch along the index finger side of your thumb.
- Blue or black discoloration of the skin over the thumb.
- Thumb pain that worsens with movement in any or all directions.
- Pain in the wrist (which may be referred pain from your thumb).
Grades of thumb sprains[edit | edit source]
Thumb sprains are ranked by how much the ligament is pulled or torn away from the bone[10]. Classification of UCL injury according to Hintermann et al, as the following:
| Type | Injury | Examination |
| I | Undisplaced fracture | Stable in flexion (<30°) |
| II | Displaced fracture | No special test |
| III | No fracture | Stable in flexion (<30°) |
| IV | No fracture | Unstable in flexion (>30°) |
| V | Avulsion fracture of the volar plate | Stable in flexion |
Presentation of an ulnar collateral ligament injury with an avulsion fracture. Photo courtesy H. Stevenson.
Differential Diagnosis[edit | edit source]
The injury can involve other structures such as the adductor aponeurosis, the accessory collateral ligament, bony structures, tendons, and neurological tissues.[15] The injuries all present with pincer grasp weakness. However, they may be differentiated by the location of tenderness.
- Stener lesion: is a particular type of UCL injury with palmar subluxation of the base of the proximal phalanx.
- Bennett or Rolando fracture: is an intra-articular fracture luxation at the base of MC I in the CMC joint.[13]
- Avulsion fracture: In children, who still have an immature skeleton, hyperabduction trauma mostly leads to a Salter-Harris III avulsion of the UCL insertion and rarely to a true rupture of the UCL[4].
- Wrist sprain: when a wrist sprain injury occurs, the ligaments of the wrist are stretched beyond their normal limits.
- Wrist fracture.
- Chronic instability of the 1ste MCP joint: Injuries to the two main supporting ligaments traversing the metacarpophalangeal (MCP) joint of the thumb can lead to symptomatic joint instability with subsequent pain, weakness and arthritis if ignored. These two ligaments are the ulnar and radial collateral ligaments[24].
- Neuropraxia of the radial nerve arises secondary to traction, swelling, or stiffness.
- Rheumatoid arthritis/ osteoarthritis.
Complications[edit | edit source]
If the UCL is ruptured there is a possibility that the distal end may become interposed by the adductor aponeurosis, which is referred to as a Stener lesion (Figure 5). A Stener lesion is difficult to diagnose but leads to poor healing and usually indicates operative management. If left untreated, a torn UCL can lead to joint instability and a weak pinch grip[26].
Diagnostic Procedures[edit | edit source]
The type of lesion can be accurately derived by means of X-ray, ultrasound, or MRI.
X-rays[edit | edit source]
Anteroposterior and lateral X-ray films of the thumb are taken to rule out any associated bony injuries. Associated bony avulsion fractures are seen in 20%–30% of UCL ruptures. The position of an avulsed bony fragment usually indicates the position of the distal end of the UCL.[27] Indications for surgical treatment based on imaging include avulsion fractures with displacement of greater than 5 mm or any fracture involving 25% or more of the MCP joint surface. Stress X-ray films of the thumb MCP joint have also been used for diagnosis[28].
Ultrasound[edit | edit source]
Ultrasound (US) is an excellent and cost-effective modality for diagnosing UCL tears because it allows direct visualization of the entire UCL and surrounding structures. It locates the torn end of the UCL in almost 90% of cases [16].The diagnosis should be done by the US before conservative therapy is performed with a glove spica cast. There are some limitations when applying, for example, the ultrasound cannot be performed later than 1 week after the initial trauma because shrinking of the torn ligament and scar tissue can be confounding when making a diagnosis [2][29] or for chronic UCL injuries.
The sensitivity of US was 95.4% with a specificity of 80% for detection of Stener lesions. The US, with the use of this specific dynamic maneuver, is a reliable and reproducible tool for detecting Stener lesions.
MRI[edit | edit source]
MRI can be seen as a gold standard with a sensitivity of 96%-100% and specificity of 95-100%. An alternative can be an ultrasound of the thumb[2]. It is considered by some as the best modality for evaluating UCL injuries, especially for chronic UCL injuries[30].
Arthrography[edit | edit source]
Arthrography involves distension of the MCP joint by injecting contrast material and then visualizing the joint by X-ray or MRI (MR-arthrography). UCL injuries are diagnosed by direct visualization of any focal defect or by extravasation of contrast from the joint, suggesting rents in the ligaments. Another indirect finding on arthrography suggestive of UCL tear is a demonstration of the heads of the adductor pollicis muscle[13][31].
Clinical and anatomical findings and the understanding of the injury mechanism show that stability testing (performed with the joint in full flexion) and additional standard radiographs remain the keystones in decision making in all MCPJ sprains
Follow up.[edit | edit source]
The orthopedic surgeon will see the patient after surgical repair or after a period of immobilization in a cast. The patient's thumb will be reexamined. The doctor will decide if the patient needs to continue to immobilize the thumb or if physical therapy is needed to regain movement. The remainder of the rehabilitation and the management of any chronic problems that may arise from the injury will be addressed by your orthopedic or hand surgeon. [21]
Examination[edit | edit source]
Begin looking for deformities with the observation of the hand at rest and flexion. Then test the sensation in the hand followed by active range of motion (AROM) followed by passive range of motion (PROM) and resisted movement to assess tendon integrity, if possible[9]. Clinical examination may occasionally reveal a tender swelling and a hematoma at the ulnar side of the base of the thumb[4]. If there is a fracture suspected to the first metacarpal or proximal phalanx of the thumb, plain radiographs are indicated prior to stress testing of the UCL.
Objective examination and X-ray are sensitive to detect UCL injuries[32]. If there is no associated fracture of the shaft, the thumb MCP joint stability is tested by stress test and detect the firm endpoint as the following;
- The metacarpal is stabilized by one hand to support the proximal phalanges of the thumb from any strain.
- With the proximal phalanges in 30° flexion radial stress is applied and repeated in the extended position to detect the firm end point.
- The degree of deviation compared with the other side, a difference of 15° between the affected and opposite sides in flexion, or the degree is > 35° denotes a tear of the primary UCL and in extension a tear of the accessory part of the UCL.
- If it is not detected there will be a complete UCL tore, the absence of a firm endpoint during testing is a more reliable criterion when clinically diagnosing a complete rupture of the UCL[3],[4]
- If there is a stener lesion the examiner will feel a ligamentous lump.
A stress test may be painful and the examiner may need to use local anesthesia to can do the test and avoid the tension of the surrounding muscles. It is fair to say we can find laxity/instability of the thumb MCP joint in cases of chronic UCL injuries[13].
A study by Cooper et al "Local anesthetic infiltration increases the accuracy of assessment of ulnar collateral ligament injuries" described how Oberst anesthesia (in which 1–2 ml of lidocaine is injected in the MCP joint) increases the clinical accuracy from 28% to 98% after an average of one week after the initial trauma.
In most of the literature the following standard has been used for laxity of the MCP joint.
Medical management[edit | edit source]
A UCL injury may be managed conservatively or surgically depending on various factors that primarily include: timing of presentation (acute or chronic); grade (severity of injury); displacement (Stener lesion); location of tear (mid-substance or peripheral); associated or concomitant surrounding tissue injury (bone, volar plate, etc.); and patient-related factors (occupational demands, etc.)[13] Indication for operative treatment of ulnar collateral ligament injuries of the thumb should be made on the basis of whether the ligament is displaced proximal to the adductor aponeurosis or not (Stener Leasion). Thus the diagnostic efforts should concentrate on ligament displacement rather than whether the ligament is ruptured totally or partially. [34]
An injury that is not managed properly can lead to chronic instability of the MCPJ.[15] Operative management depends on a timely diagnosis of the injury; chronic lesions become more difficult to repair with increased time since injury since remaining tissue becomes attenuated not robust enough to provide adequate support to the joint.[35] There are multiple methods of repair, which can be categorized into dynamic or static.[9][35]
Dynamic:[edit | edit source]
- Extensor indicis proprius tendon transfer
- Extensor pollicis brevis tendon transfer
- Adductor pollicis brevis tendon transfer
Dynamic procedures are more likely to loosen with time while usually preserving good mobility of the MCP joint. [36]
Static:[edit | edit source]
- Figure-of-eight grafting
- Parallel configuration graft
- Triangular configuration with proximal apex graft
- Triangular configuration with distal apex graft
- Dually opposed biotenodesis fixation of the tendon graft
- Tendon graft weaves
- Dually opposed suture anchor fixation
- Hybrid technique
- Free tendon graft: an insertion is made on the ulnar side of the thumb, exposing the ligament remnant. A tendon graft is used to connect the bones. The tendon graft replaces the ligament and is proximal bound to the ligament remnant and distal to the phalangeal bone. [37]
There is a wide variety in static operations and there is still a lot of discussions about which treatment is the best. Most treatments give positive results which lead to a lot of discussions.[36] [38]
Provided surgery has been performed timely ( quality of results drops when surgery is delayed, good results can still be achieved after 3–4 weeks. A period of usually 6 weeks of immobilization is applied, after which a new radiograph is made and physical therapy of the hand can be started. When the pain has subsided and the range of motion has completely returned, the hand can be used again to full effect. Usually, this takes about 3 months Patients with worse outcomes are mostly patients with a delay in presentation. When repaired in a timely manner, complications are rare.
Different surgical techniques can be used. Which one applies depends on the anatomy of the lesion and can often only be decided upon during surgery. The UCL can be fixated with a suture anchor or with transosseous stitches. Small bone fragments can be removed; larger ones can be fixated with a Kirschner wire or a small screw. Results seem to be independent of the chosen technique, and successful recovery to the patient’s level before the initial trauma occurs in 90%-96% of all patients [8,21,22]. This means that the question remains whether the patients mentioned above (with persisting complaints after the first non-surgical and later surgical treatment) would have benefitted from initial surgical intervention
Not enough information is available on the chances for recurrence with this type of injury. Also, no trials have even been set up to investigate whether surgical intervention is really superior to non-surgical treatment.[4]
Physical Therapy Management[edit | edit source]
The treatment of skier’s thumb is different for partial and complete ruptures. Partial ruptures are treated conservatively. The MCP joint is immobilized, with the MCP fixed and the IP joint remaining free to prevent unnecessary stiffness. A navicular cast or brace is usually used. Swelling can be controlled with elevation while supine and the use of cold compresses as needed.[35]
The primary goal of rehabilitation is enhancing the patients' function and reducing the time of functional recovery, the reported treatment presents potential advantages in the management of this frequent acute hand injury.
Conservative treatment[edit | edit source]
Partial UCL injuries like ligament strains, partial tears, low-demand patients, and poor-operative candidates, including patients with degenerative MCP joint disease are effectively treated conservatively.[35]
Controversy also exists about treating a bony skier’s thumb without surgery. The literature however shows that if the MCP joint is stable during testing and there is no dislocation of the fragment, this injury can be treated conservatively without reason for concern.
- For patients with:
- less than 30 degrees of valgus laxity of extension of the MCPJ
- Less than 15 degrees difference between sides and no signs of avulsion fracture on radiographs.[15]
Immobilisation[edit | edit source]
from 10 days up to 6 weeks, depending on the degree of laxity during the initial examination. Authors of a recent review on skier’s thumb agreed on a 4-week period. [4]suggestions:
- A short-arm thumb spica cast
- Thermoplastic splint: allows for the patient to begin the movement of the interphalangeal joint.
- A hand-based removable thumb spica orthosis. The MCP joint is immobilized, with the MCP fixed and the IP joint remaining free to prevent unnecessary stiffness.(Figure 7)[15][4][39]
Wearing a splint will avoid putting radial stress on the thumb and gives the ligament time to heal.[15] The optimal positioning for the splint involves holding the MCPJ in slight flexion with a slight ulnar deviation; the interphalangeal joints should not be immobilized in the splint.[15]
Exercise therapy[edit | edit source]
After the period of immobilization is over, the therapy can be started. Most likely the patient will perform exercises that help strengthen and stretch the joint in order to regain full function in your thumb. (11) The patient should begin supervised hand therapy during the period of immobilization.[15] Gentle flexion and extension range of motion exercises can begin after about four weeks, with the patient continuing to wear the splint between therapy sessions. After 8 weeks progressive strengthening exercises may begin, but unrestricted activity is not allowed until after 12 weeks.[15] Gripping and pinching activities should not start until 10-12 weeks and should be advanced as tolerated; forceful gripping activities are typically not tolerated until about week 12.[35]
Treatment after surgery[edit | edit source]
The content of the physical therapy after surgery is the same as those of the conservative treatment, besides:
Duration of Immobilisation: usually 6 weeks is applied- Control radiograph after immobilisation
Following surgery a splint is usually worn for four to five weeks. The immediate postoperative motion of the operated joint produced faster and better functional results. Therefore the use of a functional splint is preferred, as well as the early progressive start with moving within the boundaries of pain. [39] Athletes whose injuries require surgery can usually return to play in about three to four months. [11] The study of Derkash, considering pain, stability, muscular force (tweezers grip), and functionality in ADL, shows that less than 5% of the patients experience a weakened tweezers grip and stiffness. Pain was absent or mild in 99% of the cases. 96% of the treated patients were satisfied with the results of the operation. When a secondary operation is required results were less successful. [40]
When the pain has subsided and the range of motion has completely returned, the hand can be completely used again. Usually, this takes about 3 months.[4]
Exercises. [41][edit | edit source]
Thumb active range of motion[edit | edit source]
With your palm flat on a table or other surface, move your thumb away from your palm as far you can. Hold this position for 5 seconds and bring it back to the starting position. Then rest your hand on the table in a handshake position. Move your thumb out to the side away from your palm as far as possible. Hold for 5 seconds. Return to the starting position. Next, bring your thumb across your palm toward your little finger. Hold this position for 5 seconds. Return to the starting position. Repeat this entire sequence 15 times. Do 2 sets of 15. [41]
Wrist range of motion[edit | edit source]
- Flexion: Gently bend your wrist forward. Hold for 5 seconds. Do 2 sets of 15. [41]
- Extension: Gently bend your wrist backward. Hold this position for 5 seconds. Do 2 sets of 15.[41]
- Side to side: Gently move your wrist from side to side (a handshake motion). Hold for 5 seconds in each direction. Do 2 sets of 15.[41]
- Thumb strengthening: Pick up small objects, such as paper clips, pencils, and coins, using your thumb and each of your other fingers, one at a time. Practice this exercise for about 5 minutes.[41]
- Finger spring: Place a large rubber band around the outside of your thumb and fingers. Open your fingers to stretch the rubber band. Do 2 sets of 15. [41]
- Grip strengthening: Squeeze a soft rubber ball and hold the squeeze for 5 seconds. Do 2 sets of 15.[41]
- Wrist flexion: Hold a can or hammer handle in your hand with your palm facing up. Bend your wrist upward. Slowly lower the weight and return to the starting position. Do 2 sets of 15. Gradually increase the weight of the can or weight you are holding.[41]
- Wrist extension: Hold a soup can or hammer handle in your hand with your palm facing down. Slowly bend your wrist up. Slowly lower the weight down into the starting position. Do 2 sets of 15. Gradually increase the weight of the object you are holding.[41]
Clinical Bottom Line[edit | edit source]
Skier’s thumb, also known as the gamekeeper's thumb, is an injury to the metacarpal phalangeal joint of the thumb. It can occur to the medial side of the thumb, but this is rare. The chance of a medial side injury is as small as 10-30%.
When there is an abnormal movement like hyperabduction of the thumb or a sudden force on the thumb then the ligament can rupture (with or without an avulsion fracture). We diagnose UCL rupture mostly with an ultrasound, which is the most reliable and not costly. We can also palpate a rupture by doing the stress test.
UCL rupture can be treated with an operation but this depends on different factors(see medical management). When an operation is needed, the treatment will likely be decided by the surgeon. This will also depend on some factors but most surgeons have a favorite treatment in a wide variety of operations.
Partial tears and strains are mostly not treated with an operation. It comes first with the immobilization of the MCP joint to give some rest so that the body can recover. After that, the patient starts wearing a splint and gets six weeks of therapy sessions (this also includes post-operative treatments). Where the mobility and strength get back to the normal values compared with the contralateral thumb.
References[edit | edit source]
- ↑ 1.0 1.1 Ritting AW, Baldwin PC, Rodner CM. Ulnar collateral ligament injury of the thumb metacarpophalangeal joint. Clinical Journal of Sports Medicine. 2010 Mar 1;20(2):106-12.
- ↑ 2.0 2.1 2.2 Mahajan M, Rhemrev SJ. Rupture of the ulnar collateral ligament of the thumb–a review. International journal of emergency medicine. 2013 Dec;6(1):1-6.
- ↑ 3.0 3.1 3.2 Tsiouri C, Hayton MJ, Baratz M. Injury to the ulnar collateral ligament of the thumb. Hand. 2009 Mar;4(1):12-8.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 4.8 4.9 Mahajan M, Rhemrev SJ. Rupture of the ulnar collateral ligament of the thumb–a review. International journal of emergency medicine. 2013 Dec;6(1):1-6.
- ↑ Ritting AW, Baldwin PC, Rodner CM. Ulnar collateral ligament injury of the thumb metacarpophalangeal joint. Clinical Journal of Sport Medicine. 2010 Mar 1;20(2):106-12.
- ↑ Anna Pickens . Game keepers thumb. EM in 5. Available from: https://www.youtube.com/watch?v=0ZUtTT9v3r0 (last accessed 15.4.2019)
- ↑ Ebrahim FS et al. US diagnosis of UCL tears of the thumb and Stener lesions: technique, pattern-based approach, and differential diagnosis. Radiographics. 2006; 26(4): 1007-20
- ↑ ORTHOfilms . Stener Lesion. EM in 5. Available from: https://www.youtube.com/watch?v=RLskrc7qifY(last accessed 15.4.2019)
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 9.6 Patel S, Potty A, Taylor EJ, Sorene ED. Collateral ligament injuries of the metacarpophalangeal joint of the thumb: a treatment algorithm. Strategies in trauma and limb reconstruction. 2010 Apr;5(1):1-0.
- ↑ 10.0 10.1 10.2 Sebastin S, et al. Overview of a finger, hand, and wrist fractures. http://www.uptodate.Foye PM et al, Skier’s Thumb. Medscape. 2010
- ↑ American Society for Surgery of the Hand. Thumb sprains. www.assh.org/Public/HandConditions/Pages/ThumbSprains.aspx (accessed 18 March 2011)
- ↑ Pediatric Trauma Care II: A clinical reference for physicians and nurses caring for the acutely injured child. AHC Media. LLC. 2014;6:52-53
- ↑ 13.0 13.1 13.2 13.3 13.4 13.5 13.6 13.7 Madan SS, Pai DR, Kaur A, Dixit R. Injury to the ulnar collateral ligament of thumb. Orthopaedic surgery. 2014 Feb;6(1):1-7.
- ↑ 14.0 14.1 J. B. Engelhardt, Rupture of the ulnar collateral ligament of the metacarpophalangeal joint of the thumb. injury.1993;vol24:1:21-24
- ↑ 15.0 15.1 15.2 15.3 15.4 15.5 15.6 15.7 15.8 15.9 Anderson D. Skier's thumb. Australian family physician. 2010 Aug;39(8):575-7.
- ↑ 16.0 16.1 ChuterG.S.J. Ulnar collateral ligament injuries of the thumb: 10 years of surgical experience. Injury. June 2009;vol40:6:652-656.
- ↑ Palmer DH et al. Helicopter skiing wrist injuries. A case report of “bugaboo forearm”.; Am J Sports Med. 1994 Jan-Feb;22(1):148-9
- ↑ Fricker R1, et al.Skier’s thumb. Treatment, prevention and recommendations
- ↑ J. A. Fairclough et al. Skier’s thumb-a method of prevention; Injury 1986; 17,203-204
- ↑ Fricker R, Hintermann B. Skier’s thumb. Sports Medicine. 1995 Jan;19(1):73-9.
- ↑ 21.0 21.1 Glickel SZ, et al. Dislocations and ligament injuries in the digits. Green DP, Hotchkiss RN, Pederson WC, eds. Green’s Operative Hand Surgery. 4th ed. New York, NY: Churchill Livingstone. 1999; 772-807
- ↑ Michael A. et al, Evaluation and Treatment of Injuries of the Ulnar Collateral Ligament of the Thumb Metacarpophalangeal Joint, Bulletin of the NYU Hospital for Joint Diseases. 2009;67(1):68-74
- ↑ Hall ™, et al. Therapeutic Exercise Moving Toward Function. 3rd ed; Lippincott, Williams and Wilkins, 2010
- ↑ Shelain Patel, et al. Collateral ligament injuries of the metacarpophalangeal joint of the thumb: a treatment algorithm; Strategies Trauma Limb Reconstr. 2010; 5(1): 1–10
- ↑ Zemel NP. Metacarpophalangeal joint injuries in fingers. Hand Clin. 1992; 8(4):745-54
- ↑ Leggit JC et al. Acute finger injuries: Part II. Fractures, dislocations, and thumb injuries. Am Fam Physician. 2006;73(5):827-834
- ↑ Thirkannad S, Wolff TW. The ‘‘two fleck sign for an occult Stener lesion. Journal of Hand Surgery (European Volume). 2008 Apr;33(2):208-11.
- ↑ Rodríguez AS. Simultaneous bilateral functional radiography in ulnar collateral ligament lesion of the thumb: an original technique. American Journal of Orthopedics. 2015 Aug.
- ↑ Ebrahim FS, De Maeseneer M, Jager T, Marcelis S, Jamadar DA, Jacobson JA. US diagnosis of UCL tears of the thumb and Stener lesions: technique, pattern-based approach, and differential diagnosis. Radiographics. 2006 Jul;26(4):1007-20.
- ↑ Lohman M, et al. MR imaging in chronic rupture of the ulnar collateral ligament of the thumb. Acta Radiol. 2001; 42: 10–14
- ↑ Campbell RE, McGhee AN, Freedman KB, Tjoumakaris FP. Diagnostic imaging of ulnar collateral ligament injury: a systematic review. The American Journal of Sports Medicine. 2020 Sep;48(11):2819-27.
- ↑ Prein TK, Brogren E, Dahlin LB, Søe NH, Brorson S. Ulnar collateral ligament injury to the thumb. Ugeskrift for Laeger. 2021 Jul 1;183(28).
- ↑ Dr. Tamara Hefferon. Thumb UCL Test: Skier's Thumb . Available from: http://www.youtube.com/watch?v=sAzgUuvUDvo[last accessed 20/2/2022]
- ↑ Abrahamsson SO, et al. Diagnosis of displaced ulnar collateral ligament of the metacarpophalangeal joint of the thumb. J Hand Surg Am. 1990; 15: 457–460
- ↑ 35.0 35.1 35.2 35.3 35.4 Rettig A et al. Anatomic reconstruction of thumb metacarpophalangeal joint ulnar collateral ligament using an interference screw docking technique. Tech Hand Up Extrem Surg. 2009;13(1):7-10.
- ↑ 36.0 36.1 C. Fusetti. The ECRL bone-tendon ligamentoplasty for chronic ulnar instability of the metacarpophalangeal joint of the thumb. Hand Surgery Unit, Chirurgie de la Main. 2005; Vol 24:5:217–221
- ↑ G.I Mitsionis. treatment of chronic injuries of the ulnar collateral ligament of the thumb using a free tendon graft and bone suture anchors. The Journal of Hand Surgery:British & European volume. 2000; Vol 25:2:208–211
- ↑ Başar H. Comparison of results after surgical repair of acute and chronic ulnar collateral ligament injury of the thumb. Chirurgie de la Main. 2014;vol 33:6:384–389
- ↑ 39.0 39.1 Rocchi L, et al. A modified spica-splint in postoperative early-motion management of skier’s thumb lesion: a randomized clinical trial.
- ↑ Derkash RS, et al. Acute surgical repair of the skier’s thumb. Clin Orthop Relat Res 1987;(216):29-33
- ↑ 41.0 41.1 41.2 41.3 41.4 41.5 41.6 41.7 41.8 41.9 Mayfield JK, et al. Carpal dislocations: pathomechanics and progressive perilunar instability. J Hand Surg Am. 1980;5 (3): 226-41