Salter-Harris Fractures
Original Editor - Margaret Layden
Top Contributors - Meaghan Rieke, Admin, Kim Jackson, Margaret Layden, Vidya Acharya and WikiSysop
Introduction[edit | edit source]
Salter-Harris fractures (physeal fractures) refer to fractures through a growth plate (physis) and are therefore specifically applied to bone fractures in children. The commonest injuries seen in children with open growth plates are fractures involving epiphyseal plates, or physis[1][2].
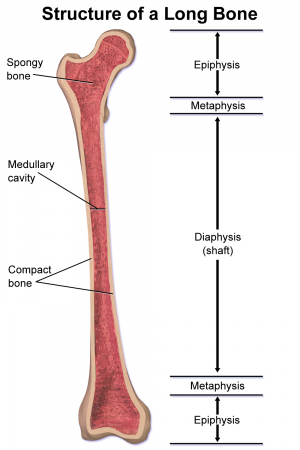
Clinically Relevant Anatomy[edit | edit source]
The bones of growing children contain four sections including the diaphysis (shaft), metaphysis, and epiphysis (end). The metaphysis and epiphysis are separated by the physis (growth plate). Salter-Harris fractures are unique to children because they involve the growth plate. Cartilage grows from the epiphysis up toward the metaphysis and neovascularization develops from the metaphysis toward the epiphysis. Damage to the vascular supply will disrupt bone development but damage to the cartilage may not cause a problem if it is repositioned appropriately and the vasuclar supply has not been disrupted.[3]
Classification[edit | edit source]
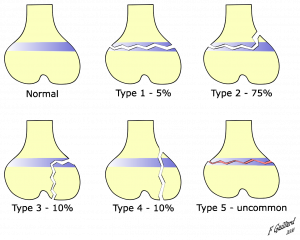
Salter-Harris fractures are classified into 5 types:
- Type I is a fracture through the growth plate. The fracture line extends through the physis or within the growth plate. Type I fractures are due to the longitudinal force applied through the physis which splits the epiphysis from the metaphysis.
- Type II extends through the metaphysis and the growth plate. There is no involvement of the epiphysis. This is the most common of the Salter-Harris fractures.
- Type III is an intra-articular fracture through the growth plate and the epiphysis. This is rare and when it does occur, it is usually at the distal end of the tibia. If the fracture extends the complete length of the physis, this type of fracture may form two epiphyseal segments. Since the epiphysis is involved, damage to the articular cartilage may occur. One example of this is a Tillaux fracture of the ankle, which is a fracture of the anterolateral aspect of the growth plate andepiphysis[2].
- Type IV extends through the epiphysis, the growth plate and the metaphysis.
- Type V is a crushing type or compression injury of the growth plate injury that affects the growth plate.[3] The force is transmitted through the epiphysis and physis, potentially resulting in disruption of the germinal matrix, hypertrophic region, and vascular supply. Though Harris-Salter V fractures are very rare, they may be seen in cases of electric shock, frostbite, and irradiation. As this fracture pattern tends to result from severe injury, these typically have a poor prognosis leading to bone growth arrest[2].
- There are Type VI-Type IX fractures also but these are rare.
Mechanism of Injury / Pathological Process[edit | edit source]
Salter-Harris fractures are often the result of sports-related injuries however they have also been attributed to child abuse, genetics, injury from extreme cold, radiation and medications, neurological disorders, and metabolic diseases which all affect the growth plate according to the National Institute of Arthritis and Musculoskeletal and Skin Diseases.[4]
Approximately 1/3rd of Salter-Harris fractures occur as the result of sports and 1/5th occur from recreational activities. They may result from a single injury or may be caused by repetitive stresses on the upper and lower extremities.[4]
Clinical Presentation[edit | edit source]
Point tenderness on palpation at the epiphyseal plate may indicate a fracture. Other signs to look for are persistent pain or pain that affects the child’s ability to tolerate weight bearing through the limb or use of the limb. [4] Soft tissue swelling and/or visible deformity could be another sign of a fracture.[4]
Diagnostic Procedures[edit | edit source]
The diagnostic process begins with obtaining a history of the patients medical status and the mechanism of injury. The Ottawa Rules and Low-Risk Ankle Rule can be used to determine the need for a radiograph.[5] Radiographs may be negative, especially with a Type I fracture.[5] The contralateral limb will be radiographed as well for comparison. Magnetic resonance imaging (MRI), computed tomography (CT) and ultrasound may also be used. [4]
.
Management / Interventions[edit | edit source]
Medical Management[edit | edit source]
According to information from NIAMS:
Type I and most Type II fractures are treated with cast immobilization with closed reduction and casting or splinting. The reduction should be performed carefully to avoid damage to or grating of the physis on any metaphyseal bone fragments[2].
Although Type II sometimes requires surgery. Both normally heal well.
Type III disrupts the growth plate and therefore requires surgery. Internal fixation may be required to allow for good alignment. Open reduction and internal fixation (avoiding crossing the physis)[2].
Type III and IV fractures with displacement of less than 2mm may also be managed non-surgically with a period of non-weight bearing in a cast followed by a period of non-weight bearing in a fracture boot.[6]
Type IV and Type V are also usually treated with surgery with internal fixation.[7]
The patient is seen by their physician for assessment of their growth over the next 2 years, usually at 3-6 month intervals. Approximately 85% of growth plate fractures heal without any long-term deficits. The most common complication of growth plate fractures is the early arrest of bone growth which may lead to a short limb or a crooked limb. There is a greater incidence of this at the knee compared to the upper extremity.[4] In addition, Type I and II fractures have the lowest risk of physeal (growth) arrest.[6]
Rehabilitation[edit | edit source]
The patient may be referred for physical therapy to restore range of motion, strength, and function. In the acute phase after injury or surgical management, physical therapy should focus on assisting the patient with adhering to immobilization or weight-bearing protocols. Controlled range of motion exercises and light strengthening can be implemented. After the growth plate has undergone sufficient healing, progressive strengthening, range of motion, balance, and proprioception exercises should be implemented. In young athletes, advanced rehabilitation should include sport-specific exercises and drills.[8]
Outcome Measures[edit | edit source]
Return to play/return to sport testing should be used. Involved muscle strength should be 90% of the contralateral muscle strength in order for athletes to return to previous sports or activities.[8] Joint- or body region-specific outcome measures can be used based on the fracture location.
Differential Diagnosis[edit | edit source]
According to Moore et al., ankle fractures, wrist, and scaphoid fractures and complications should be considered.[3]
Additionally, one needs to consider medications, radiation, neurological disorders, metabolic disease, or exposure to extreme cold especially if no specific injury can be identified.[4]
References[edit | edit source]
- ↑ Cepela DJ, Tartaglione JP, Dooley TP, Patel PN. Classifications In brief: salter-harris classification of pediatric physeal fractures.
- ↑ 2.0 2.1 2.2 2.3 2.4 Levine RH, Foris LA, Waseem M. Salter Harris Fractures. InStatPearls [Internet] 2019 Jun 14. StatPearls Publishing.
- ↑ 3.0 3.1 3.2 Moore W, Smith TH. Salter-harris fractures. http://emedicine.medscape.com/article/412956-print (accessed 24 Jun 2018).
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 National Institutes of Health. Growth plate injuries. https://www.niams.nih.gov/health-topics/growth-plate-injuries (accessed 24 Jun 2018).
- ↑ 5.0 5.1 Su AW, Larson AN. Pediatric ankle fractures: concepts and treatment principles. Foot Ankle Clin 2015;20(4):705-719.
- ↑ 6.0 6.1 Wuerz TH, Gurd DP. Pediatric physeal ankle fracture. J Am Acad Orthop Surg 2013; 21:234-244.
- ↑ Consumer Health Information Network. arthritis-symptom.com/fracture/salter-harris-fracture.htm
- ↑ 8.0 8.1 Paterno, MV. Unique issues in the rehablitation of the pediatric and adolescent athlete after musculoskeletal injury. Sports Med Arthrosc Rev 2016;24:178-183.