ACL Rehabilitation: Acute Management after Surgery
Original Editor - Your name will be added here if you created the original content for this page.
Top Contributors - Mariam Hashem, Kim Jackson, Tarina van der Stockt, Chelsea Mclene, Tony Lowe, Leana Louw, Wanda van Niekerk, Jess Bell, Robin Tacchetti, Jorge Rodríguez Palomino and Rachael Lowe
Introduction[edit | edit source]
Anterior Cruciate Ligament injury is one of the most common injuries among different sports. In football , the range of ACL injuries has been estimated to range from 0.06 to 10 injuries per 1000 game hours. Professional athletes are more prone to ACL injures[1]. Most injuries occur when the opposite tam has the ball and the players are defending with tackling and cutting are considered the most common playing actions assosiated with the injury (51% and 15% respectively).
Females are at a higher risk for ACL injury[2] due to many factors such as higher valgus stress and loading in females when performing tasks, differences in hamstring/quadriceps strength ratio and vastus lateralis/semitendinous strength ratio, lateral and posterior hip insufficiencies, and nondominant leg strength differences[3]. In contrast, a case series report by Brophy et al reported no differences between the genders[4]. The difference between male ad female athletes according to this report was in the mechanism of injury; males were more likely to suffer contact injuries (56%) while noncontact injuries were dominant among female players.
In other sports, the incidence rates vary. In skiing, ACL injury represent 30.9 per 100,000 skiers per day[5]. While in basketball, 17 per 100,000 athletic exposures were repoted between 1989 and 2004 in the USA[6].
Instability, knee OA, inability to return to sport and recurrent injuries are among the short and long term list of consequences that follow ACL injury.
Considerations Before Desigining a Rehabilitation Program[edit | edit source]
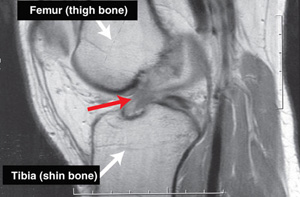
ACL injury is often a complex presentation with other associated damages such as mensicus injury, medial collateral injury, bone contusion and chondral injury.
The highest recurrence rates of ACL injury and the fact that many players may not be able to return to their proir level of performance challenges the rehabilitation strategy. It is recommended that oucome measures should not be based on a timely manner, instead a clearence to return to sport should be given according to performance levels as we will discuss later.
Since it is not a simple injury, a multidisciplinary team is needed to help athletes recover and maintain their level of performance. Inaddition to physiotherapy you should keep communication channels open with the following professionals and know when to refer your patient to them:
- Orthopedic Surgeon to track your patient progress.
- Sports Psychologist; when he athletes are struggling to return to sport.
- Sports Nutritionist; the time spent away from the field has devastating consequences on muscle mass and body composition. An individualized nutrition plan is also needed to facilitate recovery and return to sport.
Acute Management Goals[edit | edit source]
The acute management after surgery takes from 4-6 weeks and has its specific goals that need to be considered:
- Joint Homeostasis
- Scar management
- ROM in all directions
- Quadriceps independent work and terminal extension range
- A long term plan for 6-9 months of recovery. To draw a map for your patient and explain the process to them, engage them in setting goals and also to det time-specific milestones that would help in desigining your program.
Protection of the post surgical repair is done by the following:
- Limiting ROM to 90° until femoral and/or adductor nerve block is gone (usually it takes 48-72 hours). Once patient can report accurate sensation, ROM is allowed with regard to patient comfort.
- Bracing in a mobilizer until femoral/adductor nerve block is off then change to a C-hinge knee brace for 3-7 days or until the patient is able to perform terminal knee extension, depending on the time you see your patient.
- Partial Weight Bearing is recommended for two weeks after surgery to minimize swelling and inflammation and allow full resolution of effusion.
- Stationary Bike is introduced on day 10, depending on joint mobility.
- Complete weight bearning strength training is delayed up to 6 weeks.
Homeaostasis[edit | edit source]
References[edit | edit source]
- ↑ Rochcongar P, Laboute E, Jan J, Carling C. Ruptures of the anterior cruciate ligament in soccer. International journal of sports medicine. 2009 May;30(05):372-8.
- ↑ Brophy R, Silvers HJ, Gonzales T, Mandelbaum BR. Gender influences: the role of leg dominance in ACL injury among soccer players. British journal of sports medicine. 2010 Jun 1:bjsports51243.
- ↑ Hewett TE, Myer GD, Ford KR, Heidt Jr RS, Colosimo AJ, McLean SG, Van den Bogert AJ, Paterno MV, Succop P. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. The American journal of sports medicine. 2005 Apr;33(4):492-501.
- ↑ Brophy RH, Stepan JG, Silvers HJ, Mandelbaum BR. Defending puts the anterior cruciate ligament at risk during soccer: a gender-based analysis. Sports health. 2015 May;7(3):244-9.
- ↑ Demirağ B, Oncan T, Durak K. An evaluation of knee ligament injuries encountered in skiers at the Uludag Ski Center. Acta orthopaedica et traumatologica turcica. 2004;38(5):313-6.
- ↑ Mihata LC, Beutler AI, Boden BP. Comparing the incidence of anterior cruciate ligament injury in collegiate lacrosse, soccer, and basketball players: implications for anterior cruciate ligament mechanism and prevention. The American journal of sports medicine. 2006 Jun;34(6):899-904.