Lumbar Conditions in Ballet Dancers: Difference between revisions
No edit summary |
Diana Yang (talk | contribs) mNo edit summary |
||
| Line 6: | Line 6: | ||
Dance medicine literature is small and very heterogeneous with a mostly ballet focus.<ref name=":7" /> Overuse injuries in the spine is generally regarded as the second most effected region with the lower limbs being the first in ballet dancers,<ref>Sobrino, F.J. & Guillen, P. (2017) Overuse Injuries in Professional Ballet. ''Sport and Exercise Science''. </ref> these injuries are typically presented as pain to the affected region.<ref name=":8" /> | Dance medicine literature is small and very heterogeneous with a mostly ballet focus.<ref name=":7" /> Overuse injuries in the spine is generally regarded as the second most effected region with the lower limbs being the first in ballet dancers,<ref>Sobrino, F.J. & Guillen, P. (2017) Overuse Injuries in Professional Ballet. ''Sport and Exercise Science''. </ref> these injuries are typically presented as pain to the affected region.<ref name=":8" /> | ||
Certain movements in ballet are especially prone to put additional strain on the lower back in both female and male dancers. While male dancers are generally expected to meet tougher athletic demands such as lifting their partners, female dancers are usually required to meet stricter technical demands.<ref name=":8" /> Excessive stress on the lumbar spine during lifts and hyperlordosis in the back to compensate for hip extension contribute to the strain in the musculoskeletal structures in the lumbar region.<ref name=":1" /> <ref name=":2" /><ref name=":7" /><ref name=":9">Gelabert, R. (1986) Dancers’ Spinal Syndromes. ''The Journal of Orthopaedic and Sports Physical Therapy''. 7 (4), 180–191.</ref><ref>Skallerud, A., Brumbaugh, A., Fudalla, S., Parker, T., Robertson, K. & Pepin, M.-E. (2022) Comparing Lumbar Lordosis in Functional Dance Positions in Collegiate Dancers with and without Low Back Pain. ''J Dance Med Sci''. 26 (3), 191–201.</ref> | Certain movements in ballet are especially prone to put additional strain on the lower back in both female and male dancers. While male dancers are generally expected to meet tougher athletic demands such as lifting their partners, female dancers are usually required to meet stricter technical demands.<ref name=":8" /> Excessive stress on the lumbar spine during lifts and hyperlordosis in the back to compensate for hip extension contribute to the strain in the musculoskeletal structures in the lumbar region.<ref name=":1" /><ref name=":2" /><ref name=":7" /><ref name=":9">Gelabert, R. (1986) Dancers’ Spinal Syndromes. ''The Journal of Orthopaedic and Sports Physical Therapy''. 7 (4), 180–191.</ref><ref>Skallerud, A., Brumbaugh, A., Fudalla, S., Parker, T., Robertson, K. & Pepin, M.-E. (2022) Comparing Lumbar Lordosis in Functional Dance Positions in Collegiate Dancers with and without Low Back Pain. ''J Dance Med Sci''. 26 (3), 191–201.</ref> | ||
=== <big>Lumbar Conditions in Ballet Dancers</big> === | === <big>Lumbar Conditions in Ballet Dancers</big> === | ||
[[File:Turnout.jpg|thumb|'''Figure 1'''. Turnout in ballet requiring maximal external rotation at the hips.]] | [[File:Turnout.jpg|thumb|'''Figure 1'''. Turnout in ballet requiring maximal external rotation at the hips.|295x295px]] | ||
Turnout (Figure 1), the first position in ballet, requires maximal hip external rotation. When the tightness of the psoas muscle limits the degree of external rotation at the hip, dancers will attempt to compensate by increasing hip flexion and thus lumbar lordosis in. | Turnout (Figure 1), the first position in ballet, requires maximal hip external rotation. When the tightness of the psoas muscle limits the degree of external rotation at the hip, dancers will attempt to compensate by increasing hip flexion and thus lumbar lordosis in. | ||
| Line 27: | Line 27: | ||
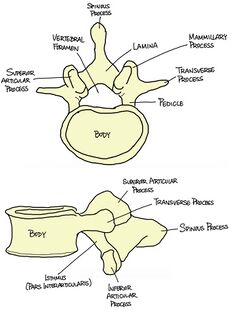
[[File:Lumbar Vertebra drawing.jpg|thumb|'''Figure 3'''. Vertebral body of a Lumbar Vertebra.|310x310px]] | [[File:Lumbar Vertebra drawing.jpg|thumb|'''Figure 3'''. Vertebral body of a Lumbar Vertebra.|310x310px]] | ||
The [[Lumbar Anatomy|lumbar]] spine consists of 5 vertebrae, situated between the [[Thoracic Anatomy|thoracic spine]] and the [[sacrum]]. Each vertebra consists of a vertebral body and a neural arch, with the body anterior to the arch (Figure 3). When viewed superiorly, the body is wider transversely, and the neural arch is triangular shaped (especially distinguishable at L5). The facet angles range from 120 – 150 degrees relative to the sagittal plane, and consistently decrease from L1 to L5. <ref>Ebraheim, N.A., Hassan, A., Lee, M. & Xu, R. (2004) Functional anatomy of the lumbar spine. ''Seminars in Pain Medicine''. 2 (3), 131–137.</ref> | The [[Lumbar Anatomy|lumbar]] spine consists of 5 vertebrae, situated between the [[Thoracic Anatomy|thoracic spine]] and the [[sacrum]]. Each vertebra consists of a vertebral body and a neural arch, with the body anterior to the arch (Figure 3). When viewed superiorly, the body is wider transversely, and the neural arch is triangular shaped (especially distinguishable at L5). The facet angles range from 120 – 150 degrees relative to the sagittal plane, and consistently decrease from L1 to L5. <ref>Ebraheim, N.A., Hassan, A., Lee, M. & Xu, R. (2004) Functional anatomy of the lumbar spine. ''Seminars in Pain Medicine''. 2 (3), 131–137.</ref> | ||
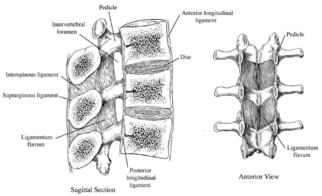
As with the rest of the spinal column, the articulations consist of the intervertebral disc anteriorly, and a pair of facet joints posteriorly. The ligaments (Figure 4) stabilize the spine as one unit, including the following major ligaments:[[File:Lumbar Ligaments.png|thumb|'''Figure 4'''. Major ligaments of the lumbar spine (Ebraheim et al., 2014).|left|322x322px]] | |||
As with the rest of the spinal column, the articulations consist of the intervertebral disc anteriorly, and a pair of facet joints posteriorly. The ligaments (Figure 4) stabilize the spine as one unit, including the following major ligaments | |||
* [[Anterior longitudinal ligament]]: originating from the skull and inserting into the upper part of the sacrum, connecting the whole anterior aspect of the vertebral bodies and intervertebral discs | * [[Anterior longitudinal ligament]]: originating from the skull and inserting into the upper part of the sacrum, connecting the whole anterior aspect of the vertebral bodies and intervertebral discs | ||
* [[Posterior longitudinal ligament]]: originating from the occipital bone and inserting into the sacrum, connecting the whole posterior aspect of the vertebral bodies and discs | * [[Posterior longitudinal ligament]]: originating from the occipital bone and inserting into the sacrum, connecting the whole posterior aspect of the vertebral bodies and discs | ||
Revision as of 15:30, 18 May 2023
Introduction[edit | edit source]
Ballet dancers are both highly skilled artists and elite athletes.[1] Due to their intense and highly repetitive nature of movement patterns, ballet dancers are often at significant risk for injury,[2] especially overuse injuries (as opposed to traumatic injuries) in the lower extremities and the lumbar region. Many of the injuries trace back to technique error, or external factors such as the footwear and the stage.[2][3][4][5][6]
The number of overuse injuries are seen more in female dancers than their male counterpart, this is mostly due to the higher technical requirements, leading to higher repetition of physically demanding movements in rehearsals and performances, making the female dancers more prone to overuse injuries (Sobrino & Guillén, 2017; Sobrino, Cuadra & Guillén, 2015).[7][8]
Dance medicine literature is small and very heterogeneous with a mostly ballet focus.[6] Overuse injuries in the spine is generally regarded as the second most effected region with the lower limbs being the first in ballet dancers,[9] these injuries are typically presented as pain to the affected region.[8]
Certain movements in ballet are especially prone to put additional strain on the lower back in both female and male dancers. While male dancers are generally expected to meet tougher athletic demands such as lifting their partners, female dancers are usually required to meet stricter technical demands.[8] Excessive stress on the lumbar spine during lifts and hyperlordosis in the back to compensate for hip extension contribute to the strain in the musculoskeletal structures in the lumbar region.[1][4][6][10][11]
Lumbar Conditions in Ballet Dancers[edit | edit source]
Turnout (Figure 1), the first position in ballet, requires maximal hip external rotation. When the tightness of the psoas muscle limits the degree of external rotation at the hip, dancers will attempt to compensate by increasing hip flexion and thus lumbar lordosis in.
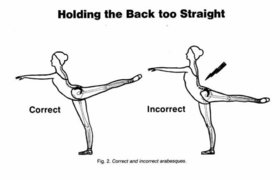
Similarly, in movements such as arabesque (Figure 2) that require extension at the hip. If there is insufficient hip extension or the spine is too straight, compensatory techniques such as increasing lumbar lordosis will be employed, resulting in excessive torsion strain.
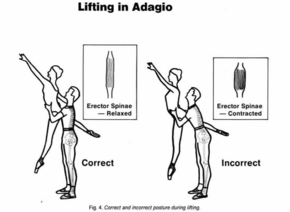
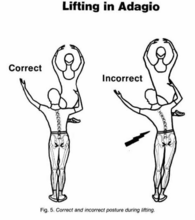
Both mechanisms will lead to the shortening of the erector spinae, and thoracolumbar fascia, contributing to a hyperlordotic posture in the lumbar region. [4][12] In male dancers, excessive lumbar lordosis is seen during lifts of another dancer, especially away from their center of gravity.[4][10]
Incorrect technique and posture adding excessive stress to the lumbar spine in ballet dancers can result in a hyperlordotic posture, which can lead to low back pain (LBP),[3] and joint trauma[13] such as spondylolysis, or trauma to the pars interarticularis, the intervertebral discs, and the facet joints. [4] It predisposes dancers to muscle spasm, piriformis syndrome, and other spinal conditions like spondylolisthesis.[6]
This page will focus on the following three conditions in the lumbar region:
- Hyperlordosis
- Spondylolysis
- Spondylolisthesis
Clinically Relevant Anatomy[edit | edit source]
The lumbar spine consists of 5 vertebrae, situated between the thoracic spine and the sacrum. Each vertebra consists of a vertebral body and a neural arch, with the body anterior to the arch (Figure 3). When viewed superiorly, the body is wider transversely, and the neural arch is triangular shaped (especially distinguishable at L5). The facet angles range from 120 – 150 degrees relative to the sagittal plane, and consistently decrease from L1 to L5. [14]
As with the rest of the spinal column, the articulations consist of the intervertebral disc anteriorly, and a pair of facet joints posteriorly. The ligaments (Figure 4) stabilize the spine as one unit, including the following major ligaments:
- Anterior longitudinal ligament: originating from the skull and inserting into the upper part of the sacrum, connecting the whole anterior aspect of the vertebral bodies and intervertebral discs
- Posterior longitudinal ligament: originating from the occipital bone and inserting into the sacrum, connecting the whole posterior aspect of the vertebral bodies and discs
- Ligamentum flava: present in between the laminae of each vertebra
- Supraspinous and Interspinous ligaments: connecting the spinous processes of each vertebra
The lordotic curvature of the lumber spine is formed because the sacrum is tilt forwards and inclined downwards, so to compensate for the inclination angle of the sacrum, the spine must assume a lordotic curve. Moreover, the wedge shaped lumbosacral interverbal disc and L5 vertebral body contribute to a forward inclination at the L5/S1 joint. As a result of the inclination, the anterior longitudinal ligament is stretched, and the intervertebral discs are compressed slightly.[15]
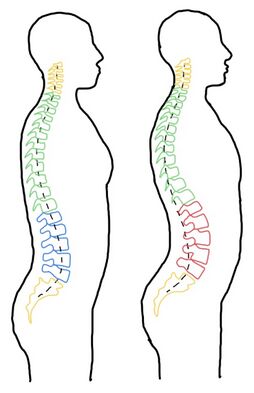
The mean angle of lumbar lordosis is said to be around 48-61 degrees.[16] Lumbar hyperlordosis is indicated when the angle is greater than 68 degrees.[15] Figure 5 demonstrate the comparison between the normal lumbar curvature and an increased lordosis in the lumbar spine. The hyperlordotic and hyperextended positions implicate the lumbar spine is more vulnerable to microtrauma to the pars interarticularis, intervertebral discs, and the facet joints. This can subsequently contribute to overuse or stress fractures in the lumbar spine. In the hyperlordotic position, the erector spinae muscle in the back shortens, contributing to the increasing lumbar lordosis in a standing position.[10]
Clinical Presentation[edit | edit source]
| Condition | Subjective Presentation | Objective Presentation | Diagnosis |
|---|---|---|---|
| Spondylolysis and Spondylothesis |
|
|
|
| Hyperlordosis |
|
|
|
Epidemiology[edit | edit source]
Hyperlordosis[edit | edit source]
Relevant Literature[edit | edit source]
The extreme ranges of motion required during dancing and gymnastics may contribute to the participants' high lumbar lordosis. [17] Ambegaonkar (2014) examined 17 female dancers using 2-dimensional sagittal plane photographs and the Watson Maconncha Posture Analysis Instrument. A strength of this study are the experimental methods due to be found reliable and accurate in previous studies and are commonly used in a clinical and research setting for assessing lumbar lordosis. Results showed among dancers, 9 had significant lumber lordosis deviations and 5 had moderate deviations. This shows the extreme ranges of motion required during the technique when dancing may contribute to the participants high lumbar lordosis. However, the limitation of this study entails focusing that it only examined female dancers, therefore the findings may not be applicable to other populations as well as not investigating the influence of age, training onset, training regimes, or other factors on lumbar lordosis. Additionally, the study only examined lumbar lordosis levels at one point in time, future research could enquire longitudinal studies to determine if there is a relationship between lumbar lordosis levels and lumbar injury incidence in dancers. Another study by Byran and Smith (1992) discusses the patterns of weakness and tightness in certain muscle groups in ballet dancers that contribute to hyperlordotic posture such as lumbodorsal fascia and hamstring can occur during the growth spurt phase of development. This could be common as the average starting ages ranging from 5 to 11 years old with full time training typically beginning around 14 to 15 years old [18] [19] Due to the demands of dance involve extreme and repetitive lumber hyperextension alongside areas of weak and tight muscles during their growth spurt where full time intense training begins, may result in a hyperlordotic posture.[20] However, the limitation of this study entails focusing that it only examined female dancers, therefore the findings may not be applicable to other populations.
Spondylolysis[edit | edit source]
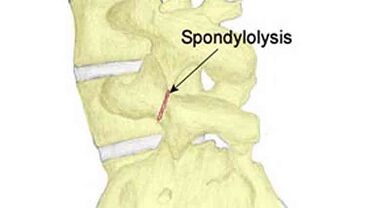
Spondylolysis is an isolated defect in the neural arch of the vertebrae [21]. It refers to a stress fracture of the pars interarticularis of a vertebra in the spine. Lumbar spondylolysis results from repetitive, mechanical stress on the lower back, however, biological factors are not ruled out [21]. There are congenital factors such as spina bifida occulta and exaggerated lumbar lordosis that predispose individuals to pars interarticularis fractures [22]. The defect can either be asymptomatic or associated with significant low back pain [23].
The pars interarticularis is the weakest area of the vertebrae, making it the most susceptible to injury. Spondylolysis can occur in one of the pars interarticularis or in both of them in one vertebra, meaning that is can be unilateral or bilateral [24]. The vast majority of spondylolitic defects occur at the L5 level (85-95%) and L4 being the second most commonly involved level (5-15%)[25]. Spondylolysis is found in 3-10% of the general population [26]. It is of of the most common types of skeletal injury in paediatric dancers and gymnasts.
The most common symptom of spondylolysis is back pain [27], usually with an incidious onset and may be referred to the buttocks or posterior aspect of the thigh. The pain can be brought on by loading the lumbar spine in combination with lumbar extension and rotation movements [28]. The diagnosis of of spondylolysis cannot be made with physical examination alone [28]. Two-view plain film x-rays are typically used for initial diagnosis as they are inexpensive and relatively low in radiation [29].
Spondylolisthesis[edit | edit source]
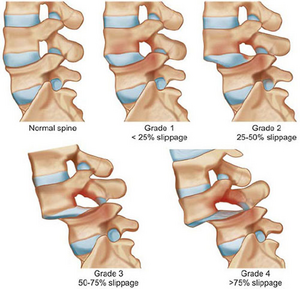
Spondylolisthesis is closely related to Spondylolysis. It refers to the forward slip of the vertebrae [6]. This is due to stress fractures (Spondylolysis) causing a weakening of the vertebral column to the extent that the vertebrae cannot maintain its position, resulting in the vertebrae to move outside of its normal anatomical place [30]. Spondylolisthesis can be defined by four grades, grade I is when there 1 to 25% slippage, grade II up to 50% slippage and grade III is up to 75% in slippage and lastly grade IV is when there is greater than 75% slippage[31].
Wiltse et al developed six classifications for Spondylolisthesis and dancers are likely to develop grade II Isthmic spondylolithesis. Grade II is further divided into three parts, type A which is fatigue fractures of the pars, type B which refers to elongated but intact pars and type C which is acute fracture of the pars. [32]Grade II Isthmic spondylolithesis is greatly associated with flexion, twisting and most notably hyperextension activities and movement repetitively performed by ballet dancers. [33]Symptoms of dull aches in the lower back and radicular pain into the glutes and anterior thigh usually accompany Spondylolisthesis and dancers who experience this, usually can not identify an exactly when the initial injury occurred[6]. Additionally, stigma and dance culture means that injured dancers often delay seeking medical help and "dance through" the pain.[34]
Spondylolysis and Spondylolisthesis Relevant Literature[edit | edit source]
The literature shows a fourfold increase in spondylolysis and spondylolisthesis in adolescent dancers when compared with the general population[35]. This incidence is mainly caused by the repetitive microtrauma and shear forces of hyperextension into positions and the poor mechanics and alignment often used by young dancers to obtain these hyperextension positions. A review found that 590 out of the 4243 athletes (13.9%) had a radiological diagnosis of spondylolysis [36]. It recommended a radiological examination of the lumbar spine in symptomatic athletes who are considered to be at high risk of developing spondylolysis. The review included both male and female athletes meaning that it has high population validity. However, this review was conducted a significant amount of time ago. Therefore, the prevalence of spondylolysis in elite athletes may have changed in recent years. Another limitation of this review was the age range of patients included in the review was 15-27 years, therefore, it is not representative of elite athletes outside of this age range.
Management Recommendations[edit | edit source]
Strengthening[edit | edit source]
Positioning[edit | edit source]
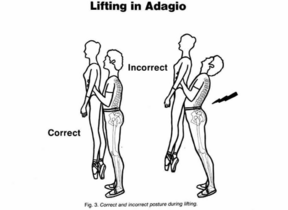
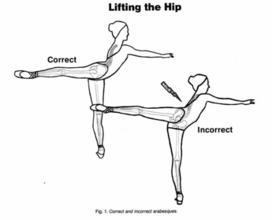
Gelabert (1986) [10] explains that in a ballet dancer, if the iliofemoral ligament in front of the hip joint restricts hypertension of the leg and the external rotation at the hip socket, the dancer will often disguise this limitation by lifting the hip to the side like shown in Figure 1. The repetition of this incorrect movement has a massive effect on low back afflictions and multiplies when the back is kept too straight shown in Figure 2. This is performed instead of the correct position by increasing the inclination of the pelvis forward as the leg raises backwards.
This study shows in 100 cases of low back syndromes in ballet dancers, 45% are related to those who lift at the hip in arabesque and other movements of the leg backwards and 25% of those who forcefully try to raise their leg above 90 degrees while keeping their back too straight. It has been found that these injuries will arise faster with individuals with longer backs and tight hip muscles and ligaments, which is often found in male physiques. Alongside this, spasm of the lumbar muscles occurs usually from faults of technique in hyperextension. Tension within the upper spine and chest muscles will be reflected in the thoracic region and to lumbar, pelvis and to the legs, increasing fatigue which causes inefficient breathing patterns and inclining the spine to strain. The impact of this is instrumental to male dancers when lifting, this is shown in Figure 3,4, and 5, it can lead to weak muscle pull, inefficient energy use and an increased risk of low back strain.
Stretching[edit | edit source]
Conclusion[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 Allen, N., Nevill, A., Brooks, J., Koutedakis, Y. & Wyon, M. (2012) Ballet injuries: Injury incidence and severity over 1 year. Journal of Orthopaedic and Sports Physical Therapy. 42 (9), 781–790.
- ↑ 2.0 2.1 Gamboa, J.M., Robert, L.A. & Fergus, A. (2008) Injury patterns in elite preprofessional ballet dancers and the utility of screening programs to identify risk characteristics. The Journal of orthopaedic and sports physical therapy. 38 (3), 126–136.
- ↑ 3.0 3.1 Pinnelli, M., Pulcinelli, M., Carnevale, A., Di Tocco, J., Massaroni, C., Schena, E., Longo, U.G. & Denaro, V. (2022) A Wearable System for Detecting Lumbar Hyperlordosis in Ballet Dancers: Design, Development and Feasibility Assessment. 2022 IEEE International Workshop on Metrology for Industry 4.0 and IoT, MetroInd 4.0 and IoT 2022 - Proceedings. 277–282.
- ↑ 4.0 4.1 4.2 4.3 4.4 Milan, K.R. (1994) Injury in Ballet: A Review of Relevant Topics for the Physical Therapist. J Orthop Sports Phys Ther. 19 (2), 121–129.
- ↑ Cejudo, A., Gómez-Lozano, S., de Baranda, P.S., Vargas-Macías, A. & Santonja-Medina, F. (2021) Sagittal Integral Morphotype of Female Classical Ballet Dancers and Predictors of Sciatica and Low Back Pain. International Journal of Environmental Research and Public Health. 18 (9).
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Gottschlich, L.M. & Young, C.C. (2011) Spine injuries in dancers. Current Sports Medicine Reports. 10 (1), 40–44.
- ↑ Sobrino, F.J., Cuadra, C. de la & Guillén, P. (2015) Overuse Injuries in Professional Ballet Injury-Based Differences Among Ballet Disciplines. The Orthopaedic Journal of Sports Medicine. 3 (6), 1–7.
- ↑ 8.0 8.1 8.2 Sobrino, F.J. & Guillén, P. (2017) Overuse Injuries in Professional Ballet: Influence of Age and Years of Professional Practice. Orthopaedic Journal of Sports Medicine. 5 (6).
- ↑ Sobrino, F.J. & Guillen, P. (2017) Overuse Injuries in Professional Ballet. Sport and Exercise Science.
- ↑ 10.0 10.1 10.2 10.3 Gelabert, R. (1986) Dancers’ Spinal Syndromes. The Journal of Orthopaedic and Sports Physical Therapy. 7 (4), 180–191.
- ↑ Skallerud, A., Brumbaugh, A., Fudalla, S., Parker, T., Robertson, K. & Pepin, M.-E. (2022) Comparing Lumbar Lordosis in Functional Dance Positions in Collegiate Dancers with and without Low Back Pain. J Dance Med Sci. 26 (3), 191–201.
- ↑ Livanelioglu, A., Otman, S., Yakut, Y. & Uygur, F. (1998) The Effects of Classical Ballet Training on the Lumbar Region. Journal of Dance Medicine & Science. 2 (2), 52–55.
- ↑ Roussel, N.A., Nijs, J., Mottram, S., Van Moorsel, A., Truijen, S. & Stassijns, G. (2009) Altered lumbopelvic movement control but not generalized joint hypermobility is associated with increased injury in dancers. A prospective study. Manual Therapy. 14 (6), 630–635.
- ↑ Ebraheim, N.A., Hassan, A., Lee, M. & Xu, R. (2004) Functional anatomy of the lumbar spine. Seminars in Pain Medicine. 2 (3), 131–137.
- ↑ 15.0 15.1 Bogduk, N. (2005) Clinical Anatomy of the Lumbar Spine and Sacrum. 4th edition. Elsevier: Churchill Livingstone.
- ↑ Jentzsch, T., Geiger, J., König, M.A. & Werner, C.M.L. (2017) Hyperlordosis is Associated with Facet Joint Pathology at the Lower Lumbar Spine. Clinical Spine Surgery. 30 (3), 129–135.
- ↑ Ambegoankar, J. P. et al., 2014. Lumbar lordosis in female collegiate dancers and gymnasts. Medical problems of performing artists, 29(4), pp. 189-192.
- ↑ Hutchinson, C. U., Sachs-Ericsson, N. J. & Ericsson, A. K., 2013. Generalizable aspects of the development of expertise in ballet across countries and cultures: a perspective from the expert-performance approach. High Ability Studies, 24(1), pp. 21-47.
- ↑ Bernacki, J. L. et al., 2021. Risk Factors for Lower-Extremity Injuries in Female Ballet Dancers: A Systematic Review. Clinical Journal of Sports Medicine, 31(2), pp. 64-79.
- ↑ Bryan, N. & Smith, B. M., 1992. The ballet dancer. Occup Med: State of the Art Reviews, 7(1), pp. 67-75.
- ↑ 21.0 21.1 Berger, R. G. & Doyle, S. M., 2019. Spondylolysis 2019 update. Current Opinion in Pediatrics, 31(1), pp. 61-68.
- ↑ Watkins, R. G. & Watkins, R. G., 2010. Lumbar Spondylolysis and Spondylolisthesis in Athletes. Seminars in Spine Surgery, 22(4), pp. 210-217.
- ↑ Syrmou, E. et al., 2010. Spondylolysis: A review and reappraisal. Hippokratia Quarterly Medical Journal, 14(1), pp. 17-21.
- ↑ Leone, A. et al., 2011. Lumbar spondylolysis: a review. Skeletal Radiology, Volume 40, pp. 683-700.
- ↑ Standaert, D. C. & Herring, S., 2000. Spondylolysis: a critical review. British Journal of Sports Medicine, Volume 34, pp. 415-422.
- ↑ Lemoine, T. et al., 2018. The prevalence of lumbar spondylolysis in young children: a retrospective analysis using CT. European Spine Journal, Volume 27, pp. 1067-1072.
- ↑ Porter, R. W. & Hibbert, C. S., 1984. Symptoms associated with lysis of the pars interarticularis. Spine, Volume 9, pp. 755-758.
- ↑ 28.0 28.1 Goetzinger, S. et al., 2020. Spondylolysis in Young Athletes: An Overview Emphasizing Nonoperative Management. Journal of Sports Medicine, Volume 2020, pp. 1-15.
- ↑ Miller, R. et al., 2013. A Review of Spondylolysis and Undiagnosed Mechanical Back Pain. Journal of Pediatric Orthopaedics, 33(3), pp. 282-288.
- ↑ https://www.nhs.uk/conditions/spondylolisthesis/
- ↑ Hu, S.S., Tribus, C.B., Diab, M. and Ghanayem, A.J. (2008). Spondylolisthesis and Spondylolysis. JBJS, [online] 90(3), p.656. Available at: https://journals.lww.com/jbjsjournal/pages/articleviewer.aspx?year=2008&issue=03000&article=00025&type=Fulltext [Accessed 18 May 2023].
- ↑ Wiltse, L.L. and Winter, R.B. (1983). Terminology and measurement of spondylolisthesis. The Journal of Bone & Joint Surgery, 65(6), pp.768–772. doi:https://doi.org/10.2106/00004623-198365060-00007.
- ↑ Wiltse, L.L. and Winter, R.B. (1983). Terminology and measurement of spondylolisthesis. The Journal of Bone & Joint Surgery, 65(6), pp.768–772. doi:https://doi.org/10.2106/00004623-198365060-00007.
- ↑ Vassallo, A.J., Pappas, E., Stamatakis, E. and Hiller, C.E. (2019). Injury Fear, Stigma, and Reporting in Professional Dancers. Safety and Health at Work, [online] 10(3), pp.260–264. doi:https://doi.org/10.1016/j.shaw.2019.03.001.
- ↑ Tsirikos, A. & Garrido, E., 2010. Spondylolysis and spondylolisthesis in children and adolescents. Journal of Bone Joint Surgery, 92(6), pp. 741-749.
- ↑ Rossi, F. & Dragoni, S., 2001. The prevalence of spondylolysis and spondylolisthesis in symptomatic elite athletes: radiographic findings. Radiography, Volume 7, pp. 37-42.