The Ageing Foot: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) No edit summary |
||
| (26 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- [[User:Ewa Jaraczewska|Ewa Jaraczewska]] based on the course by [https://members.physio-pedia.com/instructor/helene-simpson/ Helene Simpson] | '''Original Editor '''- [[User: Ewa Jaraczewska|Ewa Jaraczewska]] based on the course by [https://members.physio-pedia.com/instructor/helene-simpson/ Helene Simpson] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
One in four older adults have foot pain.<ref name=":0" /> Foot pain can affect walking and contribute to falling and functional disability in older adults.<ref name=":4">Zhang B, Lu Q. [https://paahjournal.com/articles/10.5334/paah.57/ A current review of foot disorder and plantar pressure alternation in the elderly.] Physical Activity and Health. 2020 Sep 2;4(1).</ref> The aetiology of foot pain is often multifactorial. Foot pain may be caused by musculoskeletal pathologies, as well as vascular and [[Neurological Disorders| Neurological Disorders]],<ref>Oh-Park M, Kirschner J, Abdelshahed D, Kim DDJ. Painful Foot Disorders in the Geriatric Population: A Narrative Review. Am J Phys Med Rehabil. 2019 Sep;98(9):811-819. </ref> but the three major foot problems in older adults are [[Foot Pain|pain]], neuropathy, and deformities.<ref name=":1">Muchna A, Najafi B, Wendel CS, Schwenk M, Armstrong DG, Mohler J. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6647839/pdf/nihms-1041883.pdf Foot Problems in Older Adults Associations with Incident Falls, Frailty Syndrome, and Sensor-Derived Gait, Balance, and Physical Activity Measures.] J Am Podiatr Med Assoc. 2018 Mar;108(2):126-139. doi: 10.7547/15-186. Epub 2017 Aug 30. </ref> The most common orthopaedic deformities in the elderly include [[Hallux Valgus|hallux valgus]], prominent [[Metatarsalgia|metatarsal heads]], and an abnormal medial [[Arches of the Foot|arch]] structure.<ref name=":4" /> Overall, foot deformities and other foot conditions are highly prevalent in adults aged over 65 years,<ref>Helfand AE. Foot problems in older patients: a focused podogeriatric assessment study in ambulatory care. J Am Podiatr Med Assoc. 2004 May-Jun;94(3):293-304. </ref> which is significant as these conditions are associated with frailty and decreased physical activity.<ref name=":1" />This article will discuss age related changes in the foot and suggested therapeutic interventions to improve balance, decrease risk for falls, and prevent or reduce skin and functional changes. It highlights the need for education and remediation regarding footwear advice in older adults. | |||
=== Risk factors === | === Risk factors === | ||
The following are | The following are risk factors for foot problems in older adults: | ||
* Gender (women more frequently than men)<ref name=":0" /><ref name=":2">Simpson H. The Ageing Foot Course. Plus 2022</ref> | * Gender (women are more frequently affected than men)<ref name=":0" /><ref name=":2">Simpson H. The Ageing Foot Course. Plus 2022</ref> | ||
* Obesity<ref name=":1" /> | * Obesity<ref name=":1" /> | ||
* Chronic conditions, including diabetes and osteoarthritis<ref name=":1" /> | * Chronic conditions, including [[diabetes]] and [[osteoarthritis]]<ref name=":1" /> | ||
* Peripheral neuropathy<ref name=":2" /> | * Peripheral neuropathy<ref name=":2" /> | ||
* Neurological disorders (stroke, Parkinson's | * Neurological disorders (e.g. [[stroke]], [[Parkinson's]])<ref name=":1" /> | ||
* Lower extremity oedema (can be related to vascular or cardiac pathology)<ref name=":2" /> | * Lower extremity [[Oedema Assessment|oedema]] (can be related to vascular or cardiac pathology)<ref name=":2" /> | ||
* Inappropriate footwear | * Inappropriate footwear<ref name=":1" /> | ||
* Underlying geriatric syndromes and conditions<ref name=":1" /> | |||
== Age-Related Changes in the Foot == | == Age-Related Changes in the Foot == | ||
| Line 25: | Line 26: | ||
==== Skin ==== | ==== Skin ==== | ||
Weight-bearing activities place specific demands on the skin of the foot's plantar surface. The foot has certain features to accommodate these loads:<ref name=":0" /> the [[Skin|epidermis]] is thicker in the foot compared to other parts of the body; the [[Skin|dermis]] is around 3mm thick and has adipose tissue that can resist sheer forces; and the fingerprint-like pattern of the epidermis helps to generate enough friction during walking.<ref name=":0" /> However, all aspects of the skin change as a person ages. These changes affect not only the superficial skin but also the local vascular response, thermoregulation, sensory perception, and injury response,<ref>Fenske NA, Lober CW. Structural and functional changes of normal ageing skin. J Am Acad Dermatol. 1986 Oct;15(4 Pt 1):571-85. </ref> and they include: | |||
* | * Flattening of the dermo-epidermal junction<ref name=":0">Menz HB. [https://www.karger.com/Article/Pdf/368357 Biomechanics of the ageing foot and ankle: a mini-review.] Gerontology. 2015;61(4):381-8.</ref> | ||
* | * Decreased contact between the dermis and epidermis, which causes the skin to separate along this interface<ref name=":3">Levine JM. [https://journals.lww.com/aswcjournal/FullText/2020/01000/Clinical_Aspects_of_Aging_Skin__Considerations_for.4.aspx Clinical aspects of ageing skin: Considerations for the wound care practitioner]. Advances in skin & wound care. 2020 Jan 1;33(1):12-9.</ref> | ||
* | * Loss of elastin and collagen fibres in the dermis. The dermis becomes atrophic. There is a reduction of fibroblasts, and the collagen becomes disorganised.<ref name=":3" /> The remaining collagen fibres become thicker and stiffer.<ref>Smith L. Histopathologic characteristics and ultrastructure of ageing skin. Cutis. 1989 May;43(5):414-24. </ref> | ||
* | * Limited ability by the dense collagen to recoil, which leads to increased compression and development of hyperkeratosis (corns and calluses)<ref>Periyasamy R, Anand S, Ammini AC. The effect of ageing on the hardness of foot sole skin: a preliminary study. Foot (Edinb). 2012 Jun;22(2):95-9.</ref> | ||
* | ** Hyperkeratosis is defined as increased thickness of the outer layer of the skin<ref>Farci F, Mahabal GD. Hyperkeratosis. [Updated 2022 May 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: <nowiki>https://www.ncbi.nlm.nih.gov/books/NBK562206/</nowiki></ref> | ||
* | * Alteration in the mechanical properties of the plantar skin, leading to increased hardness<ref name=":0" /> and dryness | ||
* | * A reduction in the density of sweat glands, which contributes to impaired thermoregulation<ref name=":0" /><ref name=":3" /> | ||
* | * Loss of subcutaneous fat and decreased dermal vascularity, leading to poor thermoregulation<ref name=":3" /> | ||
Overall, the thickening of the exterior layer of the skin and presence of calluses may | * Reduced sensation to touch, pressure, and vibration due to decreased mechanoreceptors (Meissner and Pacini corpuscles)<ref name=":3" /> | ||
Overall, the thickening of the exterior layer of the skin and the presence of calluses may lead to the development of plantar lesions, causing severe pain and disability. The best management strategies are custom-made orthotics, which support the medial arch and unload the metatarsal heads.<ref name=":2" /> | |||
==== Soft Tissue ==== | ==== Soft Tissue ==== | ||
The role of the plantar soft tissue is to protect underlying blood vessels and nerves and to reduce the shear forces that occur while walking. Ageing has a direct impact on the foot's soft tissues, causing progressive stiffness. In particular, it affects the tissue at the big toe, first, third, and fifth metatarsal heads, and the heel.<ref>Kwan RL, Zheng YP, Cheing GL. The effect of ageing on the biomechanical properties of plantar soft tissues. Clin Biomech (Bristol, Avon). 2010 Jul;25(6):601-5.</ref> The metatarsal pad becomes slower to recover after being compressed. Similarly, the heel pad dissipates more energy when compressed,<ref name=":0" /> the plantar fascia demonstrates less recoil due to stiffness.<ref>Jha DK, Wongkaewpotong J, Chuckpaiwong B. Effect of Age and BMI on Sonographic Findings of Plantar Fascia. J Foot Ankle Surg. 2022 May 23:S1067-2516(22)00157-0</ref> The consequences of the soft tissue ageing process are:<ref name=":0" /> | |||
* Range of motion reduction (especially in ankle dorsiflexion) | * Range of motion reduction (especially in ankle dorsiflexion) | ||
* Achilles tendon complaints | * [[Achilles Tendon|Achilles tendon]] complaints | ||
* Changes in gait pattern: more pull off vs | * Changes in gait pattern: more pull-off vs pushing-off, less propulsion | ||
* Increased risk of falls | * Increased risk of [[falls]] | ||
==== Range of Motion ==== | ==== Range of Motion ==== | ||
The ageing process | The ageing process affects joint physiology, leading to joint stiffness. Changes include:<ref name=":0" /> | ||
* Reduction in the water content of the cartilage | |||
* Reduction in the synovial fluid volume and proteoglycans | |||
* Bonding of the collagen fibres | |||
A | A decreased ankle dorsiflexion and subtalar joint inversion-eversion range in older adults contribute to their reduced ability to perform dynamic tasks, maintain static standing balance, and perform functional activities.<ref>Hernández-Guillén D, Tolsada-Velasco C, Roig-Casasús S, Costa-Moreno E, Borja-de-Fuentes I, Blasco JM. [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0247885 Association ankle function and balance in community-dwelling older adults.] PloS one. 2021 Mar 4;16(3):e0247885.</ref> | ||
[[File:Hallux valgus 2.jpeg|thumb|Hallux Valgus deformity]] | |||
==== | ==== Muscle Strength ==== | ||
Progressive changes in skeletal muscle mass ([[sarcopenia]]), metabolism and functional capacity are typical in the ageing population.<ref>Shur NF, Creedon L, Skirrow S, Atherton PJ, MacDonald IA, Lund J, Greenhaff PL. [https://www.sciencedirect.com/science/article/pii/S156816372100091X Age-related changes in muscle architecture and metabolism in humans: The potential contribution of physical inactivity to age-related functional decline]. Ageing Research Reviews. 2021 Jul 1;68:101344.</ref> Older adults experience a reduction in the size and number of muscle fibres in their foot muscles. [[Muscle Fibre Types#Type 1|Large, slow-twitch motor]] units develop and [[Muscle Fibre Types#Type 2A|type II fibres]] become denervated. These changes indicate the presence of age-related atrophy, which can be exacerbated by wearing poorly fitting footwear long-term.<ref name=":0" /> The consequences of atrophy of the foot muscles in the elderly include:<ref name=":0" /> | |||
* Decreased ankle | * Decreased ankle plantar flexor strength (causes difficulty rising onto the toes) | ||
* | * Weakness of the toe plantar flexors, which negatively affects the grasping function of the toes during weight-bearing activities (impaired static and dynamic balance and functional ability, increased risk of falls)<ref>Yong-Wook K, Oh-Yun K, Heon-Seock C, Jong-Hyuck W, Chung-Hwi Y, Tae-Ho K. [https://www.jstage.jst.go.jp/article/jpts/23/1/23_1_127/_pdf Comparison of Toe Plantar Flexors Strength and Balancing Ability between Elderly Fallers and Non-fallers]. Journal of Physical Therapy Science 2011; 23 (1): 127-132</ref> | ||
* Development of toe deformities | ** toe grip strength (TGS) decreases by 30% in older patients compared to younger patients <ref>Endo M, Ashton-Miller JA, Alexander NB. Effects of age and gender on toe flexor muscle strength. J Gerontol A Biol Sci Med Sci. 2002 Jun;57(6):M392-7. </ref> | ||
** toe grip weakness has been associated with developing forefoot deformities and disorders <ref>Menz HB, Morris ME, Lord SR. Foot and ankle risk factors for falls in older people: a prospective study. J Gerontol A Biol Sci Med Sci. 2006 Aug;61(8):866-70. </ref> | |||
* Development of toe deformities ([[Hallux Valgus|hallux valgus]] and lesser toe deformities) | |||
** They alter weight distribution under the foot when walking <ref>Mickle KJ, Munro BJ, Lord SR, Menz HB, Steele JR. Gait, balance and plantar pressures in older people with toe deformities. Gait Posture. 2011 Jul;34(3):347-51. | |||
</ref> | |||
*Lower ambulatory performance<ref>Hida T, Harada A. [Fall risk and fracture. Diagnosing sarcopenia and sarcopenic leg to prevent fall and fracture: its difficulty and pit falls]. Clin Calcium. 2013 May;23(5):707-12. Japanese. </ref> | |||
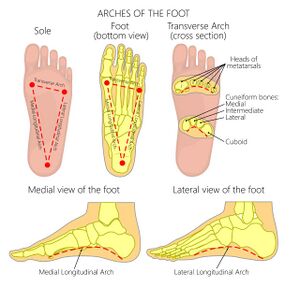
[[File:Arches of the Foot - shutterstock 478538809 smaller.jpg|thumb|Arches of the foot]] | |||
=== Biomechanical Changes === | === Biomechanical Changes === | ||
Age-related changes in soft tissue, range of motion, and muscle strength lead to the following biomechanical changes:<ref name=":0" /> | |||
* The lowering of the medial longitudinal arch | |||
* Reduced midfoot and metatarsal mobility | |||
* Flatter and more dynamically pronated feet | |||
* Planus foot posture | |||
* Less plantarflexed calcaneus at the [[The Gait Cycle|toe-off]] phase of gait | |||
* Less propulsive gait pattern | |||
== Physiotherapy Intervention == | |||
=== General Principles === | |||
# Do not focus on just the foot | |||
# Assess the kinetic chain: look at posture, weight distribution, and centre of mass distribution | |||
# Offer a programme which includes stretching and strengthening | |||
# Use manual techniques to reduce tissue stiffness | |||
# Stimulate the plantar sensors | |||
# Assess footwear | |||
# Be careful when choosing orthotics for medial arch support: do not make the foot stiffer | |||
=== Therapeutic Interventions === | |||
==== Manual Techniques ==== | |||
'''Manual techniques ''' mobilisation of the stiff foot and stimulating the plantar sensory receptors to increase proprioception and improve balance.<ref name=":2" /> | |||
Mobilisation techniques can be one or more of the following: | |||
* Mobilisation with movement: application of gentle pain-free overpressure to an end-range movement<ref>Abassi M, Whiteley R. [https://ijspt.scholasticahq.com/article/25544-serial-within-session-improvements-in-ankle-dorsiflexion-during-clinical-interventions-including-mobilization-with-movement-and-a-novel-manipulation-i Serial Within-Session Improvements in Ankle Dorsiflexion During Clinical Interventions Including Mobilization-With-Movement and A Novel Manipulation Intervention – A Case Series.] IJSPT. 2021;16(4):1158-1168.</ref> | |||
* Anterior/posterior talocrural joint mobilisation in weight-bearing and non-weight-bearing positions, which aims to for improving DF range of motion <ref name=":6">Shashua A, Flechter S, Avidan L, Ofir D, Melayev A, Kalichman L. [https://www.jospt.org/doi/epdf/10.2519/jospt.2015.5155 The effect of additional ankle and midfoot mobilizations on plantar fasciitis: a randomized controlled trial.] J Orthop Sports Phys Ther. 2015 Apr;45(4):265-72. </ref> | |||
* Subtalar joint mobilisation for eversion and inversion<ref name=":6" /> | |||
* Mid-tarsal mobilisation for pronation and supination of the midfoot<ref name=":6" /> | |||
Plantar-sensory treatments may include the following:<ref name=":7">Hu X, Liao J, Hu X, Zeng Z, Wang L. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10298754/pdf/pone.0287689.pdf Effects of plantar-sensory treatments on postural control in chronic ankle instability: A systematic review and meta-analysis.] PLoS One. 2023 Jun 27;18(6):e0287689.</ref> | |||
* Plantar massage | |||
* [[Vibration|Whole-body vibration]] | |||
* Textured surface-stimulation treatment | |||
According to Hu et al.<ref name=":7" />, patients with chronic ankle instability may have better postural control after applying plantar-sensory treatments. Plantar massage and long-term whole-body vibration were found to be the most effective. | |||
A randomized clinical trial by McKeon and Wikstrom<ref>McKeon PO, Wikstrom EA. The effect of sensory-targeted ankle rehabilitation strategies on single-leg centre of pressure elements in those with chronic ankle instability: A randomized clinical trial. J Sci Med Sport. 2019 Mar;22(3):288-293.</ref>, found that sensory-targeted ankle rehabilitation strategies improved single-leg postural control. One treatment was sufficient for the change to occur. However, it did not offer a long-lasting effect. | |||
==== Stretching ==== | |||
Calf muscle stretching is recommended to reduce pressure on the forefoot. | |||
The | The following complications may be associated with an increased forefoot pressure:<ref name=":8">Macklin K, Healy A, Chockalingam N. The effect of calf muscle stretching exercises on ankle joint dorsiflexion and dynamic foot pressures, force and related temporal parameters. Foot (Edinb). 2012 Mar;22(1):10-7. </ref> | ||
* excessive pressure on the plantar aspect of the forefoot | |||
* an increased plantar pressure due to premature forefoot with ground contact | |||
* limited arterial perfusion to the forefoot plantar tissue for a prolonged time could increase the risk of ulceration or delayed foot ulcer healing | |||
Calf muscles stretching outcomes:<ref name=":8" /> | |||
* several weeks of calf muscle stretch training improves ankle joint flexibility and dorsiflexion range of motion | |||
* reduction in the pathological forefoot pressures | |||
* improvement in dynamic gait pattern | |||
==== Strengthening of the Foot Intrinsic Muscles ==== | |||
'''Strengthening''': toe strengthening exercises to improve the strength of the intrinsic muscles of the foot, increase the stability of the arch, and improve the toe-off phase of gait and balance during ambulation. | |||
== | The roles of the intrinsic muscles of the foot include the following:<ref name=":9">Karimzadeh A, Kouhzad Mohammadi H, Mehravar M, Zahednejad S, Taheri N, Sadeghi M. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9731073/pdf/JFMPC-11-5205.pdf The effects of intrinsic foot muscles strengthening exercises on foot kinetic parameters in pronated foot subjects during forward jump landing.] J Family Med Prim Care. 2022 Sep;11(9):5205-5210.</ref> | ||
* stabilise the foot during balance on one foot | |||
* support the medial longitudinal arch | |||
* maintain concavity during walking | |||
* stabilise the tarsal and metatarsal bones | |||
* control the amount and speed of pronation of the foot | |||
Examples of toe strengthening exercises include using toes to scrunch up the towel while the rest of the foot remains in contact with the ground. <ref name=":9" /> | |||
==== Footwear and Orthotics ==== | |||
'''Footwear assessment''': | |||
Ill-fitting shoes are one of the major underlying causes of foot problems in the older population.<ref>Hijmans JM, Geertzen JH, Dijkstra PU, Postema K. A systematic review of the effects of shoes and other ankle or foot appliances on balance in older people and people with peripheral nervous system disorders. Gait Posture. 2007 Feb;25(2):316-23. </ref> | |||
* Tight footwear can lead to callus formations or corns with skin hyperkeratosis and ulceration. <ref>Menz HB, Morris ME. Footwear characteristics and foot problems in older people. Gerontology. 2005 Sep-Oct;51(5):346-51. </ref> | |||
* Tight and narrow footwear is linked to the development of hallux valgus deformity, or bunion. | |||
* Dorsal foot pain, as one of the symptoms of lesser toe deformities, such as hammertoes, tends to get worse with ill-fitting footwear. | |||
O'Rourke et al.<ref name=":5">O’Rourke B, Walsh ME, Brophy R, Vallely S, Murphy N, Conroy B, Cunningham C, Horgan NF. [https://bmcgeriatr.biomedcentral.com/articles/10.1186/s12877-020-1448-9 Does the shoe fit? Characterising ill-fitting footwear among community-dwelling older adults attending geriatric services: an observational cross-sectional study]. BMC geriatrics. 2020 Dec;20(1):1-8.</ref> found that older adults often wear incorrectly fitting shoes or shoes with unsafe features, like slippers. Wearing slip-on slippers means the toe must grab even more to hang onto the slipper. This can contribute to the drop of the medial arch and the development of hammer toes.<ref name=":2" /> | |||
'''Footwear modification:''' | |||
* Soft to cushion the foot and supportive to prevent the foot from collapsing. | |||
* Wider and higher-toe box shoes. | |||
* Foot inserts improve arch support, facilitate balance and decrease the width of the foot during weight-bearing manoeuvres. <ref>Bapirzadeh K, Jamali A, Forghany S, Nester c, Tavakoli S, Hemmati F. [https://jfootankleres.biomedcentral.com/articles/10.1186/1757-1146-7-S1-A19 The effect of three different insoles on balance in people with functional ankle instability]. J Foot Ankle Res2014; 7 (Suppl 1), A19.</ref> | |||
* Metatarsal pads and splits can help to limit the need for extra-depth shoes. | |||
* Higher collars offer better support for balance. | |||
* Extra-depth shoes are recommended for hammertoes or mid-foot arthrosis. | |||
* Low-heeled footwear reduces the risk of falls. | |||
* Athletic shoes and sneakers are associated with the lowest fall risk. | |||
* Slip-resistant soles are recommended inside and outside the household to reduce the risk of falls. | |||
'''Orthotics:''' | |||
'''[[Introduction to Orthotics]]''': collaboration with an orthotist to make a custom-made orthosis that supports the medial arch without increasing foot stiffness. The proper orthotics should allow for increased shock absorption capacity in the foot. | |||
# | * Customised foot orthosis with medial longitudinal and transverse arch supports on the plantar pressure redistributes plantar pressure and contact area and enhances the functional support of the mid-foot. <ref>Chen H-Y, Peng H-T, Chang C-K, Wang F-T, Yen C-H, Wang T-Y, Chuang H-C, Chiu F-Y, Song C-Y. [https://www.mdpi.com/2076-3417/12/15/7593 Immediate Effect of Customized Foot Orthosis on Plantar Pressure and Contact Area in Patients with Symptomatic Hallux Valgus.] Applied Sciences. 2022; 12(15):7593.</ref> | ||
* Rigid medial arch support orthoses provide better feedback to improve stability in flat foot patients. <ref>Setyawan D, Septiani AE, Sari KIU. COMPARISON FOR THE USED OF RIGID MEDIAL ARCH SUPPORT AND FLEXIBLE MEDIAL ARCH SUPPORT ON FLAT FEET PATIENTS’ WALKING SPEED. Journal of Prosthetics Orthotics and Science Technology 2023; 2: 6-10. </ref> | |||
* Foot orthoses with arch support help to redistribute plantar foot pressure and relieve foot pain. | |||
* Medial forefoot and rearfoot postings should be considered in addition to arch support for more aggressive flatfoot posture correction.<ref>Peng Y, Wang Y, Wong DW, Chen TL, Chen SF, Zhang G, Tan Q, Zhang M. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8960448/pdf/fbioe-10-853085.pdf Different Design Feature Combinations of Flatfoot Orthosis on Plantar Fascia Strain and Plantar Pressure: A Muscle-Driven Finite Element Analysis With Taguchi Method]. Front Bioeng Biotechnol. 2022 Mar 10;10:853085.</ref> | |||
The following video discusses how progression in age effect feet and person's mobility.{{#ev:youtube|v=j_819z3ILH0|300}}<ref>Dr Sinha Housecall Doctors. How Aging Affects Your Feet | |||
Available from: https://www.youtube.com/watch?v=j_819z3ILH0 [last accessed 17/09/2022]</ref> | |||
== Resources == | |||
*[https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6240965/pdf/10.1177_2151459318801756.pdf Frailty as an Outcome Predictor After Ankle Fractures: Where Are We Now?] | |||
*[https://bmcgeriatr.biomedcentral.com/articles/10.1186/s12877-020-1448-9 Does the shoe really fit? Characterising ill-fitting footwear among community-dwelling older adults attending geriatric services: an observational cross-sectional study]. | |||
== References == | == References == | ||
Latest revision as of 11:44, 20 November 2023
Original Editor - Ewa Jaraczewska based on the course by Helene Simpson
Top Contributors - Ewa Jaraczewska, Jess Bell and Kim Jackson
Introduction[edit | edit source]
One in four older adults have foot pain.[1] Foot pain can affect walking and contribute to falling and functional disability in older adults.[2] The aetiology of foot pain is often multifactorial. Foot pain may be caused by musculoskeletal pathologies, as well as vascular and Neurological Disorders,[3] but the three major foot problems in older adults are pain, neuropathy, and deformities.[4] The most common orthopaedic deformities in the elderly include hallux valgus, prominent metatarsal heads, and an abnormal medial arch structure.[2] Overall, foot deformities and other foot conditions are highly prevalent in adults aged over 65 years,[5] which is significant as these conditions are associated with frailty and decreased physical activity.[4]This article will discuss age related changes in the foot and suggested therapeutic interventions to improve balance, decrease risk for falls, and prevent or reduce skin and functional changes. It highlights the need for education and remediation regarding footwear advice in older adults.
Risk factors[edit | edit source]
The following are risk factors for foot problems in older adults:
- Gender (women are more frequently affected than men)[1][6]
- Obesity[4]
- Chronic conditions, including diabetes and osteoarthritis[4]
- Peripheral neuropathy[6]
- Neurological disorders (e.g. stroke, Parkinson's)[4]
- Lower extremity oedema (can be related to vascular or cardiac pathology)[6]
- Inappropriate footwear[4]
- Underlying geriatric syndromes and conditions[4]
Age-Related Changes in the Foot[edit | edit source]
Physiological changes[edit | edit source]
Skin[edit | edit source]
Weight-bearing activities place specific demands on the skin of the foot's plantar surface. The foot has certain features to accommodate these loads:[1] the epidermis is thicker in the foot compared to other parts of the body; the dermis is around 3mm thick and has adipose tissue that can resist sheer forces; and the fingerprint-like pattern of the epidermis helps to generate enough friction during walking.[1] However, all aspects of the skin change as a person ages. These changes affect not only the superficial skin but also the local vascular response, thermoregulation, sensory perception, and injury response,[7] and they include:
- Flattening of the dermo-epidermal junction[1]
- Decreased contact between the dermis and epidermis, which causes the skin to separate along this interface[8]
- Loss of elastin and collagen fibres in the dermis. The dermis becomes atrophic. There is a reduction of fibroblasts, and the collagen becomes disorganised.[8] The remaining collagen fibres become thicker and stiffer.[9]
- Limited ability by the dense collagen to recoil, which leads to increased compression and development of hyperkeratosis (corns and calluses)[10]
- Hyperkeratosis is defined as increased thickness of the outer layer of the skin[11]
- Alteration in the mechanical properties of the plantar skin, leading to increased hardness[1] and dryness
- A reduction in the density of sweat glands, which contributes to impaired thermoregulation[1][8]
- Loss of subcutaneous fat and decreased dermal vascularity, leading to poor thermoregulation[8]
- Reduced sensation to touch, pressure, and vibration due to decreased mechanoreceptors (Meissner and Pacini corpuscles)[8]
Overall, the thickening of the exterior layer of the skin and the presence of calluses may lead to the development of plantar lesions, causing severe pain and disability. The best management strategies are custom-made orthotics, which support the medial arch and unload the metatarsal heads.[6]
Soft Tissue[edit | edit source]
The role of the plantar soft tissue is to protect underlying blood vessels and nerves and to reduce the shear forces that occur while walking. Ageing has a direct impact on the foot's soft tissues, causing progressive stiffness. In particular, it affects the tissue at the big toe, first, third, and fifth metatarsal heads, and the heel.[12] The metatarsal pad becomes slower to recover after being compressed. Similarly, the heel pad dissipates more energy when compressed,[1] the plantar fascia demonstrates less recoil due to stiffness.[13] The consequences of the soft tissue ageing process are:[1]
- Range of motion reduction (especially in ankle dorsiflexion)
- Achilles tendon complaints
- Changes in gait pattern: more pull-off vs pushing-off, less propulsion
- Increased risk of falls
Range of Motion[edit | edit source]
The ageing process affects joint physiology, leading to joint stiffness. Changes include:[1]
- Reduction in the water content of the cartilage
- Reduction in the synovial fluid volume and proteoglycans
- Bonding of the collagen fibres
A decreased ankle dorsiflexion and subtalar joint inversion-eversion range in older adults contribute to their reduced ability to perform dynamic tasks, maintain static standing balance, and perform functional activities.[14]
Muscle Strength[edit | edit source]
Progressive changes in skeletal muscle mass (sarcopenia), metabolism and functional capacity are typical in the ageing population.[15] Older adults experience a reduction in the size and number of muscle fibres in their foot muscles. Large, slow-twitch motor units develop and type II fibres become denervated. These changes indicate the presence of age-related atrophy, which can be exacerbated by wearing poorly fitting footwear long-term.[1] The consequences of atrophy of the foot muscles in the elderly include:[1]
- Decreased ankle plantar flexor strength (causes difficulty rising onto the toes)
- Weakness of the toe plantar flexors, which negatively affects the grasping function of the toes during weight-bearing activities (impaired static and dynamic balance and functional ability, increased risk of falls)[16]
- Development of toe deformities (hallux valgus and lesser toe deformities)
- They alter weight distribution under the foot when walking [19]
- Lower ambulatory performance[20]
Biomechanical Changes[edit | edit source]
Age-related changes in soft tissue, range of motion, and muscle strength lead to the following biomechanical changes:[1]
- The lowering of the medial longitudinal arch
- Reduced midfoot and metatarsal mobility
- Flatter and more dynamically pronated feet
- Planus foot posture
- Less plantarflexed calcaneus at the toe-off phase of gait
- Less propulsive gait pattern
Physiotherapy Intervention[edit | edit source]
General Principles[edit | edit source]
- Do not focus on just the foot
- Assess the kinetic chain: look at posture, weight distribution, and centre of mass distribution
- Offer a programme which includes stretching and strengthening
- Use manual techniques to reduce tissue stiffness
- Stimulate the plantar sensors
- Assess footwear
- Be careful when choosing orthotics for medial arch support: do not make the foot stiffer
Therapeutic Interventions[edit | edit source]
Manual Techniques[edit | edit source]
Manual techniques mobilisation of the stiff foot and stimulating the plantar sensory receptors to increase proprioception and improve balance.[6]
Mobilisation techniques can be one or more of the following:
- Mobilisation with movement: application of gentle pain-free overpressure to an end-range movement[21]
- Anterior/posterior talocrural joint mobilisation in weight-bearing and non-weight-bearing positions, which aims to for improving DF range of motion [22]
- Subtalar joint mobilisation for eversion and inversion[22]
- Mid-tarsal mobilisation for pronation and supination of the midfoot[22]
Plantar-sensory treatments may include the following:[23]
- Plantar massage
- Whole-body vibration
- Textured surface-stimulation treatment
According to Hu et al.[23], patients with chronic ankle instability may have better postural control after applying plantar-sensory treatments. Plantar massage and long-term whole-body vibration were found to be the most effective.
A randomized clinical trial by McKeon and Wikstrom[24], found that sensory-targeted ankle rehabilitation strategies improved single-leg postural control. One treatment was sufficient for the change to occur. However, it did not offer a long-lasting effect.
Stretching[edit | edit source]
Calf muscle stretching is recommended to reduce pressure on the forefoot.
The following complications may be associated with an increased forefoot pressure:[25]
- excessive pressure on the plantar aspect of the forefoot
- an increased plantar pressure due to premature forefoot with ground contact
- limited arterial perfusion to the forefoot plantar tissue for a prolonged time could increase the risk of ulceration or delayed foot ulcer healing
Calf muscles stretching outcomes:[25]
- several weeks of calf muscle stretch training improves ankle joint flexibility and dorsiflexion range of motion
- reduction in the pathological forefoot pressures
- improvement in dynamic gait pattern
Strengthening of the Foot Intrinsic Muscles[edit | edit source]
Strengthening: toe strengthening exercises to improve the strength of the intrinsic muscles of the foot, increase the stability of the arch, and improve the toe-off phase of gait and balance during ambulation.
The roles of the intrinsic muscles of the foot include the following:[26]
- stabilise the foot during balance on one foot
- support the medial longitudinal arch
- maintain concavity during walking
- stabilise the tarsal and metatarsal bones
- control the amount and speed of pronation of the foot
Examples of toe strengthening exercises include using toes to scrunch up the towel while the rest of the foot remains in contact with the ground. [26]
Footwear and Orthotics[edit | edit source]
Footwear assessment:
Ill-fitting shoes are one of the major underlying causes of foot problems in the older population.[27]
- Tight footwear can lead to callus formations or corns with skin hyperkeratosis and ulceration. [28]
- Tight and narrow footwear is linked to the development of hallux valgus deformity, or bunion.
- Dorsal foot pain, as one of the symptoms of lesser toe deformities, such as hammertoes, tends to get worse with ill-fitting footwear.
O'Rourke et al.[29] found that older adults often wear incorrectly fitting shoes or shoes with unsafe features, like slippers. Wearing slip-on slippers means the toe must grab even more to hang onto the slipper. This can contribute to the drop of the medial arch and the development of hammer toes.[6]
Footwear modification:
- Soft to cushion the foot and supportive to prevent the foot from collapsing.
- Wider and higher-toe box shoes.
- Foot inserts improve arch support, facilitate balance and decrease the width of the foot during weight-bearing manoeuvres. [30]
- Metatarsal pads and splits can help to limit the need for extra-depth shoes.
- Higher collars offer better support for balance.
- Extra-depth shoes are recommended for hammertoes or mid-foot arthrosis.
- Low-heeled footwear reduces the risk of falls.
- Athletic shoes and sneakers are associated with the lowest fall risk.
- Slip-resistant soles are recommended inside and outside the household to reduce the risk of falls.
Orthotics:
Introduction to Orthotics: collaboration with an orthotist to make a custom-made orthosis that supports the medial arch without increasing foot stiffness. The proper orthotics should allow for increased shock absorption capacity in the foot.
- Customised foot orthosis with medial longitudinal and transverse arch supports on the plantar pressure redistributes plantar pressure and contact area and enhances the functional support of the mid-foot. [31]
- Rigid medial arch support orthoses provide better feedback to improve stability in flat foot patients. [32]
- Foot orthoses with arch support help to redistribute plantar foot pressure and relieve foot pain.
- Medial forefoot and rearfoot postings should be considered in addition to arch support for more aggressive flatfoot posture correction.[33]
The following video discusses how progression in age effect feet and person's mobility.
Resources[edit | edit source]
- Frailty as an Outcome Predictor After Ankle Fractures: Where Are We Now?
- Does the shoe really fit? Characterising ill-fitting footwear among community-dwelling older adults attending geriatric services: an observational cross-sectional study.
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 Menz HB. Biomechanics of the ageing foot and ankle: a mini-review. Gerontology. 2015;61(4):381-8.
- ↑ 2.0 2.1 Zhang B, Lu Q. A current review of foot disorder and plantar pressure alternation in the elderly. Physical Activity and Health. 2020 Sep 2;4(1).
- ↑ Oh-Park M, Kirschner J, Abdelshahed D, Kim DDJ. Painful Foot Disorders in the Geriatric Population: A Narrative Review. Am J Phys Med Rehabil. 2019 Sep;98(9):811-819.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 Muchna A, Najafi B, Wendel CS, Schwenk M, Armstrong DG, Mohler J. Foot Problems in Older Adults Associations with Incident Falls, Frailty Syndrome, and Sensor-Derived Gait, Balance, and Physical Activity Measures. J Am Podiatr Med Assoc. 2018 Mar;108(2):126-139. doi: 10.7547/15-186. Epub 2017 Aug 30.
- ↑ Helfand AE. Foot problems in older patients: a focused podogeriatric assessment study in ambulatory care. J Am Podiatr Med Assoc. 2004 May-Jun;94(3):293-304.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Simpson H. The Ageing Foot Course. Plus 2022
- ↑ Fenske NA, Lober CW. Structural and functional changes of normal ageing skin. J Am Acad Dermatol. 1986 Oct;15(4 Pt 1):571-85.
- ↑ 8.0 8.1 8.2 8.3 8.4 Levine JM. Clinical aspects of ageing skin: Considerations for the wound care practitioner. Advances in skin & wound care. 2020 Jan 1;33(1):12-9.
- ↑ Smith L. Histopathologic characteristics and ultrastructure of ageing skin. Cutis. 1989 May;43(5):414-24.
- ↑ Periyasamy R, Anand S, Ammini AC. The effect of ageing on the hardness of foot sole skin: a preliminary study. Foot (Edinb). 2012 Jun;22(2):95-9.
- ↑ Farci F, Mahabal GD. Hyperkeratosis. [Updated 2022 May 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK562206/
- ↑ Kwan RL, Zheng YP, Cheing GL. The effect of ageing on the biomechanical properties of plantar soft tissues. Clin Biomech (Bristol, Avon). 2010 Jul;25(6):601-5.
- ↑ Jha DK, Wongkaewpotong J, Chuckpaiwong B. Effect of Age and BMI on Sonographic Findings of Plantar Fascia. J Foot Ankle Surg. 2022 May 23:S1067-2516(22)00157-0
- ↑ Hernández-Guillén D, Tolsada-Velasco C, Roig-Casasús S, Costa-Moreno E, Borja-de-Fuentes I, Blasco JM. Association ankle function and balance in community-dwelling older adults. PloS one. 2021 Mar 4;16(3):e0247885.
- ↑ Shur NF, Creedon L, Skirrow S, Atherton PJ, MacDonald IA, Lund J, Greenhaff PL. Age-related changes in muscle architecture and metabolism in humans: The potential contribution of physical inactivity to age-related functional decline. Ageing Research Reviews. 2021 Jul 1;68:101344.
- ↑ Yong-Wook K, Oh-Yun K, Heon-Seock C, Jong-Hyuck W, Chung-Hwi Y, Tae-Ho K. Comparison of Toe Plantar Flexors Strength and Balancing Ability between Elderly Fallers and Non-fallers. Journal of Physical Therapy Science 2011; 23 (1): 127-132
- ↑ Endo M, Ashton-Miller JA, Alexander NB. Effects of age and gender on toe flexor muscle strength. J Gerontol A Biol Sci Med Sci. 2002 Jun;57(6):M392-7.
- ↑ Menz HB, Morris ME, Lord SR. Foot and ankle risk factors for falls in older people: a prospective study. J Gerontol A Biol Sci Med Sci. 2006 Aug;61(8):866-70.
- ↑ Mickle KJ, Munro BJ, Lord SR, Menz HB, Steele JR. Gait, balance and plantar pressures in older people with toe deformities. Gait Posture. 2011 Jul;34(3):347-51.
- ↑ Hida T, Harada A. [Fall risk and fracture. Diagnosing sarcopenia and sarcopenic leg to prevent fall and fracture: its difficulty and pit falls]. Clin Calcium. 2013 May;23(5):707-12. Japanese.
- ↑ Abassi M, Whiteley R. Serial Within-Session Improvements in Ankle Dorsiflexion During Clinical Interventions Including Mobilization-With-Movement and A Novel Manipulation Intervention – A Case Series. IJSPT. 2021;16(4):1158-1168.
- ↑ 22.0 22.1 22.2 Shashua A, Flechter S, Avidan L, Ofir D, Melayev A, Kalichman L. The effect of additional ankle and midfoot mobilizations on plantar fasciitis: a randomized controlled trial. J Orthop Sports Phys Ther. 2015 Apr;45(4):265-72.
- ↑ 23.0 23.1 Hu X, Liao J, Hu X, Zeng Z, Wang L. Effects of plantar-sensory treatments on postural control in chronic ankle instability: A systematic review and meta-analysis. PLoS One. 2023 Jun 27;18(6):e0287689.
- ↑ McKeon PO, Wikstrom EA. The effect of sensory-targeted ankle rehabilitation strategies on single-leg centre of pressure elements in those with chronic ankle instability: A randomized clinical trial. J Sci Med Sport. 2019 Mar;22(3):288-293.
- ↑ 25.0 25.1 Macklin K, Healy A, Chockalingam N. The effect of calf muscle stretching exercises on ankle joint dorsiflexion and dynamic foot pressures, force and related temporal parameters. Foot (Edinb). 2012 Mar;22(1):10-7.
- ↑ 26.0 26.1 Karimzadeh A, Kouhzad Mohammadi H, Mehravar M, Zahednejad S, Taheri N, Sadeghi M. The effects of intrinsic foot muscles strengthening exercises on foot kinetic parameters in pronated foot subjects during forward jump landing. J Family Med Prim Care. 2022 Sep;11(9):5205-5210.
- ↑ Hijmans JM, Geertzen JH, Dijkstra PU, Postema K. A systematic review of the effects of shoes and other ankle or foot appliances on balance in older people and people with peripheral nervous system disorders. Gait Posture. 2007 Feb;25(2):316-23.
- ↑ Menz HB, Morris ME. Footwear characteristics and foot problems in older people. Gerontology. 2005 Sep-Oct;51(5):346-51.
- ↑ O’Rourke B, Walsh ME, Brophy R, Vallely S, Murphy N, Conroy B, Cunningham C, Horgan NF. Does the shoe fit? Characterising ill-fitting footwear among community-dwelling older adults attending geriatric services: an observational cross-sectional study. BMC geriatrics. 2020 Dec;20(1):1-8.
- ↑ Bapirzadeh K, Jamali A, Forghany S, Nester c, Tavakoli S, Hemmati F. The effect of three different insoles on balance in people with functional ankle instability. J Foot Ankle Res2014; 7 (Suppl 1), A19.
- ↑ Chen H-Y, Peng H-T, Chang C-K, Wang F-T, Yen C-H, Wang T-Y, Chuang H-C, Chiu F-Y, Song C-Y. Immediate Effect of Customized Foot Orthosis on Plantar Pressure and Contact Area in Patients with Symptomatic Hallux Valgus. Applied Sciences. 2022; 12(15):7593.
- ↑ Setyawan D, Septiani AE, Sari KIU. COMPARISON FOR THE USED OF RIGID MEDIAL ARCH SUPPORT AND FLEXIBLE MEDIAL ARCH SUPPORT ON FLAT FEET PATIENTS’ WALKING SPEED. Journal of Prosthetics Orthotics and Science Technology 2023; 2: 6-10.
- ↑ Peng Y, Wang Y, Wong DW, Chen TL, Chen SF, Zhang G, Tan Q, Zhang M. Different Design Feature Combinations of Flatfoot Orthosis on Plantar Fascia Strain and Plantar Pressure: A Muscle-Driven Finite Element Analysis With Taguchi Method. Front Bioeng Biotechnol. 2022 Mar 10;10:853085.
- ↑ Dr Sinha Housecall Doctors. How Aging Affects Your Feet Available from: https://www.youtube.com/watch?v=j_819z3ILH0 [last accessed 17/09/2022]