Male Urinary Incontinence: Difference between revisions
mNo edit summary |
No edit summary |
||
| (15 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Stacy Schiurring|Stacy Schiurring]] based on the course by [https://members.physio-pedia.com/course_tutor/pierre-roscher/ Pierre Roscher]<br> | <div class="editorbox"> '''Original Editor '''- [[User:Stacy Schiurring|Stacy Schiurring]] based on the course by [https://members.physio-pedia.com/course_tutor/pierre-roscher/ Pierre Roscher]<br> | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div>This page aims to provide an introductory discussion of men's health physiotherapy with regards to male | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div>This page aims to provide an introductory discussion of men's health physiotherapy with regards to male urinary incontinence. Please note that further training is required through a reputable pelvic health education company before attempting the techniques discussed in this page. See the Resources section at the bottom of this page for links to pelvic and men's health special interest groups. | ||
== Introduction == | == Introduction == | ||
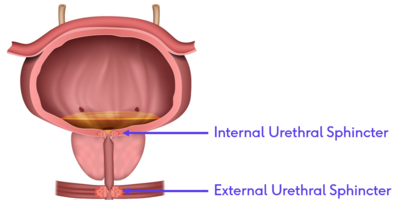
Normal urinary continence is maintained when the closure pressure of the urethra is greater than the pressure from the bladder above it. This requires a complex interaction between the autonomic nervous system that controls the more proximal smooth muscles of the internal urethral sphincter and the somatic nervous system that controls the striated muscles of the external urethral sphincter.<ref>Hodges PW, Stafford RE, Hall L, Neumann P, Morrison S, Frawley H, Doorbar-Baptist S, Nahon I, Crow J, Thompson J, Cameron AP. [https://www.sciencedirect.com/science/article/pii/S1078143919304946 Reconsideration of pelvic floor muscle training to prevent and treat incontinence after radical prostatectomy]. InUrologic Oncology: Seminars and Original Investigations 2019 Dec 25. Elsevier.</ref> | <blockquote>"Urinary and faecal incontinence are not usually at the forefront of physiotherapists’ minds on graduation; they are conditions that society still reacts to with silence or stigma. These conditions do not seem to have a significant place outside women’s health in physiotherapy practice and then mainly after pregnancy. As incontinence is often considered a women’s health issue, incontinence in men has been greatly neglected ... In recent years, partly due to the increase in lifespan and to improvements in survivorship with prostate cancer treatments, male UI and FI have become an area of importance to physiotherapists." <ref name=":1" /></blockquote>Normal urinary continence is maintained when the closure pressure of the urethra is greater than the pressure from the bladder above it. This requires a complex interaction between the [[Autonomic Nervous System|autonomic nervous system]] that controls the more proximal [[Muscle: Smooth|smooth muscles]] of the internal urethral sphincter and the somatic nervous system that controls the [[Muscle Cells (Myocyte)|striated muscles]] of the external urethral sphincter.<ref>Hodges PW, Stafford RE, Hall L, Neumann P, Morrison S, Frawley H, Doorbar-Baptist S, Nahon I, Crow J, Thompson J, Cameron AP. [https://www.sciencedirect.com/science/article/pii/S1078143919304946 Reconsideration of pelvic floor muscle training to prevent and treat incontinence after radical prostatectomy]. InUrologic Oncology: Seminars and Original Investigations 2019 Dec 25. Elsevier.</ref> | ||
{| class="wikitable" | {| class="wikitable" | ||
|+<ref name=":0">Roscher, P. Men's Health. Male Urinary Incontinence. | |+<ref name=":0">Roscher, P. Men's Health. Male Urinary Incontinence. Plus. 2022.</ref> | ||
! | ! | ||
!Innervation | !Innervation | ||
| Line 30: | Line 30: | ||
|} | |} | ||
[[File:Urethral Sphincters.png|thumb|400x400px|Urethral sphincters in situ]] | [[File:Urethral Sphincters.png|thumb|400x400px|Urethral sphincters in situ]] | ||
Issues with continence can occur for a variety of reasons. There can be problems with the closure mechanism of the urethra which would result in stress incontinence. There can also be problems with the bladder itself which could result in frequency, urgency and urge incontinence. Male urinary incontinence can have a significant psychosocial impact on an individual, affecting their [[Quality of Life|quality of life]], work absenteeism and depression. It can also have a significant emotional impact on the individual's spouse, partner or care provider.<ref name=":1">Nahon I. [https://www.researchgate.net/profile/Irmina-Nahon/publication/350198083_Physiotherapy_management_of_incontinence_in_men/links/60931ca3458515d315fc0b00/Physiotherapy-management-of-incontinence-in-men.pdf Physiotherapy management of incontinence in men.] Journal of physiotherapy. 2021 Apr 1;67(2):87-94.</ref> | |||
== The Micturition Cycle == | == The Micturition Cycle == | ||
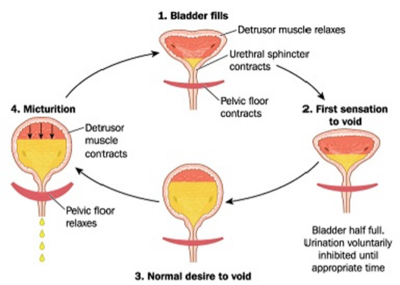
[[File:Normal micturition cycle.png|thumb|400x400px|Micturition Cycle]] | [[File:Normal micturition cycle.png|thumb|400x400px|Micturition Cycle]] | ||
Urinary continence is a pressure game.<ref name=":0" /> | Urinary continence is a pressure game.<ref name=":0" /> Maintaining urinary continence is a complex interaction between the bladder, [[Brain Anatomy|brain]], [[Pelvic Floor Anatomy|muscles of the pelvic floor]], and social contexts. The bladder spends 99% of the time in a storage phase, collecting [[urine]] as it arrives from the [[kidney]]<nowiki/>s via the ureters. The bladder undergoes receptive relaxation of the detrusor muscle to allow for the increasing volume without a rise in pressure. Low storage pressure is needed to allow urine drainage into the bladder from the upper urinary tract. While the bladder is in its storage phase, the urethra and the sphincteric mechanism are closed and the high outlet resistance pressure maintains continence. Urethral pressure is generated by the sphincter mechanism.<ref name=":1" /> | ||
When it is time to void, a series of coordinated parasympathetic peripheral and central pathways cause the urinary sphincters to relax while activating the detrusor muscle. Bladder fullness is a stimulus for voiding, and urge is a motivator.<ref name=":1" /> | When it is time to void, a series of coordinated [[Parasympathetic System|parasympathetic]], peripheral and central pathways cause the urinary sphincters to relax while activating the detrusor muscle. Bladder fullness is a stimulus for voiding, and urge is a motivator.<ref name=":1" /> The normal micturition cycle occurs 6-8 times per day.<ref name=":0" /> For more detailed information on the micturition cycle please read [[Micturition (Urinary) Reflex|this article.]] | ||
The following short video provides a thorough summary of the micturition cycle. | The following short video provides a thorough summary of the micturition cycle. | ||
{{#ev:youtube| Zl4VoTpxluQ |500}}<ref>YouTube. The Micturition Reflex | Bladder Nerve Supply | Renal Physiology. Available from: https://www.youtube.com/watch?v=Zl4VoTpxluQ [last accessed 23/03/2022]</ref> | {{#ev:youtube| Zl4VoTpxluQ |500}}<ref>YouTube. The Micturition Reflex | Bladder Nerve Supply | Renal Physiology. Available from: https://www.youtube.com/watch?v=Zl4VoTpxluQ [last accessed 23/03/2022]</ref> | ||
== Types of Male Urinary Incontinence == | == Types of Male Urinary Incontinence<ref>Tran LN, Puckett Y. Urinary incontinence. StatPearls [Internet]. 2022 Jan.</ref> == | ||
=== Stress Urinary Incontinence === | === Stress Urinary Incontinence === | ||
| Line 48: | Line 48: | ||
'''There are multiple internal and external sources of pressure:''' | '''There are multiple internal and external sources of pressure:''' | ||
* | * Forced exhalations such as coughing, sneezing, or laughing | ||
* | * Physical activity such as running or jumping | ||
* | * Post-catheter insertion | ||
* | * Cystoscopy (for examination of the bladder) | ||
* TURP operation | * Transurethral resection of the prostate (TURP operation) | ||
* | * Typical after a prostatectomy | ||
Stress urinary incontinence is typically treated by addressing urinary sphincter strength and or control, and pressure management.<ref name=":0" /> | Stress urinary incontinence is typically treated by addressing urinary sphincter strength and or control, and pressure management.<ref name=":0" /> | ||
=== Urge Urinary Incontinence === | === Urge Urinary Incontinence === | ||
Urge | Urge incontinence occurs when a person experiences urgency which is then followed by an involuntary loss of urine.<ref name=":2" /> The sense of urgency can be triggered by the detrusor muscle contracting due to irritation or input from a stimulus. This interrupts the normal micturition cycle resulting in more frequent, but smaller urinary voids.<ref name=":0" /> | ||
'''Examples of detrusor muscle stimuli:''' | '''Examples of detrusor muscle stimuli:''' | ||
* | * Increased fluid intake | ||
* Drinking alcohol | * Drinking alcohol | ||
* Drinking a "detoxing" beverage such as green tea | * Drinking a "detoxing" beverage such as green tea | ||
| Line 77: | Line 77: | ||
=== Other IncontinenceTerms === | === Other IncontinenceTerms === | ||
* '''Urgency / | * '''Urgency / overactive bladder''' is a strong, sudden need to urinate. When the detrusor muscle of the bladder contracts, it signals the need to urinate. Thus, when the bladder is overactive, “urgency” can develop. | ||
* '''Frequency''' is the need to urinate frequently, | * '''Frequency''' is the need to urinate frequently, characterised by the inability to delay urination. Frequency is often accompanied by urgency. | ||
* '''Nocturia''' is the need to wake up at night to | * '''Nocturia''' is the need to wake up at night to urinate. | ||
*'''Nocturnal | *'''Nocturnal enuresis''' is leaking of urine during sleep. | ||
*'''Post-micturition dribble''' is leaking that occurs immediately after urination. | *'''Post-micturition dribble''' is leaking that occurs immediately after urination. | ||
*'''Continuous urinary leakage''' is the inability to maintain any continence. | *'''Continuous urinary leakage''' is the inability to maintain any continence. | ||
| Line 90: | Line 90: | ||
== Physiotherapy Treatment for Male Incontinence == | == Physiotherapy Treatment for Male Incontinence == | ||
Effective treatment is often multi-faceted and requires multiple different treatment approaches. | Effective treatment is often multi-faceted and requires multiple different treatment approaches. Using the [[Biopsychosocial Model|biopsychosocial model]] is beneficial for this patient population.<ref name=":0" /><blockquote>"I think our role as physios are really to find out how we can help the patient the best. Once again, I keep going on about the biopsychosocial approach, not just in assessing, but in treating them as well." | ||
-Pierre Roscher, physiotherapist</blockquote>Getting a clear clinical picture of what is occurring during the daily routine of a patient with urinary incontinence will assist in creating an effective physiotherapy plan of care. This can be done by providing the patient with a '''bladder diary'''.<ref name=":0" /> | |||
==== '''Features of a Bladder Diary:''' ==== | ==== '''Features of a Bladder Diary:''' ==== | ||
| Line 99: | Line 98: | ||
* Tracks three-consecutive 24-hour periods | * Tracks three-consecutive 24-hour periods | ||
* Patient records all meals and drinks | * Patient records all meals and drinks | ||
* Patient records all eliminations (bowel and bladder) | * Patient records all eliminations (bowel and bladder) | ||
** | ** They should make notes if they are using male incontinence pads | ||
** preferable | ** If possible, it is preferable to get an accurate measurement of how much urine they are putting out (e.g. use a measuring cup) | ||
* Keeps track of daily activities: activity levels | * Keeps track of daily activities: activity levels | ||
Example of how bladder diary can be useful clinically: | Example of how a bladder diary can be useful clinically:<ref name=":0" /> | ||
* A patient with stress incontinence may record low urine outputs and a high number of used incontinence pads because they are leaking urine throughout the day | |||
* A patient with urge incontinence will record a high number of urinary voids with small output volumes | |||
==== Other Physiotherapy Interventions: ==== | ==== Other Physiotherapy Interventions:<ref>Griffith J, Wiegand L. [https://cdn.amegroups.cn/journals/vats/files/journals/27/articles/7069/public/7069-PB4-5496-R2.pdf Literature review on the efficacy of treatments for urinary incontinence in irradiated vs. non-radiated men treated for prostate cancer.] 2022.</ref> ==== | ||
* Pelvic floor work to improve sphincter control | *[[Pelvic Floor Exercises|Pelvic floor]] work to improve sphincter control - this approach is strongly supported by research<ref name=":0" /><ref>Hodges PW, Stafford RE, Hall L, Neumann P, Morrison S, Frawley H, Doorbar-Baptist S, Nahon I, Crow J, Thompson J, Cameron AP. [https://www.sciencedirect.com/science/article/abs/pii/S1078143919304946 Reconsideration of pelvic floor muscle training to prevent and treat incontinence after radical prostatectomy.] InUrologic Oncology: Seminars and Original Investigations 2020 May 1 (Vol. 38, No. 5, pp. 354-371). Elsevier.</ref> | ||
* Use of transperineal ultrasound<ref>Stafford RE, van den Hoorn W, Coughlin G, Hodges PW. [https://espace.library.uq.edu.au/data/UQ_678060/Stafford_PPI_displacements_2017.pdf?dsi_version=dd9b546beed585929f43a0e69ac6e34c&Expires=1648088801&Key-Pair-Id=APKAJKNBJ4MJBJNC6NLQ&Signature=gAdlCkJL5GYjtat9IU56R3aQDtuKN350lBzrhi9DoxOh5ofOqGU~-7kTXj~O~mVRb6IVecNeNrl47DESjfYCb~kMJ3RR36V87HR0aTPQsluEudParDHvNXBt1nxlA0S4QwuhrL~NNykaPc73Lg8CN4e2opaMc9gfZ4YmyuCw5S~p-9lGzFJK-~sAGRcAUgBToPnBggw0fjETdqDR6ttoMt8-7B7mVdHW1sxWxpKTHPILbKHcRIbLnFK5rKqYZmUMScFqghGcnzU2tRDedptGa1dA6RJGBkLGJmemfHBeupXWJVIjAeYIVRhNqCf3SZHUg-zl~zKijx7iCE5gn2C1-A__ Postprostatectomy incontinence is related to pelvic floor displacements observed with trans‐perineal ultrasound imaging.] Neurourology and urodynamics. 2018 Feb;37(2):658-65.</ref> for visual cues of pelvic floor contractions | * Use of transperineal ultrasound<ref>Stafford RE, van den Hoorn W, Coughlin G, Hodges PW. [https://espace.library.uq.edu.au/data/UQ_678060/Stafford_PPI_displacements_2017.pdf?dsi_version=dd9b546beed585929f43a0e69ac6e34c&Expires=1648088801&Key-Pair-Id=APKAJKNBJ4MJBJNC6NLQ&Signature=gAdlCkJL5GYjtat9IU56R3aQDtuKN350lBzrhi9DoxOh5ofOqGU~-7kTXj~O~mVRb6IVecNeNrl47DESjfYCb~kMJ3RR36V87HR0aTPQsluEudParDHvNXBt1nxlA0S4QwuhrL~NNykaPc73Lg8CN4e2opaMc9gfZ4YmyuCw5S~p-9lGzFJK-~sAGRcAUgBToPnBggw0fjETdqDR6ttoMt8-7B7mVdHW1sxWxpKTHPILbKHcRIbLnFK5rKqYZmUMScFqghGcnzU2tRDedptGa1dA6RJGBkLGJmemfHBeupXWJVIjAeYIVRhNqCf3SZHUg-zl~zKijx7iCE5gn2C1-A__ Postprostatectomy incontinence is related to pelvic floor displacements observed with trans‐perineal ultrasound imaging.] Neurourology and urodynamics. 2018 Feb;37(2):658-65.</ref> for visual cues of pelvic floor contractions to help improve urethral control | ||
* Behavioural management: discussing what to wear such as dark pants to hid leaks, limit fluid intake when away from home, awareness of any foods or drinks that may irritate the bladder<ref name=":0" /> | * Behavioural management: discussing what to wear such as dark pants to hid leaks, limit fluid intake when away from home, awareness of any foods or drinks that may irritate the bladder<ref name=":0" /> | ||
* Use of male incontinence pads<ref name=":0" /> | * Use of male incontinence pads<ref name=":0" /> | ||
| Line 115: | Line 117: | ||
* Use of questionnaires to gather information and track progress<ref name=":0" /> | * Use of questionnaires to gather information and track progress<ref name=":0" /> | ||
The following short video | The following short video highlights how pelvic floor dysfunction can result is a wide variety of symptoms. It stresses the importance of proper physiotherapy interviewing to get a full clinical picture of people with men's health needs. | ||
{{#ev:youtube| S2BnSdxY7AY |500}}<ref>YouTube. Core Pelvic Floor Therapy | Pelvic Floor Dysfunction in Men. Available from: https://www.youtube.com/watch?v=S2BnSdxY7AY [last accessed 23/03/2022]</ref> | {{#ev:youtube| S2BnSdxY7AY |500}}<ref>YouTube. Core Pelvic Floor Therapy | Pelvic Floor Dysfunction in Men. Available from: https://www.youtube.com/watch?v=S2BnSdxY7AY [last accessed 23/03/2022]</ref> | ||
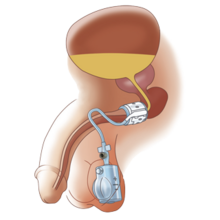
'''More invasive treatment options include:''' | '''More invasive treatment options include:'''[[File:Artificial Urinary Sphincter.png|thumb|220x220px|Artificial Urinary Sphincter]] | ||
* Sling surgery which alters the biomechanics of the bladder neck<ref>Meisterhofer K, Herzog S, Strini KA, Sebastianelli L, Bauer R, Dalpiaz O. [https://www.sciencedirect.com/science/article/abs/pii/S2405456919300082 Male slings for postprostatectomy incontinence: a systematic review and meta-analysis.] European Urology Focus. 2020 May 15;6(3):575-92.</ref> | |||
* | * Artificial Urinary Sphincter | ||
* | ** Involves placing a small cuff around the urethra, which can be inflated/deflated by a small pump placed in the scrotum | ||
* | * Pharmacological options which help control bladder stimulation | ||
<ref name=":0" /> | <ref name=":0" /> | ||
The following | The following video discusses surgical procedures for male urinary incontinence. | ||
<div class="row"> | <div class="row"> | ||
<div class="col-md-6"> {{#ev:youtube| ymMRuEPozsI |400}}<ref>YouTube. Urinary incontinence in men, artificial urinary sphincter pt1. Available from: https://www.youtube.com/watch?v=ymMRuEPozsI&t=2s[last accessed 23/03/2022]</ref> </div></div> | <div class="col-md-6"> {{#ev:youtube| ymMRuEPozsI |400}}<ref>YouTube. Urinary incontinence in men, artificial urinary sphincter pt1. Available from: https://www.youtube.com/watch?v=ymMRuEPozsI&t=2s[last accessed 23/03/2022]</ref> </div></div> | ||
| Line 147: | Line 148: | ||
* American Physical Therapy Association: [https://aptapelvichealth.org/ Academy of Pelvic Health] | * American Physical Therapy Association: [https://aptapelvichealth.org/ Academy of Pelvic Health] | ||
* American Physical Therapy Association: [https://apta.site-ym.com/store/ViewProduct.aspx?id=14929266 On-Demand: Male Pelvic Pain Course] | * American Physical Therapy Association: [https://apta.site-ym.com/store/ViewProduct.aspx?id=14929266 On-Demand: Male Pelvic Pain Course] | ||
* Australian Physiotherapy Association: [https://choose.physio/your-lifestage/adults/mens-health Men's Health] | * Australian Physiotherapy Association: [https://choose.physio/your-lifestage/adults/mens-health Men's Health] | ||
* Australian Physiotherapy Association: [https://australian.physio/inmotion/physiotherapy-and-male-pelvic-health Male Pelvic Health] | * Australian Physiotherapy Association: [https://australian.physio/inmotion/physiotherapy-and-male-pelvic-health Male Pelvic Health] | ||
| Line 155: | Line 155: | ||
<references /> | <references /> | ||
[[Category:Course Pages]] | [[Category:Course Pages]] | ||
[[Category:Mens Health]] | [[Category:Mens Health]] | ||
[[Category: | [[Category:Plus Content]] | ||
Latest revision as of 04:24, 29 October 2023
Top Contributors - Stacy Schiurring, Kim Jackson, Lucinda hampton and Jess Bell
This page aims to provide an introductory discussion of men's health physiotherapy with regards to male urinary incontinence. Please note that further training is required through a reputable pelvic health education company before attempting the techniques discussed in this page. See the Resources section at the bottom of this page for links to pelvic and men's health special interest groups.
Introduction[edit | edit source]
"Urinary and faecal incontinence are not usually at the forefront of physiotherapists’ minds on graduation; they are conditions that society still reacts to with silence or stigma. These conditions do not seem to have a significant place outside women’s health in physiotherapy practice and then mainly after pregnancy. As incontinence is often considered a women’s health issue, incontinence in men has been greatly neglected ... In recent years, partly due to the increase in lifespan and to improvements in survivorship with prostate cancer treatments, male UI and FI have become an area of importance to physiotherapists." [1]
Normal urinary continence is maintained when the closure pressure of the urethra is greater than the pressure from the bladder above it. This requires a complex interaction between the autonomic nervous system that controls the more proximal smooth muscles of the internal urethral sphincter and the somatic nervous system that controls the striated muscles of the external urethral sphincter.[2]
| Innervation | Type of Muscle | Function and Features | |
|---|---|---|---|
| Internal Urethral
Sphincter |
Autonomic control | Smooth muscle |
|
| External Urethral
Sphincter |
Somatic voluntary control | Striated skeletal muscle |
|
Issues with continence can occur for a variety of reasons. There can be problems with the closure mechanism of the urethra which would result in stress incontinence. There can also be problems with the bladder itself which could result in frequency, urgency and urge incontinence. Male urinary incontinence can have a significant psychosocial impact on an individual, affecting their quality of life, work absenteeism and depression. It can also have a significant emotional impact on the individual's spouse, partner or care provider.[1]
The Micturition Cycle[edit | edit source]
Urinary continence is a pressure game.[3] Maintaining urinary continence is a complex interaction between the bladder, brain, muscles of the pelvic floor, and social contexts. The bladder spends 99% of the time in a storage phase, collecting urine as it arrives from the kidneys via the ureters. The bladder undergoes receptive relaxation of the detrusor muscle to allow for the increasing volume without a rise in pressure. Low storage pressure is needed to allow urine drainage into the bladder from the upper urinary tract. While the bladder is in its storage phase, the urethra and the sphincteric mechanism are closed and the high outlet resistance pressure maintains continence. Urethral pressure is generated by the sphincter mechanism.[1]
When it is time to void, a series of coordinated parasympathetic, peripheral and central pathways cause the urinary sphincters to relax while activating the detrusor muscle. Bladder fullness is a stimulus for voiding, and urge is a motivator.[1] The normal micturition cycle occurs 6-8 times per day.[3] For more detailed information on the micturition cycle please read this article.
The following short video provides a thorough summary of the micturition cycle.
Types of Male Urinary Incontinence[5][edit | edit source]
Stress Urinary Incontinence[edit | edit source]
Stress incontinence occurs when the closure force of the sphincter mechanism is unable to control the amount of pressure being exerted from the bladder, resulting in leaking urine.[6]
There are multiple internal and external sources of pressure:
- Forced exhalations such as coughing, sneezing, or laughing
- Physical activity such as running or jumping
- Post-catheter insertion
- Cystoscopy (for examination of the bladder)
- Transurethral resection of the prostate (TURP operation)
- Typical after a prostatectomy
Stress urinary incontinence is typically treated by addressing urinary sphincter strength and or control, and pressure management.[3]
Urge Urinary Incontinence[edit | edit source]
Urge incontinence occurs when a person experiences urgency which is then followed by an involuntary loss of urine.[6] The sense of urgency can be triggered by the detrusor muscle contracting due to irritation or input from a stimulus. This interrupts the normal micturition cycle resulting in more frequent, but smaller urinary voids.[3]
Examples of detrusor muscle stimuli:
- Increased fluid intake
- Drinking alcohol
- Drinking a "detoxing" beverage such as green tea
- Bladder infection
- Social aspects such a timing in a routine or hearing water running
Mixed Urinary Incontinence[edit | edit source]
Mixed urinary incontinence is a combination of stress and urge incontinence features.[6]
Other IncontinenceTerms[edit | edit source]
- Urgency / overactive bladder is a strong, sudden need to urinate. When the detrusor muscle of the bladder contracts, it signals the need to urinate. Thus, when the bladder is overactive, “urgency” can develop.
- Frequency is the need to urinate frequently, characterised by the inability to delay urination. Frequency is often accompanied by urgency.
- Nocturia is the need to wake up at night to urinate.
- Nocturnal enuresis is leaking of urine during sleep.
- Post-micturition dribble is leaking that occurs immediately after urination.
- Continuous urinary leakage is the inability to maintain any continence.
The following 7-minute video reviews the micturition cycle and discusses different types of incontinence.
Physiotherapy Treatment for Male Incontinence[edit | edit source]
Effective treatment is often multi-faceted and requires multiple different treatment approaches. Using the biopsychosocial model is beneficial for this patient population.[3]
"I think our role as physios are really to find out how we can help the patient the best. Once again, I keep going on about the biopsychosocial approach, not just in assessing, but in treating them as well." -Pierre Roscher, physiotherapist
Getting a clear clinical picture of what is occurring during the daily routine of a patient with urinary incontinence will assist in creating an effective physiotherapy plan of care. This can be done by providing the patient with a bladder diary.[3]
Features of a Bladder Diary:[edit | edit source]
- Self-reported
- Tracks three-consecutive 24-hour periods
- Patient records all meals and drinks
- Patient records all eliminations (bowel and bladder)
- They should make notes if they are using male incontinence pads
- If possible, it is preferable to get an accurate measurement of how much urine they are putting out (e.g. use a measuring cup)
- Keeps track of daily activities: activity levels
Example of how a bladder diary can be useful clinically:[3]
- A patient with stress incontinence may record low urine outputs and a high number of used incontinence pads because they are leaking urine throughout the day
- A patient with urge incontinence will record a high number of urinary voids with small output volumes
Other Physiotherapy Interventions:[8][edit | edit source]
- Pelvic floor work to improve sphincter control - this approach is strongly supported by research[3][9]
- Use of transperineal ultrasound[10] for visual cues of pelvic floor contractions to help improve urethral control
- Behavioural management: discussing what to wear such as dark pants to hid leaks, limit fluid intake when away from home, awareness of any foods or drinks that may irritate the bladder[3]
- Use of male incontinence pads[3]
- Use of penile clamps[3]
- Use of questionnaires to gather information and track progress[3]
The following short video highlights how pelvic floor dysfunction can result is a wide variety of symptoms. It stresses the importance of proper physiotherapy interviewing to get a full clinical picture of people with men's health needs.
More invasive treatment options include:
- Sling surgery which alters the biomechanics of the bladder neck[12]
- Artificial Urinary Sphincter
- Involves placing a small cuff around the urethra, which can be inflated/deflated by a small pump placed in the scrotum
- Pharmacological options which help control bladder stimulation
The following video discusses surgical procedures for male urinary incontinence.
Resources[edit | edit source]
- Bladder Diary Printout Example
- Johns Hopkins Medicine list of dietary bladder irritants
- Kaiser Permanente Medicine list of dietary bladder irritants
To learn more about bladder irritants and how they can affect incontinence, please review this article:
- Burgio KL, Newman DK, Rosenberg MT, Sampselle C. Impact of behaviour and lifestyle on bladder health. International journal of clinical practice. 2013 Jun;67(6):495-504.
Professional Associations and formal continuing education courses:
- American Physical Therapy Association: Academy of Pelvic Health
- American Physical Therapy Association: On-Demand: Male Pelvic Pain Course
- Australian Physiotherapy Association: Men's Health
- Australian Physiotherapy Association: Male Pelvic Health
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Nahon I. Physiotherapy management of incontinence in men. Journal of physiotherapy. 2021 Apr 1;67(2):87-94.
- ↑ Hodges PW, Stafford RE, Hall L, Neumann P, Morrison S, Frawley H, Doorbar-Baptist S, Nahon I, Crow J, Thompson J, Cameron AP. Reconsideration of pelvic floor muscle training to prevent and treat incontinence after radical prostatectomy. InUrologic Oncology: Seminars and Original Investigations 2019 Dec 25. Elsevier.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 Roscher, P. Men's Health. Male Urinary Incontinence. Plus. 2022.
- ↑ YouTube. The Micturition Reflex | Bladder Nerve Supply | Renal Physiology. Available from: https://www.youtube.com/watch?v=Zl4VoTpxluQ [last accessed 23/03/2022]
- ↑ Tran LN, Puckett Y. Urinary incontinence. StatPearls [Internet]. 2022 Jan.
- ↑ 6.0 6.1 6.2 6.3 Abrams P, Andersson KE, Apostolidis A, Birder L, Bliss D, Brubaker L, Cardozo L, Castro-Diaz D, O'connell PR, Cottenden A, Cotterill N. 6th International Consultation on Incontinence. Recommendations of the International Scientific Committee: evaluation and treatment of urinary incontinence, pelvic organ prolapse and faecal incontinence.Neurourology and urodynamics. 2018;37(7):2271-2.
- ↑ YouTube. Urinary incontinence - causes, symptoms, diagnosis, treatment, pathology. Available from: https://www.youtube.com/watch?v=vsLBApSlPMo [last accessed 23/03/2022]
- ↑ Griffith J, Wiegand L. Literature review on the efficacy of treatments for urinary incontinence in irradiated vs. non-radiated men treated for prostate cancer. 2022.
- ↑ Hodges PW, Stafford RE, Hall L, Neumann P, Morrison S, Frawley H, Doorbar-Baptist S, Nahon I, Crow J, Thompson J, Cameron AP. Reconsideration of pelvic floor muscle training to prevent and treat incontinence after radical prostatectomy. InUrologic Oncology: Seminars and Original Investigations 2020 May 1 (Vol. 38, No. 5, pp. 354-371). Elsevier.
- ↑ Stafford RE, van den Hoorn W, Coughlin G, Hodges PW. Postprostatectomy incontinence is related to pelvic floor displacements observed with trans‐perineal ultrasound imaging. Neurourology and urodynamics. 2018 Feb;37(2):658-65.
- ↑ YouTube. Core Pelvic Floor Therapy | Pelvic Floor Dysfunction in Men. Available from: https://www.youtube.com/watch?v=S2BnSdxY7AY [last accessed 23/03/2022]
- ↑ Meisterhofer K, Herzog S, Strini KA, Sebastianelli L, Bauer R, Dalpiaz O. Male slings for postprostatectomy incontinence: a systematic review and meta-analysis. European Urology Focus. 2020 May 15;6(3):575-92.
- ↑ YouTube. Urinary incontinence in men, artificial urinary sphincter pt1. Available from: https://www.youtube.com/watch?v=ymMRuEPozsI&t=2s[last accessed 23/03/2022]