Vertebral Fractures in Children and Adolescents: Difference between revisions
Daisy Meffan (talk | contribs) mNo edit summary |
(Header,ref and text edits) |
||
| (27 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- [[User: | '''Original Editor '''- [[User:Daisy Meffan|Daisy Meffan]] as part of the [[Nottingham University Spinal Rehabilitation Project]]<br> | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Definition/Description == | == Definition/Description == | ||
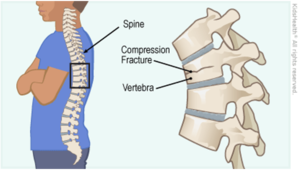
A spinal fracture happens when a vertebral body collapses | A spinal fracture happens when a vertebral body collapses. When this occurs in the paediatric population and because the bones are still developing, this may have severe consequences. A vertebral fracture is less obvious compared to a long bone fracture but is often very painful. <ref>Todd S., Di Marco M. Vertebral Fractures in Children. NHS Greater Glasgow and Clyde. Available from:https://www.smn.scot.nhs.uk/wp-content/uploads/2019/01/Vertebral-fractures-in-children.pdf [Accessed 11/3/2023]. </ref> | ||
==Clinically Relevant Anatomy == | ==Clinically Relevant Anatomy == | ||
=== Cervical spine === | |||
*Epiphyseal variants | *Epiphyseal variants | ||
*Epiphyseal plates are smooth and regular and have sclerotic lines | *Epiphyseal plates are smooth and regular and have sclerotic lines | ||
| Line 18: | Line 18: | ||
*Hyper-mobility | *Hyper-mobility | ||
[[File:Cpsine.png|thumb|Ossification centres of C1 with open synchondroses (arrows) <ref name=":0">Lustrin E., Karakas S., Ortiz A., Cinnamon J., Castillo M., Vaheesan K., Brown J., Diamond A., Black K., Singh S. [https://doi.org/10.1148/rg.233025121 Pediatric cervical spine: normal anatomy, variants, and trauma]. Radiographics. 2003 May;23(3):539-60.</ref> |alt=|200x200px]] | |||
C1 | === C1 === | ||
*Anterior arch is ossified in only 20% of cases at birth | |||
*Anterior arch is ossified in only 20% of cases at birth | *Becomes visible as an ossification centre by 1 year of age | ||
*Becomes visible as an ossification centre by 1 year of age | |||
*Neural arches appear in 7th foetal week | *Neural arches appear in 7th foetal week | ||
*Anterior arch fuses with the neural arches by 7 | *Anterior arch fuses with the neural arches by 7 | ||
*Non-fusion before this can be mistaken for a fracture | *Non-fusion before this can be mistaken for a fracture | ||
*The neural arches fuse posteriorly by 3 years of age. | *The neural arches fuse posteriorly by 3 years of age. | ||
*Occasionally, the anterior ossification centre of C1 does not develop and the neural arches attempt to fuse anteriorly- This fusion abnormality can be differentiated from a fracture in that it demonstrates sclerotic margins | *Occasionally, the anterior ossification centre of C1 does not develop and the neural arches attempt to fuse anteriorly- This fusion abnormality can be differentiated from a fracture in that it demonstrates sclerotic margins | ||
=== C2 === | |||
C2 | [[File:C2 2.png|thumb|Ossification centres of C2 with open synchondroses (arrows) <ref name=":0" />]] | ||
[[File:C2 2.png|thumb|Ossification centres of C2 with open synchondroses (arrows) | The axis, has the most complex and unique development of all vertebrae. There are four ossification centres at birth: | ||
There are four ossification centres at birth: | |||
*One for each neural arch | *One for each neural arch | ||
*One for the body | *One for the body | ||
*One for the odontoid process | *One for the odontoid process | ||
The odontoid process forms in utero from two separate ossification centres that fuse in the midline by the 7th foetal month. | The odontoid process forms in utero from two separate ossification centres that fuse in the midline by the 7th foetal month. A secondary ossification centre appears at the apex of the odontoid process (os terminale) between 3 and 6 years of age and fuses by age 12 years. The body of C2 fuses with the odontoid process by 3–6 years of age. This fusion line (subdental synchondrosis), or the remnant of the cartilaginous synchondrosis, can be seen until age 11 years and may be confused with a fracture. The neural arches fuse posteriorly by 2–3 years of age and with the body of the odontoid process between 3 and 6 years of age <ref name=":1">Gray H., Bannister L., Berry M., Williams P. Gray's anatomy. 37th ed. Philadelphia, Pa: Lea and Febiger; 1989.</ref> <ref name=":2">Harris J., Harris J., Mirvis S. The radiology of acute cervical spine trauma. Lippincott Williams & Wilkins; 1996.</ref> <ref name=":3">Herman M., Pizzutillo P. [https://doi.org/10.1016/S0030-5898(05)70098-5 Cervical spine disorders in children.] Orthop Clin North Am. 1999 Jul 1;30(3):457-66.</ref> <ref name=":4">Ogden J. [https://link.springer.com/article/10.1007/BF00361083 Radiology of postnatal skeletal development.] Skeletal Radiology. 1984 Sep;12(3):169-77.</ref> <ref name=":5">Swischuk L. [https://books.google.com.ng/books?hl=en&lr=&id=rkEZbnCVnBkC&oi=fnd&pg=PR11&dq=Swischuk+LE.+Emergency+imaging+of+the+acutely+ill+or+injured+child.+Lippincott+Williams+%26+Wilkins%3B+2000&ots=mT-0HgnTcj&sig=YxCAMAiCzv_EEx2yTmzvxwJt0Xk&redir_esc=y#v=onepage&q=Swischuk%20LE.%20Emergency%20imaging%20of%20the%20acutely%20ill%20or%20injured%20child.%20Lippincott%20Williams%20%26%20Wilkins%3B%202000&f=false Emergency imaging of the acutely ill or injured child]. Lippincott Williams & Wilkins; 2000.</ref>. C3 through C7 can be discussed as a unit because they exhibit the same developmental pattern. | ||
A secondary ossification centre appears at the apex of the odontoid process (os terminale) between 3 and 6 years of age and fuses by age 12 years. | |||
The body of C2 fuses with the odontoid process by 3–6 years of age. | |||
This fusion line (subdental synchondrosis), or the remnant of the cartilaginous synchondrosis, can be seen until age 11 years and may be confused with a fracture. | |||
The neural arches fuse posteriorly by 2–3 years of age and with the body of the odontoid process between 3 and 6 years of age | |||
C3 through C7 can be discussed as a unit because they exhibit the same developmental pattern. | |||
Three ossification sites are present: | Three ossification sites are present in: | ||
*The body - which arises from a single ossification site | *The body - which arises from a single ossification site | ||
*The two neural arches | *The two neural arches | ||
The neural arches fuse posteriorly by age 2–3 years, and the body fuses with the neural arches between 3 and 6 years of age. Additionally, secondary ossification centres may be seen at the tips of the transverse processes and spinous processes that may persist until early in the 3rd decade of life and simulate fractures. Secondary ossification centres can also appear at the superior and inferior aspects of the cervical vertebral bodies and remain unfused until early adulthood. <ref name=":1" /> <ref name=":2" /> <ref name=":3" /><ref name=":4" /><ref>Bailey D. [https://doi.org/10.1148/59.5.712 The normal cervical spine in infants and children.] Radiology. 1952 Nov;59(5):712-9.</ref> | |||
=== Ligaments === | |||
Ligaments | |||
*The anterior and posterior atlanto-occipital membranes extend from the upper aspect of C1 to the anterior and posterior aspects of the foramen magnum. | *The anterior and posterior atlanto-occipital membranes extend from the upper aspect of C1 to the anterior and posterior aspects of the foramen magnum. | ||
*The anterior atlantoaxial ligament extends from the anterior midportion of the dens to the inferior aspect of the anterior arch of C1. | *The anterior atlantoaxial ligament extends from the anterior midportion of the dens to the inferior aspect of the anterior arch of C1. | ||
| Line 58: | Line 50: | ||
*The transverse ligament extends from the tubercle on the inner aspect of one side of the atlas to the tubercle on the other side. | *The transverse ligament extends from the tubercle on the inner aspect of one side of the atlas to the tubercle on the other side. | ||
*The apical ligament lies between the superior longitudinal fasciculus of the cruciform ligament and the anterior atlanto-occipital membrane. | *The apical ligament lies between the superior longitudinal fasciculus of the cruciform ligament and the anterior atlanto-occipital membrane. | ||
*The alar ligaments connect the lateral aspect of the dens and the medial inferior aspect of the occipital condyles- the main function of the alar ligaments is to limit rotation to the contralateral side ( | *The alar ligaments connect the lateral aspect of the dens and the medial inferior aspect of the occipital condyles- the main function of the alar ligaments is to limit rotation to the contralateral side. <ref name=":1" /><ref name=":2" /><ref name=":5" /><ref>Cattell H., Filtzer D. [https://journals.lww.com/jbjsjournal/Abstract/1965/47070/Pseudosubluxation_and_Other_Normal_Variations_in.1.aspx Pseudosubluxation and other normal variations in the cervical spine in children: A study of one hundred and sixty children]. JBJS. 1965 Oct 1;47(7):1295-309.</ref> | ||
==Paediatric Versus Adult Cervical Spine == | ==Paediatric Versus Adult Cervical Spine == | ||
Cervical spine injuries in children usually occur in the upper cervical spine from the occiput to C3. | Cervical spine injuries in children usually occur in the upper [[Cervical Spine Case Studies|cervical spine]] from the occiput to C3. This fact may be explained by the unique biomechanics and anatomy of the paediatric cervical spine. | ||
This fact may be explained by the unique biomechanics and anatomy of the paediatric cervical spine. | *The fulcrum of motion in the cervical spine in children is at the C2-C3 level; in the adult cervical spine, the fulcrum is at the C5-C6 level. <ref>Kokoska E., Keller M., Rallo M., Weber T.. [https://doi.org/10.1053/jpsu.2001.20022 Characteristics of pediatric cervical spine injuries.] J Ped Surg. 2001 Jan 1;36(1):100-5.</ref> <ref name=":6">Roche C., Carty H. [https://link.springer.com/article/10.1007/s002470100532 Spinal trauma in children.] Pediatric Radiology. 2001 Oct;31(10):677-700.</ref> | ||
*The fulcrum of motion in the cervical spine in children is at the C2-C3 level; in the adult cervical spine, the fulcrum is at the C5-C6 level ( | |||
*The immature spine is hypermobile because of ligamentous laxity, shallow and angled facet joints, underdeveloped spinous processes, and physiologic anterior wedging of vertebral bodies, all of which contribute to high torque and shear forces acting on the C1-C2 region. | *The immature spine is hypermobile because of ligamentous laxity, shallow and angled facet joints, underdeveloped spinous processes, and physiologic anterior wedging of vertebral bodies, all of which contribute to high torque and shear forces acting on the C1-C2 region. | ||
*Incomplete ossification of the odontoid process, a relatively large head, and weak neck muscles are other factors that predispose to instability of the paediatric cervical spine | *Incomplete ossification of the odontoid process, a relatively large head, and weak neck muscles are other factors that predispose to instability of the paediatric cervical spine. <ref name=":2" /> <ref name=":3" /> <ref name=":5" /> <ref name=":6" /> <ref>McGrory B., Klassen R., Chao E., Staeheli J., Weaver A. [https://europepmc.org/article/med/8335674 Acute fractures and dislocations of the cervical spine in children and adolescents.] J Bone Joint Surg. American volume. 1993 Jul 1;75(7):988-95.</ref> <ref>Davis B. Media Reviews. [https://doi.org/10.1080/312703002831 Rosen's Emergency Medicine: Concepts and Clinical Practice]. Prehosp Emerg Care. 2004 Jan 1;8(3):334-5.</ref><ref>Bilston L., Brown J. [https://journals.lww.com/spinejournal/Abstract/2007/10010/Pediatric_Spinal_Injury_Type_and_Severity_Are_Age.11.aspx Pediatric spinal injury type and severity are age and mechanism dependent.] Spine. 2007 Oct 1;32(21):2339-47.</ref> | ||
==Kyphosis and Lordosis== | ==Kyphosis and Lordosis== | ||
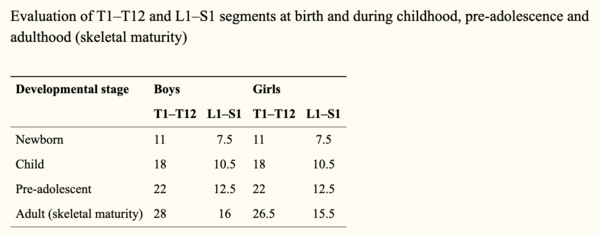
Kyphosis and lordosis are shown to increase at a linear rate from a child to adolescent age. | [[Kyphosis]] and lordosis are shown to increase at a linear rate from a child to adolescent age. | ||
*Kyphotic curves increase from 25° at 7 years of age to 38° at 19 years of age (kyphotic angle = 25° + 0.58 × age) | *Kyphotic curves increase from 25° at 7 years of age to 38° at 19 years of age (kyphotic angle = 25° + 0.58 × age) | ||
*Lordotic curves increase from 22° at 5 years of age to 32° at 20 years of age (lordotic angle = 24° + 0.51 × age). | *Lordotic curves increase from 22° at 5 years of age to 32° at 20 years of age (lordotic angle = 24° + 0.51 × age). | ||
* | *No differences were reported between males and females. <ref>Giglio C., Volpon J. [https://doi.org/10.1007/s11832-007-0033-5 Development and evaluation of thoracic kyphosis and lumbar lordosis during growth.] J Child Orthop. 2007 Sep 1;1(3):187-93.</ref> | ||
[[File:Screenshot 2021-05-23 at 22.23.10.png|center|thumb|600x600px|Heights of thoracolumbar vertebra at birth, during childhood, pre-adolescence and adulthood. <ref>Dimeglio A., Canavese F. [https://link.springer.com/article/10.1007/s00586-011-1983-3 The growing spine: how spinal deformities influence normal spine and thoracic cage growth]. Eur Spine J. 2012 Jan;21(1):64-70.</ref>]] | |||
[[File:Screenshot 2021-05-23 at 22.23.10.png|center|thumb|600x600px|Dimeglio A, Canavese F. The growing spine: how spinal deformities influence normal spine and thoracic cage growth. | |||
== Epidemiology/Aetiology == | == Epidemiology/Aetiology == | ||
Spinal fractures make up only 1-3% of all paediatric fractures | Spinal fractures make up only 1-3% of all paediatric fractures. <ref name=":7">Bouyer B., Vassal M., Zairi F., Dhenin A., Grelat M., Dubory A., Giorgi H., Walter A., Lonjon G., Dauzac C., Lonjon N. [https://doi.org/10.1016/j.otsr.2014.11.012 Surgery in vertebral fracture: epidemiology and functional and radiological results in a prospective series of 518 patients at 1 year's follow-up]. Orthop Traumatol Surg Res. 2015 Feb 1;101(1):11-5.</ref> This is less incidence than in the adult population due to the child’s spine being more mobile and elastic and having a smaller mass compared to adults. <ref name=":9">Parisini P., Di Silvestre M., Greggi T. [https://journals.lww.com/spinejournal/Abstract/2002/09150/Treatment_of_Spinal_Fractures_in_Children_and.6.aspx Treatment of spinal fractures in children and adolescents: long-term results in 44 patients]. Spine. 2002 Sep 15;27(18):1989-94.</ref> Bone structure and strength are considered vital predictors of fracture occurrence in children <ref name=":10">Tan V., Macdonald H., Kim S., Nettlefold L., Gabel L., Ashe M., McKay H. [https://doi.org/10.1002/jbmr.2254 Influence of physical activity on bone strength in children and adolescents: a systematic review and narrative synthesis]. J Bone Mineral Res. 2014 Oct;29(10):2161-81.</ref> and a bone mass reduction of 6.4% doubles the risk of fracture.<ref name=":11">Boreham C., McKay H. [http://dx.doi.org/10.1136/bjsports-2011-090188 Physical activity in childhood and bone health.] Br J Sports Med. 2011 Sep 1;45(11):877-9.</ref> The incidence of these fractures is higher in children under the age of 5 and over the age of 10 years. <ref name=":8">Saul D., Dresing K. [https://doi.org/10.4081/pr.2018.7232 Epidemiology of vertebral fractures in pediatric and adolescent patients]. Pediatr Rep. 2018 Mar;10(1):17-23.</ref> Spinal fractures in adolescents can have devastating consequences such as spinal deformity, [[scoliosis]] and [[syringomyelia]]. <ref name=":8" /> | ||
The cervical spine is the most common location for factures in infants, because of the anatomy of the infant spine such as a heavy head and less muscular | The cervical spine is the most common location for factures in infants, because of the peculiarity of the anatomy of the infant spine such as having a heavy head and less muscular neck which puts more strain on the spine. <ref name=":8" /> As previously mentioned, the paediatric spinal anatomy is different from the adult's which predisposes children to flexion and extension injuries. Some of these differences include the facet joints being oriented differently leading to greater mobility but worse stability in the spine. <ref name=":7" /> | ||
In a child's spine, there is a high resistance against compression forces largely due to resilient intevertebral discs. <ref name=":8" /> A high stress distribution in the anterior compartment of children's spines predisposes this area in particular to fractures. <ref name=":8" /> Paediatric spinal fractures are usually caused by high impact and speed injuries. These predominantly include: falls, sporting impact injuries and road traffic accidents with the most common fractures being compression fractures where the vertebral bodies collapse. | |||
In a review by Tan et al | In a review by Tan et al. <ref name=":10" /> bone strength was defined as the ability to resist fractures while taking into consideration extrinsic properties of bones such as mineral mass and distribution of bone mass. Studies provide strong evidence of the relationship between [[Physical Activity|physical activity]] and bone mass as concentric and eccentric muscle contractions elicited from physical activity place high loads on the skeleton. <ref name=":10" /> Also, fracture incidence was shown to be at its peak in early puberty at 10-12 years in girls and 13-15 years for boys. <ref name=":11" /> | ||
==Mechanism of Injury== | ==Mechanism of Injury== | ||
Neck fractures are common in children due to their disproportionately large head in comparison to weak neck muscles, which cause a bending movement on impact that is larger than the neck muscles can protect from. The upper cervical facet joints are also horizontally orientated and shallow with laxity in the ligaments | Neck fractures are common in children due to their disproportionately large head in comparison to weak neck muscles, which cause a bending movement on impact that is larger than the neck muscles can protect from. The upper cervical facet joints are also horizontally orientated and shallow with laxity in the ligaments. <ref name=":12">Leonard M., Sproule J., Mc Cormack D. [https://doi.org/10.1016/j.injury.2006.09.019 Paediatric spinal trauma and associated injuries.] Injury. 2007 Feb 1;38(2):188-93.</ref> Usually ligament laxity prevents injury in other body parts by transferring energy however this property is not shared by the spinal cord. <ref name=":12" /> | ||
Due to the positioning of the paediatric spine and it's increased elasticity from the increased cartilage and intervertebral disc thickness, there has to be a considerable amount of force obtained to cause an unstable fracture | Due to the positioning of the paediatric spine and it's increased elasticity from the increased cartilage and intervertebral disc thickness, there has to be a considerable amount of force obtained to cause an unstable [[fracture]]. <ref name=":9" /> | ||
*Motor Vehicle accidents – both passengers and pedestrians (Most Common) | *Motor Vehicle accidents – both passengers and pedestrians (Most Common) <ref name=":8" /><ref name=":12" /> | ||
*Cycling | *Cycling | ||
*Falls from a height (also common) | *Falls from a height (also common) <ref name=":8" /><ref name=":12" /> | ||
*Sporting Injuries | *Sporting Injuries <ref name=":8" /><ref name=":12" /> | ||
*Assault | *Assault | ||
=== Fractures Types === | |||
'''Contiguous compression fractures''' - common in paediatric spinal injury due to the increased C- spine mobility, commonly linked to flexion movements, however increased mobility does mean there is reduced neurological compromise. <ref name=":12" /> | |||
''' | '''Burst fractures''' – make up only 10% of all thoracolumbar injuries in paediatrics due to the increase in spinal flexibility, meaning the pressure is not concentrated in one area - the common cause of burst fractures. This also reduces neurological damage along the increased size of the paediatric spinal canal compared to the spinal cord and cauda equina. <ref name=":12" /> | ||
'''Chance fracture''' – common in children when wearing lap belts in motor traffic accidents. The seat belt acts as a fulcrum causing hyperflexion, commonly seen alongside intra-abdominal and head injuries. <ref name=":12" /> | |||
'''Apophyseal ring fractures''' - only found in the paediatric population. Normally seen in adolescents and occurs due to the ring apophysis and the vertebral body not fusing completely and may separate in the process. <ref>Ravi Kumar T., Rao R., Gadi D., Grover A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4484115/ Lumbar apophyseal ring fracture-a case report.] JCDR. 2015 May;9(5):RD01.</ref>[[File:Picture to show compression fracture .png|thumb|Visualisation of vertebral compression fracture|alt=|center]] | |||
==Characteristics/ Clinical Presentation== | ==Characteristics/ Clinical Presentation== | ||
A 10 year report at a children's university hospital found symptoms were as follows: <ref name=":8" /> <ref name=":12" /> | |||
*neck | === '''C-spine Fracture''' === | ||
*[[Neck Pain: Clinical Practice Guidelines|neck pain]] | |||
*neurological deficit | *neurological deficit | ||
| Line 141: | Line 116: | ||
*Common Additional Injuries - facial/head injuries, skull and facial fractures, facial lacerations, intercranial injury | *Common Additional Injuries - facial/head injuries, skull and facial fractures, facial lacerations, intercranial injury | ||
=== '''T-spine Fracture''' === | |||
'''T-spine Fracture''' | |||
*back pain | *back pain | ||
| Line 156: | Line 129: | ||
| | ||
'''L-spine Fracture''' | === '''L-spine Fracture''' === | ||
*Back pain | *Back pain | ||
| Line 167: | Line 139: | ||
| | ||
Due to children having a larger spinal canal than their spinal cord they can tolerate more compression than adults can before neural | Due to children having a larger spinal canal than their spinal cord they can tolerate more compression than adults can before neural damage occurs | ||
'''N/B''': Ensure to look for fractures at all levels of the spine (C-spine, T-spine and L-spine) when assessing for potential spinal fracture in children. <ref name=":8" /> | |||
== | ===Fracture trends=== | ||
In children below 5 the most common area to injure was T8 followed by lumbar | * In children below 5 the most common area to injure was T8 followed by lumbar | ||
* Between the ages of 5-10 the most common fracture area was the thoracolumbar region | |||
Between the ages of 5-10 the most common fracture area was the thoracolumbar region | * In teenagers the most common area begins to shift to the lumbar spine | ||
* From 15 years and older the lumbar area is most affected | |||
In teenagers the most common area begins to shift to the lumbar spine | <ref name=":8" /> | ||
From 15 years and older the lumbar area is most affected | |||
==Differential Diagnosis== | ==Differential Diagnosis== | ||
| Line 187: | Line 157: | ||
* [[Ankylosing Spondylitis (Axial Spondyloarthritis)|Juvenile Ankylosing Spondylitis]] | * [[Ankylosing Spondylitis (Axial Spondyloarthritis)|Juvenile Ankylosing Spondylitis]] | ||
* [[Disc Herniation]] | * [[Disc Herniation]] | ||
* Spinal cord injury without radiographic abnormality | * [[Spinal Cord Injury|Spinal cord injury]] without radiographic abnormality | ||
==Diagnostic Procedures== | ==Diagnostic Procedures== | ||
* Sensation of ‘breath arrest’ - immediately after the trauma the children would feel extremely short of breath, this is a predictive factor for vertebral fracture, particularly thoracolumbar fractures. | * '''Sensation of ‘breath arrest’''' - immediately after the trauma the children would feel extremely short of breath, this is a predictive factor for vertebral fracture, particularly thoracolumbar fractures. | ||
* X-ray – due to cartilaginous nature of the vertebra, fractures | * '''X-ray''' – due to the cartilaginous nature of the vertebra, fractures are not always clear from routine x-rays and children can go undiagnosed. | ||
* MRI – used to determine diagnosis of potential fractures shown on x-ray | * '''MRI''' – used to determine diagnosis of potential fractures shown on x-ray. They give clear images of the vertebra allowing for more accurate diagnosis. This allows for direct visualisation and confirmation of the fracture, where it is in the spine and what type of fracture has occurred. | ||
* CT scan – | * '''CT scan''' – these have better prognostic ability than x-ray as they show bony details in higher definition than an x-ray. It is therefore more likely to get a clear diagnosis from a CT scan than an x-ray. However, like with x-rays fractures can go unnoticed on CT scans, therefore if there is any doubt about the potential of a fracture it should be followed up with an MRI scan to clarify a potential diagnosis. | ||
* Flexion/Extension C-spine x-rays – often used after CT scans if no findings are present to determine if there is any undiagnosed cervical instability | * '''Flexion/Extension C-spine x-rays –''' often used after CT scans if no findings are present to determine if there is any undiagnosed cervical instability <ref>Leroux J., Vivier P., Slimane M., Foulongne E., Abu-Amara S., Lechevallier J., Griffet J. [https://doi.org/10.1016/j.otsr.2012.10.009 Early diagnosis of thoracolumbar spine fractures in children. A prospective study]. Orthopaedics & Traumatology: Surgery & Research. 2013 Feb 1;99(1):60-5.</ref><ref>Cui S., France J. Fractures of the Spine in Children. Available from: https://ota.org/sites/files/2018-06/P13-Fractures%20of%20the%20Spine%20in%20Children.pdf [Accessed 18//05/2021]</ref><ref>Murphy A. Cervical spine (flexion and extension views). Radiopaedia. Available from: https://radiopaedia.org/articles/58732 [Accessed 18/05/2021]</ref> | ||
=== Other Diagnostic Tools === | |||
==== '''Nexus criteria''' ==== | |||
National Emergency R-ray Utilisation Group criteria assesses low-risk patients for cervical spine injury. It is primarily used to determine if an x-ray is required or if further imaging is needed after an x-ray to determine possible diagnosis. | |||
Nexus criteria | Nexus criteria: <ref>Stiell I., Clement C., Wells G., Morrison L. [https://www.proquest.com/openview/29d86e493a0dfb6541fd112b5e0cf370/1?pq-origsite=gscholar&cbl=45787 Prospective validation of the NEXUS low-risk criteria for cervical spine radiography.] CJEM 2002 Mar 1;4(2):129.</ref> | ||
*Absence of midline cervical tenderness | *Absence of midline cervical tenderness | ||
| Line 218: | Line 187: | ||
*Absence of a painful, distracting injury | *Absence of a painful, distracting injury | ||
Canadian C-spine Rule | ==== '''Canadian C-spine Rule''' ==== | ||
These are a set of guidelines to help a clinician decide if cervical imaging (i.e. x-ray, CT or MRI) are appropriate for trauma patients. For children however, consideration needs to be taken around developmental stage, so applying these rules can be difficult. | |||
C-spine rules: | C-spine rules: <ref>Fox S.. Paediatric Cervical Spine Injury. Paediatric EM Morsels: Paediatric Emergency Medicine Education. Available from: https://pedemmorsels.com/pediatric-cervical-spine-injury/ [Accessed 18/05/2021]</ref> | ||
# Any high-risk factors which mandate radiography | # Any high-risk factors which mandate radiography | ||
| Line 236: | Line 205: | ||
# Able to actively rotate neck | # Able to actively rotate neck | ||
#* 45 degrees left and right | #* 45 degrees left and right | ||
== Management == | == Management == | ||
'''Conservative Management''' | === '''Conservative Management''' === | ||
==== Casting ==== | |||
There are two types: Minerva and Plaster and they usually stay on for a period of around 2 months. | |||
==== Halo Vests ==== | |||
To be worn for an average of 8 weeks. | |||
==== Bed Rest ==== | |||
Until acute symptoms subside, followed by a moulded body cast. | |||
Conservative management, particularly of wedge fractures without neurological lesions can be successful, leaving only moderate residual deformities. However, it is important there is an accurate diagnosis to confirm the stability of the fracture to ensure accurate treatment is provided.Whilst nonoperative treatment is viable for burst fractures in children with no neurological deficits and minimal initial kyphosis, operative treatments are recommended for unstable burst fractures to correct the deformity. <ref name=":9" /> | |||
'''Angelliaume et al, 2017:''' <ref>Angelliaume A., Simon A., Boissière L., Bouty A., Sales de Gauzy J., Vital J., Gille O., Tournier C., Aunoble S., Pontailler J., Lefèvre Y. [https://doi.org/10.1097/BPB.0000000000000329 Conservative treatment of pediatric thoracic and lumbar spinal fractures: outcomes in the sagittal plane.] J Pediatr Orthop B. 2016 Jan 1;26(1):73-9.</ref> | |||
* In a case of a stable spinal fracture without [[Neurological Disorders|neurological]] deficiency, conservative treatment must be the first treatment of choice in children | |||
*The significant difference between the initial and the final local kyphosis at the thoracic level was not found for the lumbar level. | |||
*It is hypothesised that the brace is more efficient at the thoracic level than at the lumbar level and enables more remodelling, decreasing compressive forces by an antikyphotic effect- furthermore, it is easier to correct a thoracic kyphosis than a lumbar one using an antikyphotic brace | |||
Functional outcomes | ==== Functional outcomes ==== | ||
*Functional results indicated a high rate of back pain. | *Functional results indicated a high rate of back pain. | ||
*However, patients’ functional results were satisfactory because they reported no limitations in their daily life activities and did not use painkillers. | *However, patients’ functional results were satisfactory because they reported no limitations in their daily life activities and did not use painkillers. | ||
| Line 268: | Line 232: | ||
*However, rates of back pain in adolescents without back injury are also high, with a prevalence of 7–70% . | *However, rates of back pain in adolescents without back injury are also high, with a prevalence of 7–70% . | ||
=== Surgical Management === | |||
[[File:Post-operative radiographs after short instrumentation and anterior grafting to treat a burst fracture of T12..png|thumb|Spinal internal fixation <ref name=":13" /> ]]Overall surgical interventions depend on the type and severity of the fracture. The Denis classification can be used to differentiate between a stable and a unstable vertebral fracture which can help decide on management options. Generally according to the evidence, lots of stable fractures can be treated conservatively however unstable fractures will require surgical management. <ref name=":9" /> <ref name=":13">Sayama C., Chen T., Trost G., Jea A. [https://doi.org/10.3171/2014.5.FOCUS1490 A review of pediatric lumbar spine trauma.] Neurosurgical Focus. 2014 Jul 1;37(1):E6.</ref> Furthermore, if the patient has a neurological deficit or a spinal cord injury, surgery is necessary to stabilise the fracture and gain neurological function. <ref>Ferrero E., Compagnon R., Pesenti S., Lefèvre Y., Polirsztok E., Ilharreborde B., de Gauzy J. [https://doi.org/10.1016/j.otsr.2019.08.021 Surgical management of burst fractures in children and adolescents: A Multicentre Retrospective Study.] Orthopaedics & Traumatology: Surgery & Research. 2020 Feb 1;106(1):173-8.</ref> Surgical outcomes within the population have been positive. Vander Have et al. <ref>Vander Have K., Caird M., Gross S., Farley F., Graziano G., Stauff M., Segal L. [https://journals.lww.com/pedorthopaedics/Abstract/2009/10000/Burst_Fractures_of_the_Thoracic_and_Lumbar_Spine.11.aspx Burst fractures of the thoracic and lumbar spine in children and adolescents.] J Pediatr Orthop. 2009 Oct 1;29(7):713-9.</ref> found that surgical intervention was positive in ensuring the correction of the kyphosis of the spine compared to conservative management that which led to worsening of kyphosis. | |||
Types of surgery can vary depending on the type of fracture and the age. Adolescents can be treated using adult type instrumentation due to a more developed spine <ref name=":13" /> whereas, younger children have smaller pedicles so a normal screw placement in this area can be challenging. <ref name=":13" /> Evidence suggests a shorted fusion is the prefered approach in peadiactric fractures in order to preserve growth and mobility. <ref>Lalonde F., Letts M., Yang J., Thomas K. [https://europepmc.org/article/med/11234937 An analysis of burst fractures of the spine in adolescents.] Am J Orthop. 2001 Feb 1;30(2):115-20.</ref> In the lumbar spine, lumbar fusion can be used which involves fusing the vertebral bodies together so no movement can occur between them enabling the fracture to be repaired, this can be managed via a posterior approach. <ref name=":14">Boddu S. Spinal Compression Fractures. Weill Cornell Brain and Spine Centre. Available from: https://weillcornellbrainandspine.org/condition/spinal-compression-fractures/surgery-spinal-compression-fractures [Accessed 12/03/2023]</ref> If the fracture is more severe, reconstruction surgery such as vertebroplasty or kyphoplasty can take place. <ref name=":14" /> Although conservative management has been proven to correct initial conditions and deformities, these deformities can return overtime leading to a short term fix as opposed to a long term fix. | |||
Types of surgery can vary depending on the type of fracture and the age. | |||
== Prevention == | == Prevention == | ||
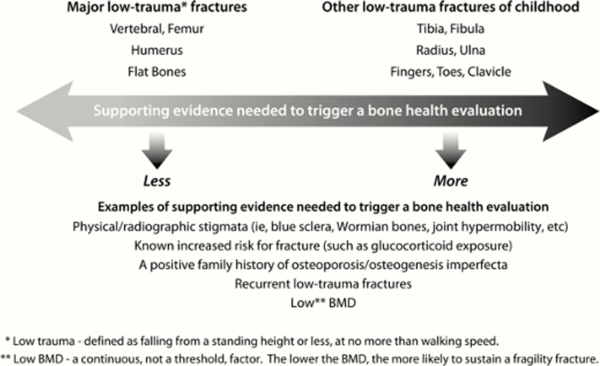
Over recent years there has been an increased recognition of the need to identify children with bone fragility | Over recent years, there has been an increased recognition of the need to identify children with bone fragility, <ref name=":15">Ward L., Weber D., Munns C., Högler W., Zemel B. [https://doi.org/10.1210/clinem/dgz294 A contemporary view of the definition and diagnosis of osteoporosis in children and adolescents.] J Clin Endocrinol Metab. 2020 May;105(5):e2088-97.</ref> this is due to [[osteoporosis]] being thought to root from childhood therefore preventative efforts should be initiated in early life to ensure life-long bone health. <ref name=":16">Golden N., Abrams S. [https://pediatrics.aappublications.org/content/134/4/e1229.short Optimizing bone health in children and adolescents.] Pediatrics. 2014 Oct 1;134(4):e1229-43.</ref> | ||
* | *'''Calcium''': intake during infancy, childhood and adolescence contribute to bone mass gain. Dietary supplementations may be offered to those who cannot take in enough calcium. <ref name=":16" /> | ||
* | *'''Vitamin D:''' testing for vitamin D deficiency is recommended for those who have recurrent traumatic fractures even on low-impact. <ref name=":16" /> | ||
* | *'''Mechanical loading and weight bearing exercise''': puts force on the skeleton that increases bone formation. <ref name=":16" /> | ||
Dual Energy X-ray absorptiometry (DXA) is considered the gold standard for the assessment for bone mass as it is preferred due to low radiation. <ref name=":16" /> It is reported that an association occurs between low bone mass measured using DXA and increased fracture risk in children.<ref name=":16" /> | |||
There is a need to assess each child on an individual basis to identify if they need a bone health evaluation. In the diagram below,<ref name=":16" /> it can be seen what health factors should be considered in the decision of whether to conduct a bone health evaluation. <ref name=":15" /> | |||
An additional consideration is road traffic safety. Leonard et al. <ref name=":12" /> found in their study of paediatric spinal trauma that children who were restrained by a lap belt in the rear of a vehicle whereby a head on collision occurred led to hyperflexion of their spine and resulting in intra-abdominal and head injuries. <ref name=":12" /> To prevent these injuries from occuring, it is recommended that cross-body seat belts and booster seats be used to strap chiodren in vehicles. | |||
[[File:Example of supporting evidence needed to trigger a bone health evaluation.png|thumb|The extent of supporting evidence needed to trigger a bone health evaluation in relation to fracture characteristics <ref name=":15" />|alt=|center|600x600px]] | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Nottingham University Spinal Rehabilitation Project]] | |||
[[Category:Paediatrics]] | |||
[[Category:Paediatrics - Conditions]] | |||
[[Category:Paediatrics - Assessment and Examination]] | |||
[[Category:Paediatrics - Interventions]] | |||
Latest revision as of 11:30, 12 March 2023
Original Editor - Daisy Meffan as part of the Nottingham University Spinal Rehabilitation Project
Top Contributors - Daisy Meffan, Alexia Derbyshire, Cindy John-Chu and Angeliki Chorti
Definition/Description[edit | edit source]
A spinal fracture happens when a vertebral body collapses. When this occurs in the paediatric population and because the bones are still developing, this may have severe consequences. A vertebral fracture is less obvious compared to a long bone fracture but is often very painful. [1]
Clinically Relevant Anatomy[edit | edit source]
Cervical spine[edit | edit source]
- Epiphyseal variants
- Epiphyseal plates are smooth and regular and have sclerotic lines
- Unique vertebral architecture
- Incomplete ossification of synchondroses and apophyses
- Hyper-mobility
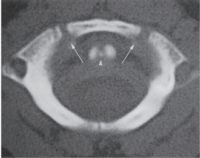
C1[edit | edit source]
- Anterior arch is ossified in only 20% of cases at birth
- Becomes visible as an ossification centre by 1 year of age
- Neural arches appear in 7th foetal week
- Anterior arch fuses with the neural arches by 7
- Non-fusion before this can be mistaken for a fracture
- The neural arches fuse posteriorly by 3 years of age.
- Occasionally, the anterior ossification centre of C1 does not develop and the neural arches attempt to fuse anteriorly- This fusion abnormality can be differentiated from a fracture in that it demonstrates sclerotic margins
C2[edit | edit source]
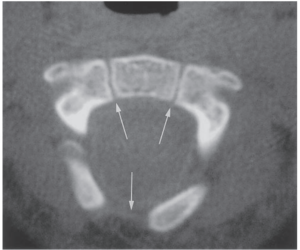
The axis, has the most complex and unique development of all vertebrae. There are four ossification centres at birth:
- One for each neural arch
- One for the body
- One for the odontoid process
The odontoid process forms in utero from two separate ossification centres that fuse in the midline by the 7th foetal month. A secondary ossification centre appears at the apex of the odontoid process (os terminale) between 3 and 6 years of age and fuses by age 12 years. The body of C2 fuses with the odontoid process by 3–6 years of age. This fusion line (subdental synchondrosis), or the remnant of the cartilaginous synchondrosis, can be seen until age 11 years and may be confused with a fracture. The neural arches fuse posteriorly by 2–3 years of age and with the body of the odontoid process between 3 and 6 years of age [3] [4] [5] [6] [7]. C3 through C7 can be discussed as a unit because they exhibit the same developmental pattern.
Three ossification sites are present in:
- The body - which arises from a single ossification site
- The two neural arches
The neural arches fuse posteriorly by age 2–3 years, and the body fuses with the neural arches between 3 and 6 years of age. Additionally, secondary ossification centres may be seen at the tips of the transverse processes and spinous processes that may persist until early in the 3rd decade of life and simulate fractures. Secondary ossification centres can also appear at the superior and inferior aspects of the cervical vertebral bodies and remain unfused until early adulthood. [3] [4] [5][6][8]
Ligaments[edit | edit source]
- The anterior and posterior atlanto-occipital membranes extend from the upper aspect of C1 to the anterior and posterior aspects of the foramen magnum.
- The anterior atlantoaxial ligament extends from the anterior midportion of the dens to the inferior aspect of the anterior arch of C1.
- The tectorial membrane is the superior extension of the posterior longitudinal ligament and attaches to the anterolateral aspect of the foramen magnum.
- The transverse ligament extends from the tubercle on the inner aspect of one side of the atlas to the tubercle on the other side.
- The apical ligament lies between the superior longitudinal fasciculus of the cruciform ligament and the anterior atlanto-occipital membrane.
- The alar ligaments connect the lateral aspect of the dens and the medial inferior aspect of the occipital condyles- the main function of the alar ligaments is to limit rotation to the contralateral side. [3][4][7][9]
Paediatric Versus Adult Cervical Spine[edit | edit source]
Cervical spine injuries in children usually occur in the upper cervical spine from the occiput to C3. This fact may be explained by the unique biomechanics and anatomy of the paediatric cervical spine.
- The fulcrum of motion in the cervical spine in children is at the C2-C3 level; in the adult cervical spine, the fulcrum is at the C5-C6 level. [10] [11]
- The immature spine is hypermobile because of ligamentous laxity, shallow and angled facet joints, underdeveloped spinous processes, and physiologic anterior wedging of vertebral bodies, all of which contribute to high torque and shear forces acting on the C1-C2 region.
- Incomplete ossification of the odontoid process, a relatively large head, and weak neck muscles are other factors that predispose to instability of the paediatric cervical spine. [4] [5] [7] [11] [12] [13][14]
Kyphosis and Lordosis[edit | edit source]
Kyphosis and lordosis are shown to increase at a linear rate from a child to adolescent age.
- Kyphotic curves increase from 25° at 7 years of age to 38° at 19 years of age (kyphotic angle = 25° + 0.58 × age)
- Lordotic curves increase from 22° at 5 years of age to 32° at 20 years of age (lordotic angle = 24° + 0.51 × age).
- No differences were reported between males and females. [15]
Epidemiology/Aetiology[edit | edit source]
Spinal fractures make up only 1-3% of all paediatric fractures. [17] This is less incidence than in the adult population due to the child’s spine being more mobile and elastic and having a smaller mass compared to adults. [18] Bone structure and strength are considered vital predictors of fracture occurrence in children [19] and a bone mass reduction of 6.4% doubles the risk of fracture.[20] The incidence of these fractures is higher in children under the age of 5 and over the age of 10 years. [21] Spinal fractures in adolescents can have devastating consequences such as spinal deformity, scoliosis and syringomyelia. [21]
The cervical spine is the most common location for factures in infants, because of the peculiarity of the anatomy of the infant spine such as having a heavy head and less muscular neck which puts more strain on the spine. [21] As previously mentioned, the paediatric spinal anatomy is different from the adult's which predisposes children to flexion and extension injuries. Some of these differences include the facet joints being oriented differently leading to greater mobility but worse stability in the spine. [17]
In a child's spine, there is a high resistance against compression forces largely due to resilient intevertebral discs. [21] A high stress distribution in the anterior compartment of children's spines predisposes this area in particular to fractures. [21] Paediatric spinal fractures are usually caused by high impact and speed injuries. These predominantly include: falls, sporting impact injuries and road traffic accidents with the most common fractures being compression fractures where the vertebral bodies collapse.
In a review by Tan et al. [19] bone strength was defined as the ability to resist fractures while taking into consideration extrinsic properties of bones such as mineral mass and distribution of bone mass. Studies provide strong evidence of the relationship between physical activity and bone mass as concentric and eccentric muscle contractions elicited from physical activity place high loads on the skeleton. [19] Also, fracture incidence was shown to be at its peak in early puberty at 10-12 years in girls and 13-15 years for boys. [20]
Mechanism of Injury[edit | edit source]
Neck fractures are common in children due to their disproportionately large head in comparison to weak neck muscles, which cause a bending movement on impact that is larger than the neck muscles can protect from. The upper cervical facet joints are also horizontally orientated and shallow with laxity in the ligaments. [22] Usually ligament laxity prevents injury in other body parts by transferring energy however this property is not shared by the spinal cord. [22]
Due to the positioning of the paediatric spine and it's increased elasticity from the increased cartilage and intervertebral disc thickness, there has to be a considerable amount of force obtained to cause an unstable fracture. [18]
- Cycling
- Assault
Fractures Types[edit | edit source]
Contiguous compression fractures - common in paediatric spinal injury due to the increased C- spine mobility, commonly linked to flexion movements, however increased mobility does mean there is reduced neurological compromise. [22]
Burst fractures – make up only 10% of all thoracolumbar injuries in paediatrics due to the increase in spinal flexibility, meaning the pressure is not concentrated in one area - the common cause of burst fractures. This also reduces neurological damage along the increased size of the paediatric spinal canal compared to the spinal cord and cauda equina. [22]
Chance fracture – common in children when wearing lap belts in motor traffic accidents. The seat belt acts as a fulcrum causing hyperflexion, commonly seen alongside intra-abdominal and head injuries. [22]
Apophyseal ring fractures - only found in the paediatric population. Normally seen in adolescents and occurs due to the ring apophysis and the vertebral body not fusing completely and may separate in the process. [23]
Characteristics/ Clinical Presentation[edit | edit source]
A 10 year report at a children's university hospital found symptoms were as follows: [21] [22]
C-spine Fracture[edit | edit source]
- neurological deficit
- fixed abnormal head positions
- Common Additional Injuries - facial/head injuries, skull and facial fractures, facial lacerations, intercranial injury
T-spine Fracture[edit | edit source]
- back pain
- ecchymoses (skin discolouration due to bleeding below skin)
- localised tenderness
- neurological deficit
- Common Additional injuries - simple or multiple rib fractures, fractured sternum, pulmonary contusion, abdominal/visceral injuries including splenic haematoma
L-spine Fracture[edit | edit source]
- Back pain
- ecchymoses (skin discolouration due to bleeding below skin)
- localised tenderness
- abdominal pain
Due to children having a larger spinal canal than their spinal cord they can tolerate more compression than adults can before neural damage occurs
N/B: Ensure to look for fractures at all levels of the spine (C-spine, T-spine and L-spine) when assessing for potential spinal fracture in children. [21]
Fracture trends[edit | edit source]
- In children below 5 the most common area to injure was T8 followed by lumbar
- Between the ages of 5-10 the most common fracture area was the thoracolumbar region
- In teenagers the most common area begins to shift to the lumbar spine
- From 15 years and older the lumbar area is most affected
Differential Diagnosis[edit | edit source]
- Low Back Pain
- Spondylosis
- Juvenile Ankylosing Spondylitis
- Disc Herniation
- Spinal cord injury without radiographic abnormality
Diagnostic Procedures[edit | edit source]
- Sensation of ‘breath arrest’ - immediately after the trauma the children would feel extremely short of breath, this is a predictive factor for vertebral fracture, particularly thoracolumbar fractures.
- X-ray – due to the cartilaginous nature of the vertebra, fractures are not always clear from routine x-rays and children can go undiagnosed.
- MRI – used to determine diagnosis of potential fractures shown on x-ray. They give clear images of the vertebra allowing for more accurate diagnosis. This allows for direct visualisation and confirmation of the fracture, where it is in the spine and what type of fracture has occurred.
- CT scan – these have better prognostic ability than x-ray as they show bony details in higher definition than an x-ray. It is therefore more likely to get a clear diagnosis from a CT scan than an x-ray. However, like with x-rays fractures can go unnoticed on CT scans, therefore if there is any doubt about the potential of a fracture it should be followed up with an MRI scan to clarify a potential diagnosis.
- Flexion/Extension C-spine x-rays – often used after CT scans if no findings are present to determine if there is any undiagnosed cervical instability [24][25][26]
Other Diagnostic Tools[edit | edit source]
Nexus criteria[edit | edit source]
National Emergency R-ray Utilisation Group criteria assesses low-risk patients for cervical spine injury. It is primarily used to determine if an x-ray is required or if further imaging is needed after an x-ray to determine possible diagnosis.
Nexus criteria: [27]
- Absence of midline cervical tenderness
- No evidence of intoxication
- Normal level of alertness
- Normal neurological exam
- Absence of a painful, distracting injury
Canadian C-spine Rule[edit | edit source]
These are a set of guidelines to help a clinician decide if cervical imaging (i.e. x-ray, CT or MRI) are appropriate for trauma patients. For children however, consideration needs to be taken around developmental stage, so applying these rules can be difficult.
C-spine rules: [28]
- Any high-risk factors which mandate radiography
- Dangerous mechanism of injury
- Age > 65
- Paraesthesia in extremities
- Any low-risk factor which allows safe assessment of range of motion
- Simple rear-end motor vehicle collision
- Sitting position in ED
- Ambulatory at any time
- Delayed onset of neck pain
- Absence of midline spine tenderness
- Able to actively rotate neck
- 45 degrees left and right
Management[edit | edit source]
Conservative Management[edit | edit source]
Casting[edit | edit source]
There are two types: Minerva and Plaster and they usually stay on for a period of around 2 months.
Halo Vests[edit | edit source]
To be worn for an average of 8 weeks.
Bed Rest[edit | edit source]
Until acute symptoms subside, followed by a moulded body cast.
Conservative management, particularly of wedge fractures without neurological lesions can be successful, leaving only moderate residual deformities. However, it is important there is an accurate diagnosis to confirm the stability of the fracture to ensure accurate treatment is provided.Whilst nonoperative treatment is viable for burst fractures in children with no neurological deficits and minimal initial kyphosis, operative treatments are recommended for unstable burst fractures to correct the deformity. [18]
Angelliaume et al, 2017: [29]
- In a case of a stable spinal fracture without neurological deficiency, conservative treatment must be the first treatment of choice in children
- The significant difference between the initial and the final local kyphosis at the thoracic level was not found for the lumbar level.
- It is hypothesised that the brace is more efficient at the thoracic level than at the lumbar level and enables more remodelling, decreasing compressive forces by an antikyphotic effect- furthermore, it is easier to correct a thoracic kyphosis than a lumbar one using an antikyphotic brace
Functional outcomes[edit | edit source]
- Functional results indicated a high rate of back pain.
- However, patients’ functional results were satisfactory because they reported no limitations in their daily life activities and did not use painkillers.
- Variable rates of functional outcomes have been reported, with 12–57% incidences of back pain after a conservative treatment
- However, rates of back pain in adolescents without back injury are also high, with a prevalence of 7–70% .
Surgical Management[edit | edit source]
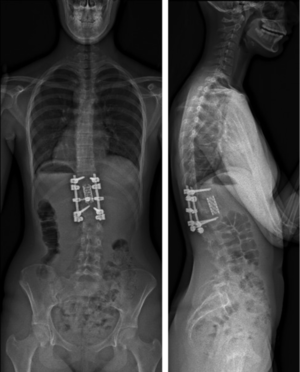
Overall surgical interventions depend on the type and severity of the fracture. The Denis classification can be used to differentiate between a stable and a unstable vertebral fracture which can help decide on management options. Generally according to the evidence, lots of stable fractures can be treated conservatively however unstable fractures will require surgical management. [18] [30] Furthermore, if the patient has a neurological deficit or a spinal cord injury, surgery is necessary to stabilise the fracture and gain neurological function. [31] Surgical outcomes within the population have been positive. Vander Have et al. [32] found that surgical intervention was positive in ensuring the correction of the kyphosis of the spine compared to conservative management that which led to worsening of kyphosis.
Types of surgery can vary depending on the type of fracture and the age. Adolescents can be treated using adult type instrumentation due to a more developed spine [30] whereas, younger children have smaller pedicles so a normal screw placement in this area can be challenging. [30] Evidence suggests a shorted fusion is the prefered approach in peadiactric fractures in order to preserve growth and mobility. [33] In the lumbar spine, lumbar fusion can be used which involves fusing the vertebral bodies together so no movement can occur between them enabling the fracture to be repaired, this can be managed via a posterior approach. [34] If the fracture is more severe, reconstruction surgery such as vertebroplasty or kyphoplasty can take place. [34] Although conservative management has been proven to correct initial conditions and deformities, these deformities can return overtime leading to a short term fix as opposed to a long term fix.
Prevention[edit | edit source]
Over recent years, there has been an increased recognition of the need to identify children with bone fragility, [35] this is due to osteoporosis being thought to root from childhood therefore preventative efforts should be initiated in early life to ensure life-long bone health. [36]
- Calcium: intake during infancy, childhood and adolescence contribute to bone mass gain. Dietary supplementations may be offered to those who cannot take in enough calcium. [36]
- Vitamin D: testing for vitamin D deficiency is recommended for those who have recurrent traumatic fractures even on low-impact. [36]
- Mechanical loading and weight bearing exercise: puts force on the skeleton that increases bone formation. [36]
Dual Energy X-ray absorptiometry (DXA) is considered the gold standard for the assessment for bone mass as it is preferred due to low radiation. [36] It is reported that an association occurs between low bone mass measured using DXA and increased fracture risk in children.[36]
There is a need to assess each child on an individual basis to identify if they need a bone health evaluation. In the diagram below,[36] it can be seen what health factors should be considered in the decision of whether to conduct a bone health evaluation. [35]
An additional consideration is road traffic safety. Leonard et al. [22] found in their study of paediatric spinal trauma that children who were restrained by a lap belt in the rear of a vehicle whereby a head on collision occurred led to hyperflexion of their spine and resulting in intra-abdominal and head injuries. [22] To prevent these injuries from occuring, it is recommended that cross-body seat belts and booster seats be used to strap chiodren in vehicles.
References[edit | edit source]
- ↑ Todd S., Di Marco M. Vertebral Fractures in Children. NHS Greater Glasgow and Clyde. Available from:https://www.smn.scot.nhs.uk/wp-content/uploads/2019/01/Vertebral-fractures-in-children.pdf [Accessed 11/3/2023].
- ↑ 2.0 2.1 Lustrin E., Karakas S., Ortiz A., Cinnamon J., Castillo M., Vaheesan K., Brown J., Diamond A., Black K., Singh S. Pediatric cervical spine: normal anatomy, variants, and trauma. Radiographics. 2003 May;23(3):539-60.
- ↑ 3.0 3.1 3.2 Gray H., Bannister L., Berry M., Williams P. Gray's anatomy. 37th ed. Philadelphia, Pa: Lea and Febiger; 1989.
- ↑ 4.0 4.1 4.2 4.3 Harris J., Harris J., Mirvis S. The radiology of acute cervical spine trauma. Lippincott Williams & Wilkins; 1996.
- ↑ 5.0 5.1 5.2 Herman M., Pizzutillo P. Cervical spine disorders in children. Orthop Clin North Am. 1999 Jul 1;30(3):457-66.
- ↑ 6.0 6.1 Ogden J. Radiology of postnatal skeletal development. Skeletal Radiology. 1984 Sep;12(3):169-77.
- ↑ 7.0 7.1 7.2 Swischuk L. Emergency imaging of the acutely ill or injured child. Lippincott Williams & Wilkins; 2000.
- ↑ Bailey D. The normal cervical spine in infants and children. Radiology. 1952 Nov;59(5):712-9.
- ↑ Cattell H., Filtzer D. Pseudosubluxation and other normal variations in the cervical spine in children: A study of one hundred and sixty children. JBJS. 1965 Oct 1;47(7):1295-309.
- ↑ Kokoska E., Keller M., Rallo M., Weber T.. Characteristics of pediatric cervical spine injuries. J Ped Surg. 2001 Jan 1;36(1):100-5.
- ↑ 11.0 11.1 Roche C., Carty H. Spinal trauma in children. Pediatric Radiology. 2001 Oct;31(10):677-700.
- ↑ McGrory B., Klassen R., Chao E., Staeheli J., Weaver A. Acute fractures and dislocations of the cervical spine in children and adolescents. J Bone Joint Surg. American volume. 1993 Jul 1;75(7):988-95.
- ↑ Davis B. Media Reviews. Rosen's Emergency Medicine: Concepts and Clinical Practice. Prehosp Emerg Care. 2004 Jan 1;8(3):334-5.
- ↑ Bilston L., Brown J. Pediatric spinal injury type and severity are age and mechanism dependent. Spine. 2007 Oct 1;32(21):2339-47.
- ↑ Giglio C., Volpon J. Development and evaluation of thoracic kyphosis and lumbar lordosis during growth. J Child Orthop. 2007 Sep 1;1(3):187-93.
- ↑ Dimeglio A., Canavese F. The growing spine: how spinal deformities influence normal spine and thoracic cage growth. Eur Spine J. 2012 Jan;21(1):64-70.
- ↑ 17.0 17.1 Bouyer B., Vassal M., Zairi F., Dhenin A., Grelat M., Dubory A., Giorgi H., Walter A., Lonjon G., Dauzac C., Lonjon N. Surgery in vertebral fracture: epidemiology and functional and radiological results in a prospective series of 518 patients at 1 year's follow-up. Orthop Traumatol Surg Res. 2015 Feb 1;101(1):11-5.
- ↑ 18.0 18.1 18.2 18.3 Parisini P., Di Silvestre M., Greggi T. Treatment of spinal fractures in children and adolescents: long-term results in 44 patients. Spine. 2002 Sep 15;27(18):1989-94.
- ↑ 19.0 19.1 19.2 Tan V., Macdonald H., Kim S., Nettlefold L., Gabel L., Ashe M., McKay H. Influence of physical activity on bone strength in children and adolescents: a systematic review and narrative synthesis. J Bone Mineral Res. 2014 Oct;29(10):2161-81.
- ↑ 20.0 20.1 Boreham C., McKay H. Physical activity in childhood and bone health. Br J Sports Med. 2011 Sep 1;45(11):877-9.
- ↑ 21.00 21.01 21.02 21.03 21.04 21.05 21.06 21.07 21.08 21.09 21.10 Saul D., Dresing K. Epidemiology of vertebral fractures in pediatric and adolescent patients. Pediatr Rep. 2018 Mar;10(1):17-23.
- ↑ 22.00 22.01 22.02 22.03 22.04 22.05 22.06 22.07 22.08 22.09 22.10 Leonard M., Sproule J., Mc Cormack D. Paediatric spinal trauma and associated injuries. Injury. 2007 Feb 1;38(2):188-93.
- ↑ Ravi Kumar T., Rao R., Gadi D., Grover A. Lumbar apophyseal ring fracture-a case report. JCDR. 2015 May;9(5):RD01.
- ↑ Leroux J., Vivier P., Slimane M., Foulongne E., Abu-Amara S., Lechevallier J., Griffet J. Early diagnosis of thoracolumbar spine fractures in children. A prospective study. Orthopaedics & Traumatology: Surgery & Research. 2013 Feb 1;99(1):60-5.
- ↑ Cui S., France J. Fractures of the Spine in Children. Available from: https://ota.org/sites/files/2018-06/P13-Fractures%20of%20the%20Spine%20in%20Children.pdf [Accessed 18//05/2021]
- ↑ Murphy A. Cervical spine (flexion and extension views). Radiopaedia. Available from: https://radiopaedia.org/articles/58732 [Accessed 18/05/2021]
- ↑ Stiell I., Clement C., Wells G., Morrison L. Prospective validation of the NEXUS low-risk criteria for cervical spine radiography. CJEM 2002 Mar 1;4(2):129.
- ↑ Fox S.. Paediatric Cervical Spine Injury. Paediatric EM Morsels: Paediatric Emergency Medicine Education. Available from: https://pedemmorsels.com/pediatric-cervical-spine-injury/ [Accessed 18/05/2021]
- ↑ Angelliaume A., Simon A., Boissière L., Bouty A., Sales de Gauzy J., Vital J., Gille O., Tournier C., Aunoble S., Pontailler J., Lefèvre Y. Conservative treatment of pediatric thoracic and lumbar spinal fractures: outcomes in the sagittal plane. J Pediatr Orthop B. 2016 Jan 1;26(1):73-9.
- ↑ 30.0 30.1 30.2 30.3 Sayama C., Chen T., Trost G., Jea A. A review of pediatric lumbar spine trauma. Neurosurgical Focus. 2014 Jul 1;37(1):E6.
- ↑ Ferrero E., Compagnon R., Pesenti S., Lefèvre Y., Polirsztok E., Ilharreborde B., de Gauzy J. Surgical management of burst fractures in children and adolescents: A Multicentre Retrospective Study. Orthopaedics & Traumatology: Surgery & Research. 2020 Feb 1;106(1):173-8.
- ↑ Vander Have K., Caird M., Gross S., Farley F., Graziano G., Stauff M., Segal L. Burst fractures of the thoracic and lumbar spine in children and adolescents. J Pediatr Orthop. 2009 Oct 1;29(7):713-9.
- ↑ Lalonde F., Letts M., Yang J., Thomas K. An analysis of burst fractures of the spine in adolescents. Am J Orthop. 2001 Feb 1;30(2):115-20.
- ↑ 34.0 34.1 Boddu S. Spinal Compression Fractures. Weill Cornell Brain and Spine Centre. Available from: https://weillcornellbrainandspine.org/condition/spinal-compression-fractures/surgery-spinal-compression-fractures [Accessed 12/03/2023]
- ↑ 35.0 35.1 35.2 Ward L., Weber D., Munns C., Högler W., Zemel B. A contemporary view of the definition and diagnosis of osteoporosis in children and adolescents. J Clin Endocrinol Metab. 2020 May;105(5):e2088-97.
- ↑ 36.0 36.1 36.2 36.3 36.4 36.5 36.6 Golden N., Abrams S. Optimizing bone health in children and adolescents. Pediatrics. 2014 Oct 1;134(4):e1229-43.