Contracted Pelvis: Difference between revisions
No edit summary |
No edit summary |
||
| (22 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[Temitope Olowoyeye|Temitope Olowoyeye]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | <div class="editorbox"> '''Original Editor '''- [[User:Temitope Olowoyeye|Temitope Olowoyeye]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== | == Introduction == | ||
Contracted pelvis considered rare in the developed world, is still prevalent in some developing countries.<ref name=":0">Bhosale A, Fonseca M, Nandanwar YS. [https://www.bhj.org.in/journal/2010-5201-jan/download/pg138-140.pdf Obstructed Labour Due to Contracted Pelvis in a Grand Multiparous Woman.] Bombay Hospital Journal. 2010;52(1):139.</ref> The contracted pelvis is the major cause of cephalopelvic disproportion, [[Labour Dystocia]], and instrumental delivery.<ref name=":5">Siccardi M, Valle C, Di Matteo F. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8011468/ Dynamic external pelvimetry test in third trimester pregnant women: shifting positions affect pelvic biomechanics and create more room in obstetric diameters.] Cureus. 2021 Mar 1;13(3).</ref> [[Labour Dystocia]] is the most common complication associated with a contracted pelvis which leads to increased incidence of perinatal and maternal morbidity as well as mortality. | |||
It is described as one with reduced pelvic dimensions or shape that is sufficiently abnormal to cause difficulty in the delivery of a normal-sized fetus during [[labour|labor]]<ref name=":0" /> <ref name=":1">Amiel GJ. [https://link.springer.com/chapter/10.1007/978-94-011-7233-2_18 Contracted pelvis and disproportion.] InEssential Obstetric Practice 1981 (pp. 167-175). Dordrecht: Springer Netherlands.</ref> | |||
== The female pelvis == | |||
In obstetrics, the shape, type, and diameter of the female [[pelvis]] determine the course and outcome of labor.<ref name=":1" /><ref name=":2">Salk I, Cetin M, Salk S, Cetin A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5588557/#:~:text=Although%20pelvises%20can%20be%20classified,the%20pelvic%20inlet%20%5B5%5D. Determining the incidence of gynecoid pelvis using three-dimensional computed tomography in nonpregnant multiparous women.] Medical Principles and Practice. 2016;25(1):40-8.</ref> The [[pelvis]] is made up of the sacrum, the coccyx, and two os coxae Each os coxae is made up of the ischium, the ilium, and the pubis. The pelvis is formed inferiorly between the sacrum and the coccyx (sacrococcygeal symphysis), posteriorly between the sacrum and each ilium ([[Sacroiliac Joint|sacroiliac joint]]), and anteriorly between the pubic bodies (pubic symphysis). <ref name=":02">Lewis CL, Laudicina NM, Khuu A, Loverro KL. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5545133/ The human pelvis: variation in structure and function during gait.] The Anatomical Record. 2017 Apr;300(4):633-42.</ref> | |||
= | The pelvic cavity is divided into the true [[pelvis]] and the false pelvis by the pelvic inlet.<ref name=":02" /> | ||
The pelvic inlet, is the anatomical limit between the true pelvis below and the false pelvis above, and its regarded as the doorway to the birth canal in obstetrics<ref name=":3">Siccardi MA, Imonugo O, Valle C. [https://www.ncbi.nlm.nih.gov/books/NBK519068/ Anatomy, Abdomen and Pelvis, Pelvic Inlet.]</ref>. The pelvic inlet involves three of the four units of which the bone pelvis is composed. The pelvic brim involves the first sacral segment, the iliac and pubis portion, but not the ischium. The dimensions of the pelvic inlet are determined by the general shape of the female pelvis.<ref name=":3" /> | |||
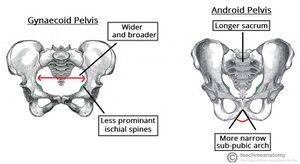
[[File:Gynaecoid and android pelvis.jpg|thumb]] | |||
The shape of the pelvic inlet depends on the general shape of the pelvis. Caldwell and Moloy classified the female pelvis into 4 basic pelvic types which are, in order of frequency, gynaecoid (∼50%), android, anthropoid, and platypelloid.<ref name=":2" /><ref>Caldwell WE, Moloy HC. [https://journals.sagepub.com/doi/pdf/10.1177/003591573803200101 Anatomical variations in the female pelvis and their effect in labor with a suggested classification.] American Journal of Obstetrics and Gynecology. 1933 Oct 1;26(4):479-505.</ref> | |||
== | The gynaecoid pelvis is the most suitable for a vaginal birth, the anthropoid pelvis is acceptably favorable. The android and platypelloid are known to be suboptimal.<ref name=":2" /><ref name=":0" /> | ||
The diameters of the pelvic inlet can be defined as | |||
The anteroposterior (or "conjugate") diameter is the distance between the pubic symphysis and the sacral promontory. Three distances are: | |||
* The anatomical conjugate or true: Measured between the sacral promontory and the upper edge of the pubic symphysis and measures an average of 11.0 cm | |||
* The obstetric conjugate: Measured from the sacral promontory to the point bulging the most on the back of the symphysis pubis, located about 1 cm below its upper border. It measures 10.5 cm on average; it is the lesser anteroposterior diameter. | |||
* The diagonal conjugate: Measured between the sacral promontory and the lower edge of the pubic symphysis, measuring an average of 12.5.<ref name=":4">Ministry of Public Heals Service of Ukraine: [https://akusher-one.pdmu.edu.ua/storage/resources/docs/KThomqvjHYGTreVLc72zaBwjLia0ZrgmhfthzBo6.pdf METHODICAL POINTING for the independent work of students for preparation to practical lesson 2020] Available from: <nowiki>https://akusher-one.pdmu.edu.ua/storage/resources/docs/KThomqvjHYGTreVLc72zaBwjLia0ZrgmhfthzBo6.pdf</nowiki> [Accessed 23rd Feb 2023].</ref> | |||
A contracted pelvis is established when the pelvic inlet at the interaxial dimension is less than 10 cm; this is viewed as a suspicion of the contracted pelvis, and when it is less than 8 cm it is viewed as a contracted pelvis.<ref name=":4" />{{#ev:youtube|kTwxNTFP-YA|300}}<ref name=":6">Human Anatomy Education. Female bony pelvis: 3-Pelvimetry. Available from: http://www.youtube.com/watch?v=kTwxNTFP-YA [last accessed 21/2/2023]</ref> | |||
== Causes == | |||
* Developmental | |||
* Metabolic: Rickets, [[Osteomalacia]] | |||
* Traumatic: fractures. | |||
* Neoplastic: osteoma. | |||
* Lumbar kyphosis. | |||
* Lumbar [[scoliosis]]. | |||
* [[Spondylolisthesis]]: The 5th lumbar vertebra with the above vertebral column is pushed forward while the promontory is pushed backward and the tip of the sacrum is pushed forwards leading to outlet contraction. | |||
= | * Dislocation of one or both femurs. | ||
* Atrophy of one or both lower limbs.<ref name=":4" /> | |||
== Diagnosis of contracted pelvis == | |||
Abdominal examination: | |||
* Nonengagement of the head: in the last 3-4 weeks in primigravida. | |||
* Pendulous abdomen: in a primigravida. | |||
* Malpresentations: are more common. | |||
Pelvimetry: It is assessment of the pelvic diameters and capacity done at 38-39 weeks.<ref name=":5" /><ref>Liselele HB, Tshibangu CK, Meuris S. [https://obgyn.onlinelibrary.wiley.com/doi/full/10.1034/j.1600-0412.2000.079008673.x Association between external pelvimetry and vertex delivery complications in African women.] Acta Obstetricia et Gynecologica Scandinavica: ORIGINAL ARTICLE. 2000 Aug;79(8):673-8.</ref> | |||
It includes internal pelvimetry (vaginal examination) for: | |||
* inlet, | |||
* cavity, and | |||
* outlet. | |||
External pelvimetry for ( Dynamic exteral pelvimetry test): <ref name=":6" /><ref name=":7">Siccardi M, Valle C, Di Matteo F, Angius V. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6901367/ A postural approach to the pelvic diameters of obstetrics: the dynamic external pelvimetry test.] Cureus. 2019 Nov 9;11(11).</ref><ref>Siccardi M, Valle C, Di Matteo F, Angius V. [https://www.researchgate.net/profile/Marco-Siccardi/publication/338914031_Evaluating_Two_Postural_Change_Methods_For_The_Positional_Dynamic_Measurement_Of_The_Diameters_Of_The_Michaelis_Sacral_Rhomboid_Area/links/5e32a7ff299bf1cdb9fcfcd0/Evaluating-Two-Postural-Change-Methods-For-The-Positional-Dynamic-Measurement-Of-The-Diameters-Of-The-Michaelis-Sacral-Rhomboid-Area.pdf Evaluating two postural change methods for the positional dynamic measurement of the diameters of the Michaelis sacral rhomboid area.] J Reprod Med Gynecol Obstet. 2020;5:035.</ref> | |||
* inlet and | |||
* outlet. | |||
Imaging pelvimetry: | |||
* X-ray. | |||
* Computerised tomography (CT). | |||
* Magnetic resonance imaging (MRI) . | |||
CT and MRI are recent and accurate<ref name=":3" /> but expensive and not always available so they are not in common use in the developing countries. | |||
== Degrees of contracted pelvis == | |||
* Minor degree: The true conjugate is 9-10 cm. It corresponds to ma inor disproportion. | |||
* Moderate degree: The true conjugate is 8-9 cm. It corresponds to moderate disproportion. | |||
* Severe degree: The true conjugate is 6-8 cm. It corresponds to marked disproportion. | |||
* Extreme degree: The true conjugate is less than 6 cm.<ref name=":4" /> | |||
== Complications == | |||
Complications of Contracted Pelvis are; | |||
Mternal | |||
* Pendulous abdomen. | |||
* Nonengagement.<ref name=":8">Yeshitila YG, Daniel B, Desta M, Kassa GM. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9524671/ Obstructed labor and its effect on adverse maternal and fetal outcomes in Ethiopia]: A systematic review and meta-analysis. Plos one. 2022 Sep 30;17(9):e0275400.</ref> | |||
* Pyelonephritis especially in high assimilation pelvis due to more compression of the ureter.<ref name=":8" /> | |||
* Inertia, slow cervical dilatation and prolonged labour. | |||
* Premature rupture of membranes and cord prolapse.<ref name=":8" /><ref name=":9">Getachew, A., Wakgari, N. and Gishille, T., . [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8365494/ Feto-Maternal Outcomes of Obstructed Labor and Associated Factors among Mothers Who Gave Birth in Public Hospitals of West Shoa Zone, Central Ethiopia: Cross-Sectional Study] ''Ethiopian Journal of Health Sciences'',2021 ''31''(3).</ref> | |||
* Obstructed labour and rupture uterus.<ref name=":8" /> | |||
* Necrotic genito-urinary fistula.<ref name=":8" /> | |||
* Injury to pelvic joints or nerves from difficult instrumental delivery.<ref name=":8" /><ref name=":9" /> | |||
* Postpartum haemorrhage.<ref name=":8" /><ref name=":9" /> | |||
Foetus | |||
* Intracranial haemorrhage. | |||
* Birth asphyxia. <ref name=":9" /> | |||
* Fracture skull. | |||
* Nerve injuries. | |||
* Intra-amniotic infection.<ref name=":9" /> | |||
== Management == | |||
Timely management of contracted pelvis during [[labour]] is essential for the safety of both mother and foetus. However, management depends mainly on the degree of contraction.<ref name=":4" /> | |||
* Minor degree of contracted pelvis vaginal delivery is recommended. | |||
* Moderate degree of contracted pelvis trial labour, if failed caesarean section | |||
* Severe or extreme degree of contracted pelvis, caesarean section is required. | |||
Indications of caesarean section in contracted pelvis | |||
* Moderate disproportion if trial of labour is contraindicated or failed. | |||
* Marked disproportion. | |||
* Extreme disproportion whether the foetus is living or dead. | |||
* Contracted outlet. | |||
* Contracted pelvis with other indications as; | |||
* elderly primigravida, | |||
* malpresentations, or | |||
* placenta previa. | |||
== Implications for physiotherapy == | |||
Adequate knowledge of contracted pelvis, degrees and the process of [[labour|labor]] would greatly enhance physiotherapy interventions in the management of contracted [[pelvis]]. Postural change during labour may have an effect on progress in labour as postural change enhances uterine activity,<ref>Borba EO, Amarante MV, Lisboa DD. [https://www.scielo.br/j/fp/a/pWvNrWw9mSnLQ8Wsgsd7zGR/?format=pdf&lang=en Physiotherapeutic assistance during labor.] Fisioterapia e Pesquisa. 2021 Nov 26;28:324-30.</ref> increasing the dimensions of pelvis. <ref name=":7" /> Increased maternal pelvic dimensions are believed to contribute to the reduction of the incidence of failure of labour to progress, ease of delivery of the baby, and reduced risk of cesarean birth during [[labour]].<ref name=":7" /> | |||
Physiotherapy is recommended in the minor and moderate contracted pelvis and is targeted at postural changes that would encourage an increase in the pelvic inlet diameters. | |||
Also, Physiotherapy has been found efficient to reduce pain, duration of labor, anxiety, laceration, and episiotomy.<ref>Biana CB, Cecagno D, Porto AR, Cecagno S, Marques VD, Soares MC. N[https://www.scielo.br/j/reeusp/a/hFW77ZFvW6MbsJfqMD53yvp/?lang=en on-pharmacological therapies applied in pregnancy and labor: an integrative review.] Revista da Escola de Enfermagem da USP. 2021 Apr 16;55.</ref> | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Womens Health]] | |||
[[Category:Pregnancy]] | |||
[[Category:Pelvis]] | |||
[[Category:Pelvic Health]] | |||
Latest revision as of 11:58, 28 February 2023
Introduction[edit | edit source]
Contracted pelvis considered rare in the developed world, is still prevalent in some developing countries.[1] The contracted pelvis is the major cause of cephalopelvic disproportion, Labour Dystocia, and instrumental delivery.[2] Labour Dystocia is the most common complication associated with a contracted pelvis which leads to increased incidence of perinatal and maternal morbidity as well as mortality.
It is described as one with reduced pelvic dimensions or shape that is sufficiently abnormal to cause difficulty in the delivery of a normal-sized fetus during labor[1] [3]
The female pelvis[edit | edit source]
In obstetrics, the shape, type, and diameter of the female pelvis determine the course and outcome of labor.[3][4] The pelvis is made up of the sacrum, the coccyx, and two os coxae Each os coxae is made up of the ischium, the ilium, and the pubis. The pelvis is formed inferiorly between the sacrum and the coccyx (sacrococcygeal symphysis), posteriorly between the sacrum and each ilium (sacroiliac joint), and anteriorly between the pubic bodies (pubic symphysis). [5]
The pelvic cavity is divided into the true pelvis and the false pelvis by the pelvic inlet.[5]
The pelvic inlet, is the anatomical limit between the true pelvis below and the false pelvis above, and its regarded as the doorway to the birth canal in obstetrics[6]. The pelvic inlet involves three of the four units of which the bone pelvis is composed. The pelvic brim involves the first sacral segment, the iliac and pubis portion, but not the ischium. The dimensions of the pelvic inlet are determined by the general shape of the female pelvis.[6]
The shape of the pelvic inlet depends on the general shape of the pelvis. Caldwell and Moloy classified the female pelvis into 4 basic pelvic types which are, in order of frequency, gynaecoid (∼50%), android, anthropoid, and platypelloid.[4][7]
The gynaecoid pelvis is the most suitable for a vaginal birth, the anthropoid pelvis is acceptably favorable. The android and platypelloid are known to be suboptimal.[4][1]
The diameters of the pelvic inlet can be defined as
The anteroposterior (or "conjugate") diameter is the distance between the pubic symphysis and the sacral promontory. Three distances are:
- The anatomical conjugate or true: Measured between the sacral promontory and the upper edge of the pubic symphysis and measures an average of 11.0 cm
- The obstetric conjugate: Measured from the sacral promontory to the point bulging the most on the back of the symphysis pubis, located about 1 cm below its upper border. It measures 10.5 cm on average; it is the lesser anteroposterior diameter.
- The diagonal conjugate: Measured between the sacral promontory and the lower edge of the pubic symphysis, measuring an average of 12.5.[8]
A contracted pelvis is established when the pelvic inlet at the interaxial dimension is less than 10 cm; this is viewed as a suspicion of the contracted pelvis, and when it is less than 8 cm it is viewed as a contracted pelvis.[8]
Causes[edit | edit source]
- Developmental
- Metabolic: Rickets, Osteomalacia
- Traumatic: fractures.
- Neoplastic: osteoma.
- Lumbar kyphosis.
- Lumbar scoliosis.
- Spondylolisthesis: The 5th lumbar vertebra with the above vertebral column is pushed forward while the promontory is pushed backward and the tip of the sacrum is pushed forwards leading to outlet contraction.
- Dislocation of one or both femurs.
- Atrophy of one or both lower limbs.[8]
Diagnosis of contracted pelvis[edit | edit source]
Abdominal examination:
- Nonengagement of the head: in the last 3-4 weeks in primigravida.
- Pendulous abdomen: in a primigravida.
- Malpresentations: are more common.
Pelvimetry: It is assessment of the pelvic diameters and capacity done at 38-39 weeks.[2][10]
It includes internal pelvimetry (vaginal examination) for:
- inlet,
- cavity, and
- outlet.
External pelvimetry for ( Dynamic exteral pelvimetry test): [9][11][12]
- inlet and
- outlet.
Imaging pelvimetry:
- X-ray.
- Computerised tomography (CT).
- Magnetic resonance imaging (MRI) .
CT and MRI are recent and accurate[6] but expensive and not always available so they are not in common use in the developing countries.
Degrees of contracted pelvis[edit | edit source]
- Minor degree: The true conjugate is 9-10 cm. It corresponds to ma inor disproportion.
- Moderate degree: The true conjugate is 8-9 cm. It corresponds to moderate disproportion.
- Severe degree: The true conjugate is 6-8 cm. It corresponds to marked disproportion.
- Extreme degree: The true conjugate is less than 6 cm.[8]
Complications[edit | edit source]
Complications of Contracted Pelvis are;
Mternal
- Pendulous abdomen.
- Nonengagement.[13]
- Pyelonephritis especially in high assimilation pelvis due to more compression of the ureter.[13]
- Inertia, slow cervical dilatation and prolonged labour.
- Premature rupture of membranes and cord prolapse.[13][14]
- Obstructed labour and rupture uterus.[13]
- Necrotic genito-urinary fistula.[13]
- Injury to pelvic joints or nerves from difficult instrumental delivery.[13][14]
- Postpartum haemorrhage.[13][14]
Foetus
- Intracranial haemorrhage.
- Birth asphyxia. [14]
- Fracture skull.
- Nerve injuries.
- Intra-amniotic infection.[14]
Management[edit | edit source]
Timely management of contracted pelvis during labour is essential for the safety of both mother and foetus. However, management depends mainly on the degree of contraction.[8]
- Minor degree of contracted pelvis vaginal delivery is recommended.
- Moderate degree of contracted pelvis trial labour, if failed caesarean section
- Severe or extreme degree of contracted pelvis, caesarean section is required.
Indications of caesarean section in contracted pelvis
- Moderate disproportion if trial of labour is contraindicated or failed.
- Marked disproportion.
- Extreme disproportion whether the foetus is living or dead.
- Contracted outlet.
- Contracted pelvis with other indications as;
- elderly primigravida,
- malpresentations, or
- placenta previa.
Implications for physiotherapy[edit | edit source]
Adequate knowledge of contracted pelvis, degrees and the process of labor would greatly enhance physiotherapy interventions in the management of contracted pelvis. Postural change during labour may have an effect on progress in labour as postural change enhances uterine activity,[15] increasing the dimensions of pelvis. [11] Increased maternal pelvic dimensions are believed to contribute to the reduction of the incidence of failure of labour to progress, ease of delivery of the baby, and reduced risk of cesarean birth during labour.[11]
Physiotherapy is recommended in the minor and moderate contracted pelvis and is targeted at postural changes that would encourage an increase in the pelvic inlet diameters.
Also, Physiotherapy has been found efficient to reduce pain, duration of labor, anxiety, laceration, and episiotomy.[16]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Bhosale A, Fonseca M, Nandanwar YS. Obstructed Labour Due to Contracted Pelvis in a Grand Multiparous Woman. Bombay Hospital Journal. 2010;52(1):139.
- ↑ 2.0 2.1 Siccardi M, Valle C, Di Matteo F. Dynamic external pelvimetry test in third trimester pregnant women: shifting positions affect pelvic biomechanics and create more room in obstetric diameters. Cureus. 2021 Mar 1;13(3).
- ↑ 3.0 3.1 Amiel GJ. Contracted pelvis and disproportion. InEssential Obstetric Practice 1981 (pp. 167-175). Dordrecht: Springer Netherlands.
- ↑ 4.0 4.1 4.2 Salk I, Cetin M, Salk S, Cetin A. Determining the incidence of gynecoid pelvis using three-dimensional computed tomography in nonpregnant multiparous women. Medical Principles and Practice. 2016;25(1):40-8.
- ↑ 5.0 5.1 Lewis CL, Laudicina NM, Khuu A, Loverro KL. The human pelvis: variation in structure and function during gait. The Anatomical Record. 2017 Apr;300(4):633-42.
- ↑ 6.0 6.1 6.2 Siccardi MA, Imonugo O, Valle C. Anatomy, Abdomen and Pelvis, Pelvic Inlet.
- ↑ Caldwell WE, Moloy HC. Anatomical variations in the female pelvis and their effect in labor with a suggested classification. American Journal of Obstetrics and Gynecology. 1933 Oct 1;26(4):479-505.
- ↑ 8.0 8.1 8.2 8.3 8.4 Ministry of Public Heals Service of Ukraine: METHODICAL POINTING for the independent work of students for preparation to practical lesson 2020 Available from: https://akusher-one.pdmu.edu.ua/storage/resources/docs/KThomqvjHYGTreVLc72zaBwjLia0ZrgmhfthzBo6.pdf [Accessed 23rd Feb 2023].
- ↑ 9.0 9.1 Human Anatomy Education. Female bony pelvis: 3-Pelvimetry. Available from: http://www.youtube.com/watch?v=kTwxNTFP-YA [last accessed 21/2/2023]
- ↑ Liselele HB, Tshibangu CK, Meuris S. Association between external pelvimetry and vertex delivery complications in African women. Acta Obstetricia et Gynecologica Scandinavica: ORIGINAL ARTICLE. 2000 Aug;79(8):673-8.
- ↑ 11.0 11.1 11.2 Siccardi M, Valle C, Di Matteo F, Angius V. A postural approach to the pelvic diameters of obstetrics: the dynamic external pelvimetry test. Cureus. 2019 Nov 9;11(11).
- ↑ Siccardi M, Valle C, Di Matteo F, Angius V. Evaluating two postural change methods for the positional dynamic measurement of the diameters of the Michaelis sacral rhomboid area. J Reprod Med Gynecol Obstet. 2020;5:035.
- ↑ 13.0 13.1 13.2 13.3 13.4 13.5 13.6 Yeshitila YG, Daniel B, Desta M, Kassa GM. Obstructed labor and its effect on adverse maternal and fetal outcomes in Ethiopia: A systematic review and meta-analysis. Plos one. 2022 Sep 30;17(9):e0275400.
- ↑ 14.0 14.1 14.2 14.3 14.4 Getachew, A., Wakgari, N. and Gishille, T., . Feto-Maternal Outcomes of Obstructed Labor and Associated Factors among Mothers Who Gave Birth in Public Hospitals of West Shoa Zone, Central Ethiopia: Cross-Sectional Study Ethiopian Journal of Health Sciences,2021 31(3).
- ↑ Borba EO, Amarante MV, Lisboa DD. Physiotherapeutic assistance during labor. Fisioterapia e Pesquisa. 2021 Nov 26;28:324-30.
- ↑ Biana CB, Cecagno D, Porto AR, Cecagno S, Marques VD, Soares MC. Non-pharmacological therapies applied in pregnancy and labor: an integrative review. Revista da Escola de Enfermagem da USP. 2021 Apr 16;55.