|
|
| (11 intermediate revisions by 3 users not shown) |
| Line 1: |
Line 1: |
| <div class="editorbox"> '''Original Editor '''- [[User:Jaleel Mohammed|Jaleel Mohammed] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | | <div class="editorbox"> '''Original Editor '''- [[User:Jaleel Mohammed|Jaleel Mohammed]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> |
| ==Introduction== | | ==Introduction== |
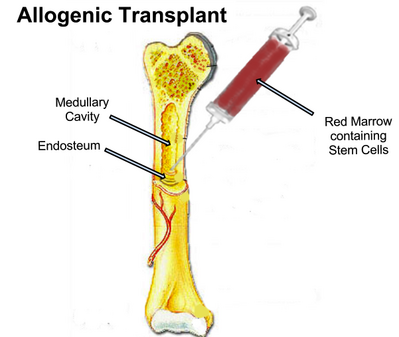
| Chronic graft-versus-host disease (cGVHD) is a common and potentially life-threatening complication which develops as a result of allogeneic hematopoietic cell transplantation (HCT), when the transplanted cells react against the body of the recipient. The prevalence of this disease, unfortunately, varies from between 25–80% in long-term survivors. cGVHD can lead to serious physical and functional impairment that affects the quality of life as it is often diagnosed late in its course when the disability has already begun.
| | [[File:Bone Marrow Transplant.png|399x399px|alt=|thumb|Bone Marrow Transplant]]Graft versus host disease (GvHD) is a very common complication of [[Bone Marrow|bone marrow]] transplantations ( also known as allogeneic haematopoietic stem cell transplantation). Anti-rejection drugs have decreased the incidence, however it still occurs regularly.<ref name=":0">Radiopedia [https://radiopaedia.org/articles/graft-versus-host-disease Graft versus host disease] Available: https://radiopaedia.org/articles/graft-versus-host-disease<nowiki/>(accessed 28.1.2023)</ref> |
|
| |
|
| ====What are the Signs and Symptoms of GVHD?====
| | GvHD cause significant damage to the tissues affected, directly contributing to functional impairment. Treatment typically involves high-dose [[Corticosteroid Medication|corticosteroids]] to suppress the [[Immune System|immune system]] which can be destructive. [[Rehabilitation Contexts|Rehabilitation]] often is required to restore function and [[Quality of Life|quality of life]].<ref>Smith SR, Asher A. [https://www.sciencedirect.com/science/article/abs/pii/S1047965116300717?via%3Dihub Rehabilitation in chronic graft-versus-host disease.] Physical Medicine and Rehabilitation Clinics. 2017 Feb 1;28(1):143-51.Available: https://www.sciencedirect.com/science/article/abs/pii/S1047965116300717?via%3Dihub (accessed 29.1.2023)</ref> |
|
| |
|
| ''' Acute GVHD:''' In the early weeks and months after your transplant (usually within the first four months) you might notice a rash, or an upset stomach with nausea, vomiting or diarrhoea, or it could affect your liver tests, sometimes causing jaundice (yellow discolouration to the skin).
| | == Pathology == |
| | Graft versus host disease presents either early/acute (<100 days) or late/chronic (>100 days) post bone marrow transplantation, being a major complication. The skin, gastrointestinal tract (in particular the small bowel), and liver are the organs most often affected.<ref name=":0" /> |
|
| |
|
| '''Chronic GVHD:''' Can happen a few months after transplant and can reoccur for several years after transplant. Like acute GVHD, it may affect your skin, gut, liver or mouth. But it can also affect other parts of your body, such as your eyes, lungs, vagina and joints. Chronic GVHD may be mild or severe, and for some people can go on for several months or even years.
| | ==How is GVHD Diagnosed?== |
|
| |
|
| '''What is the potential impact of musculoskeletal cGVHD on the Quality of Life (QoL) of the patients?'''
| | A clinical diagnosis is usually made. Typically diagnosis includes the following: |
| The number of long-term survivors after allogeneic HCT has been increasing over the past years, and quality of life (QOL) has become an important end-point. The QoL in this patient group can be affected due to:
| |
|
| |
|
| Decreased range of motion, significantly restricting a patient’s ability to perform activities of daily living.
| | # Immunologically competent cells present in the graft. |
| Painful joint contractures in some patients resulting in impaired function.
| | # The recipient has transplantation alloantigens appearing foreign to the graft and hence stimulate it antigenically. |
| Chronic graft versus host disease is an independent risk factor for joint destruction and associated pain and dysfunction.
| | # The recipient cannot mount an effective immunologic reaction against the graft, or enough time is allowed for the graft to manifest an immune response.<ref name=":1">Vaillant AA, Modi P, Mohammadi O. [https://www.ncbi.nlm.nih.gov/books/NBK538235/ Graft versus host disease.] InStatPearls [Internet] 2022 Jul 8. StatPearls Publishing.Available:https://www.ncbi.nlm.nih.gov/books/NBK538235/ (accessed 28.1.2023)</ref> |
| Some patients also show deteriorated role functioning and global QOL, increased fatigue, and skin problems.
| |
| The long-term sexual complications include decreased libido, vaginal alterations, erectile and ejaculatory dysfunctions.
| |
| Due to physical dysfunction, many patients also struggle to return to work post cGVHD.
| |
|
| |
|
| ====How is GVHD diagnosed?== | | == Treatment == |
| | Treatment for GVHD is determined by the severity of symptoms and organs involved. Treatment options are based on immunosuppression with corticosteroids being the most commonly used treatment.<ref name=":1" /> |
|
| |
|
| Some GVHD may be a good thing because it means that your new immune system is working and is likely to be attacking any remaining disease cells. This can help stop the disease from coming back. You might hear this called graft versus tumour effect.
| | ==What Are the Clinical Manifestations for cGVHD?== |
| | [[File:CGVHD.jpg|thumb|214x214px|Hand GVHD with Sclerosis]]Acute GVHD typically involves the skin, gastrointestinal tract, and liver. It may involve the lungs, kidneys, eyes, and hematopoietic system. Decreased responsiveness to active immunization may also occur. |
|
| |
|
| The early symptoms of GVHD are often the same as some side effects and complications after a transplant, so diagnosing GVHD can be hard. Although not definite some early signs might be clawing of the fingers in hand, reduce in ankle movement, skin changes and pain in the joints. Diagnosis is often made from your symptoms, as well as from the results of laboratory tests and tissue samples.
| | * Skin manifestation commonly arise as pruritic or painful maculopapular rash, first involving the palms, soles shoulders, and nape of the neck. |
| | * GI symptoms usually include diarrhea and abdominal pain, but mucositis, mucosal ulceration, nausea, and vomiting. Liver involvement usually include abnormal liver function tests with elevated bilirubin and alkaline phosphatase levels. |
|
| |
|
| ====What are the clinical manifestations for cGVHD?====
| | Chronic GVHD has a presentation similar to collagen vascular disorders and systemic sclerosis. Death may occur due to recurrent infections (as a complication of immunosuppression).<ref name=":1" /> |
| cGVHD can effect basically any organs, with the most commonly affected sites being: the skin, the mouth, the eyes, the gastrointestinal tract, the muscles and joints, the lungs, the liver, and genitalia. From a musculoskeletal point of view, the main organs involved are:
| |
| * SKIN
| |
| * FASCIA
| |
| * PERIPHERAL NERVES
| |
| * MUSCLE
| |
| * BONE (Due to use of cortisone)
| |
| Manifestations typically appear within the first year after HCT. The most commonly affected joints include fingers, wrists, elbows, shoulders, ankles, and hips, with the distal joints often affected first. cGVHD is an independent risk factor for joint destruction and associated pain and dysfunction.
| |
| [[File:CGVHD.jpg|thumb|214x214px|Hand GVHD with Sclerosis]]
| |
| '''Skin:'''
| |
|
| |
|
| Sclerotic-type chronic GVHD (ScGVHD) of the skin encompasses several cutaneous presentations characterized by inflammation and progressive fibrosis of the dermis and subcutaneous tissues, resembling morphea, systemic sclerosis, or eosinophilic fasciitis. One of the other distinctive feature for chronic GVHD is depigmentation.
| | == Physiotherapy == |
| | In put from the physiotherapist team may occur in the rehabilitation phase. Rehabilitation interventions may be required to manage complications such as reduced [[Cardiopulmonary Exercise Testing (CPET) In Adults|cardiopulmonary]] function, [[Myopathy Steroid Induced|steroid-induced myopathy]] or [[Post-traumatic arthritis|bone and joint destruction]]Physiotherapy can help client maintain a good quality of life. |
|
| |
|
| ====Loss of Muscle Strength:====
| | Treatment may include: |
| [[File:Grip .jpg|thumb|Hand Grip - Loss of muscle power and muscle mass]]
| |
| * Muscle loss, most frequently a result of disuse, deconditioning, or side effects of immunosuppressive treatment, particularly corticosteroids. This can lead to strength and muscle mass decreases at a rate of about 1% per day.
| |
| * The weight bearing lower extremities and low back extensor muscles are more affected than upper extremities, making it difficult to begin ambulating after prolonged periods of rest.
| |
| * Prolonged immobility and nutrient deficiency, in concert with paraspinal muscle atrophy, can contribute to debilitating back pain.
| |
|
| |
|
| * '''Steroid-induced Myopathy:''' | | * Increasing muscle strength |
| | * Improving [[balance]] |
| | * Increasing flexibility |
| | * Reducing risk of [[Falls and Exercise|falls]] |
| | * Preventing development of muscular and joint contractures |
| | * Providing equipment for mobility eg [[Walking Aids|walking aids]], [[Introduction to Orthotics|orthoses]], callipers and wheelchairs |
| | * Advising on [[Moving and Handling|moving and handling]] techniques and equipment.<ref>Manchester Physio [https://www.manchesterneurophysio.co.uk/adults/conditions-we-treat/orthopaedic-msk-conditions/myopathy/physiotherapy-treatment-for-myopathies.php Myopathies] Available from:https://www.manchesterneurophysio.co.uk/adults/conditions-we-treat/orthopaedic-msk-conditions/myopathy/physiotherapy-treatment-for-myopathies.php (last accessed 22.11.2020)</ref> |
|
| |
|
| * Acute - typically occurs within 1 week of high-dose oral corticosteroid use and can be associated with rhabdomyolysis and pain.
| | ===References=== |
| * Chronic form occurs weeks to months into prolonged, high-dose steroid administration The patients experience general painless muscle weakness in the upper and lower extremities and the neck and usually reports finding it difficult to rise from a seated position.
| |
| | |
| '''Bone:'''
| |
| | |
| As many as 50% of patients who undergo transplant develop osteopenia or osteoporosis and cGVHD is associated with an even higher incidence. This is often the result of chronic glucocorticoid use, a major risk factor for osteopenia and osteoporosis because of increased bone turnover. Other risk factors that these patients face that contribute to bone density loss are:
| |
| [[File:AVN .jpg|thumb|Steroid Induced AVN of Hip]]
| |
| * Calcineurin inhibitor use, chemo and radiation therapy, gonadal dysfunction,
| |
| * Renal dysfunction,
| |
| * Increased marrow turnover due to hematogenous malignancy, and
| |
| * Decreased weight-bearing activity.
| |
| The HSCT itself causes a fundamental alteration of bone mineral metabolism, with loss seen in the first 6 to 12 months. Bone density loss in cGVHD is typically seen more in the femoral heads than the vertebrae, a distinction when compared with menopausal osteoporosis, though the humeral head, knees, and ankles can also be affected.
| |
| | |
| Lastly, patients with osteoporosis can develop hip flexor contractures due to sustained forward-flexed posture. A tight iliopsoas muscle may lead to worsening lumbar lordosis, increasing pain, and adding force being applied to vertebrae already prone to fracture.
| |
| [[File:Myositis .jpg|thumb|Inflammatory Myositis]]
| |
| | |
| ====Inflammatory Myositis:==== | |
| Muscle mass and strength may be compromised because of an inflammatory myositis, mimicking polymyositis or dermatomyositis, that is a direct, immune-mediated result of cGVHD. Associated with tapering of immunosuppressant medications and is associated with the same genetic markers seen in patients with this autoimmune disease who have not undergone transplant. Typically, this presents with painful, symmetric proximal weakness.
| |
| | |
| ====Peripheral Nerves:====
| |
| cGVHD is associated with several possible neurologic sequelae, including mononeuropathies, generalized peripheral neuropathy, and inflammatory neuropathy. A combination of multiple neuropathy. This has also been shown to cause a neuropathic process that resembles acute inflammatory demyelinating polyneuropathy (AIDP), and is thought to be a result of direct infiltration of peripheral nerves by donor T cells.
| |
| | |
| An EMG can be diagnostic and can show demyelination, axon loss, or both. The first electromyographic sign of AIDP is an absent F-response, with subsequent findings of conduction block and denervation.
| |
| | |
| Nerve entrapment can be either by mechanical compression or fascial inflammation. As the inflamed fascia and/or skin surrounding peripheral nerves become fibrosed, the nerve may become entrapped and damaged.
| |
| | |
| Nerves at high risk for entrapment are those with little surrounding tissue, such as the ulnar nerve at the cubital tunnel and peroneal nerve at the fibular head. The median nerve at the carpal tunnel can also be damaged due to wrist flexion contractures.
| |
| | |
| ====Myasthenia Gravis:====
| |
| In rare instances, develops when tapering immunosuppressive medication because of pre-existing autoantibodies against postsynaptic acetylcholine receptors. Most commonly seen in patients who received the HSCT for aplastic anaemia. Symptoms typically are progressive weakness with exertion, with recovery of strength after rest. Ptosis is a common first symptom and its presence along with generalized weakness. May warrant an EMG that includes repetitive stimulation studies and blood tests to detect antibodies to acetylcholine receptors.
| |
| | |
| ==References==
| |
| * Filipovich AH, Weisdorf D, Pavletic S, Socie G, Wingard JR, Lee SJ, Martin P, Chien J, Przepiorka D, Couriel D, Cowen EW. National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. Diagnosis and staging working group report. Biology of blood and marrow transplantation. 2005 Dec 31;11(12):945-56.
| |
| * Baudard M, Vincent A, Moreau P, Kergueris MF, Harousseau JL, Milpied N. Mycophenolate mofetil for the treatment of acute and chronic GVHD is effective and well tolerated but induces a high risk of infectious complications: a series of 21 BM or PBSC transplant patients. Bone marrow transplantation. 2002 Sep 1;30(5):287.
| |
| * Filipovich AH, et al. National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. Diagnosis and staging working group report. Biol Blood Marrow Transplant. 2005;11:945-956.
| |
| * Janin A, et al. Fasciitis in chronic graft-versus-host disease: a clinicopathologic study of 14 cases. Ann Intern Med. 1994;120:993-998.
| |
| * Couriel DR, et al. Chronic graft-versus-host disease manifesting as polymyositis: an uncommon presentation. Bone Marrow Transplant. 2002;30:543-546.
| |
| * Haruki H, et al. Neuropathy in chronic graft-versus-host disease caused by donor T cells. Muscle Nerve. 2012;46:610-611. 39.
| |
| * Rennie JA, Auchterlonie IA. Rheumatological manifestations of the leukaemias and graft versus host disease. Baillière’s Clinical Rheumatol. 1991;5:231-251.
| |
| * Chiodi S, Spinelli S, Ravera G, Petti AR, Van Lint MT, Lamparelli T, Gualandi F, Occhini D, Mordini N, Berisso G, Bregante S. Quality of life in 244 recipients of allogeneic bone marrow transplantation. British journal of haematology. 2000 Sep 1;110(3):614-9.
| |
| * Pallua S, Giesinger J, Oberguggenberger A, Kemmler G, Nachbaur D, Clausen J, Kopp M, Sperner-Unterweger B, Holzner B. Impact of GvHD on quality of life in long-term survivors of haematopoietic transplantation. Bone marrow transplantation. 2010 Oct 1;45(10):1534-9.
| |
| * Wong FL, Francisco L, Togawa K, Kim H, Bosworth A, Atencio L, Hanby C, Grant M, Kandeel F, Forman SJ, Bhatia S. Longitudinal trajectory of sexual functioning after hematopoietic cell transplantation: impact of chronic graft vs. host disease and total body irradiation. Blood. 2013 Jan 1:blood-2013.
| |
| * Thygesen KH, Schjødt I, Jarden M. The impact of hematopoietic stem cell transplantation on sexuality: a systematic review of the literature. Bone marrow transplantation. 2012 May 1;47(5):716-24.
| |
| * Kirchhoff AC, Leisenring W, Syrjala KL. Prospective predictors of return to work in the 5 years after hematopoietic cell transplantation. Journal of Cancer Survivorship. 2010 Mar 1;4(1):33-44.
| |
| * Martires KJ, Baird K, Steinberg SM, Grkovic L, Joe GO, Williams KM, Mitchell SA, Datiles M, Hakim FT, Pavletic SZ, Cowen EW. Sclerotic-type chronic GVHD of the skin: clinical risk factors, laboratory markers, and burden of disease. Blood. 2011 Oct 13;118(15):4250-7.
| |
| * Markusse HM, Dijkmans BA, Fibbe WE. Eosinophilic fasciitis after allogeneic bone marrow transplantation. The Journal of rheumatology. 1990 May;17(5):692-4.
| |
| * Deitrick JE, Whedon GD, Shorr E. Effects of immobilization upon various metabolic and physiologic functions of normal men. Am J Med. 1948;4:3-36.
| |
| * Cuccurullo S. Physical medicine and rehabilitation board review, 2nd ed. New York: Demos; 2010. 53.
| |
| * Gupta A, Gupta Y. Glucocorticoid-induced myopathy: pathophysiology, diagnosis, and treatment. Indian J Endocrinol Metab. 2013;17:913.
| |
| * Stevens AM, Sullivan KM, Nelson JL. Polymyositis as a manifestation of chronic graft-versus-host disease. Rheumatology. 2003;42:34-39.
| |
| * Sullivan KM, et al. Chronic graft-versus-host disease in 52 patients: adverse natural course and successful treatment with combination immunosuppression. Blood. 1981;57:267-276.
| |
| * McClune BL, et al. Screening, prevention and management of osteoporosis and bone loss in adult and pediatric hematopoietic cell transplant recipients. Bone Marrow Transplant. 2011;46:1-9. 49.
| |
| * Schimmer AD, et al. Decreased bone mineral density is common after autologous blood or marrow transplantation. Bone Marrow Transplant. 2001;28:387-391. 50.
| |
| * McClune B, Majhail NS, Flowers ME. Bone loss and avascular necrosis of bone after hematopoietic cell transplantation. Semin Hematol. 2012;49: 59-65.
| |
| * Enright H, Haake R, Weisdorf D. Avascular necrosis of bone: a common serious complication of allogeneic bone marrow transplantation. Am J Med. 1990;89:733-738. 55.
| |
| * McAvoy S, et al. Corticosteroid dose as a risk factor for avascular necrosis of the bone after hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2010;161231-161236.
| |
| * Sean Robinson Smith, Andrew J. Haig, Daniel R. Couriel, Musculoskeletal, Neurologic, and Cardiopulmonary Aspects of Physical Rehabilitatin Patients with Chronic Graft-versus-Host Disease, Biology of Blood and Marrow Transplantation, Volume 21, Issue 5, May 2015, Pages 799-808, ISSN 1083-8791, <nowiki>https://doi.org/10.1016/j.bbmt.2014.10.019</nowiki>.
| |
| [[Category:Autoimmune Disorders]] | | [[Category:Autoimmune Disorders]] |
| | [[Category:Conditions]] |