Internal disc disruption: Difference between revisions
(Updated peer review via STOPS) |
Kim Jackson (talk | contribs) No edit summary |
||
| (20 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Alexander Chan |Alexander Chan ]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | |||
'''Original | <div class="editorbox"> | ||
</div> | </div> | ||
== | == Introduction == | ||
[[File:Internal disc disruption.png|alt=|thumb|IDD with radial fissure, no change in annulus from outer surface]] | |||
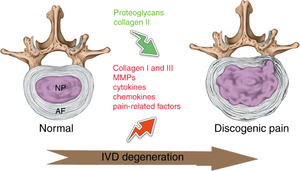
Internal disc disruption (IDD) is a common cause of disabling low back pain (LBP) in young, healthy adults. Internal disc disruption is a distortion of the nucleus pulposus, with annular fissures, without developing [[Disc Herniation|disc herniation]].<ref name="p6" /> | |||
# The radial fissure extend from the nucleus to annulus causing annular tearing and irritation of the free nerve endings | |||
# If it reaches the outer third of the annulus fibrosis, the radial fissure stimulate chemical and mechanoreceptors causing pain<ref name=":0">Simon J, McAuliffe M, Shamim F, Vuong N, Tahaei A. Discogenic low back pain. Physical Medicine and Rehabilitation Clinics. 2014 May 1;25(2):305-17.</ref>. | |||
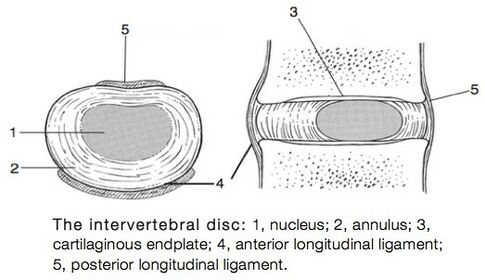
'''Clinically Relevant Anatomy:''' Click on the link for more specific details about [http://www.physio-pedia.com/index.php/Intervertebral_disc intervertebral disc] and [[Biomechanics of Lumbar Intervertebral Disc Herniation]] | |||
Click on the link for more specific details about [http://www.physio-pedia.com/index.php/Intervertebral_disc intervertebral disc] | |||
== Epidemiology /Etiology == | == Epidemiology /Etiology == | ||
[[File:Allan foto4.jpg|right|frameless|485x485px]] | |||
Internal disc disruption is a subgroup of [[Lumbar Discogenic Pain|discogenic pain]]. | |||
Repetitive shearing, axial load, and disc compression is believed to be related to the development of fissure, this leads to vertebral endplate fracture where the fissures can develop containing nuclear material of the degraded disc. This could initiate an autoimmune response.<ref name="p2">Crock, H.V., A reappraisal of intervertebral disc lesions. Med J Aust, 1970. 1(20): p. 983-9.</ref> | |||
The prevalence of IDD has been estimated to be 39% (95% CI: 29% to 49%) in ninety-two patients with chronic LBP.<ref name=" | The prevalence of IDD has been estimated to be 39% (95% CI: 29% to 49%) in ninety-two patients with chronic LBP.<ref name="p3">Schwarzer, A.C., et al., The prevalence and clinical features of internal disc disruption in patients with chronic low back pain. Spine (Phila Pa 1976), 1995. 20(17): p. 1878-83.</ref> In a more recent study, it has been estimated at 42% (95% confidence interval [CI] = 35% to 49%).<ref name="p4">DePalma, M.J., J.M. Ketchum, and T. Saullo, What is the source of chronic low back pain and does age play a role? Pain Med, 2011. 12(2): p. 224-33.</ref> | ||
< | == Classification of IDD == | ||
{| class="wikitable" | |||
!Grades | |||
!Description<ref>https://freinlazzara.medicalillustration.com/generateexhibit.php?ID=3102&ExhibitKeywordsRaw=&TL=&A=</ref> | |||
|- | |||
|grade 1 | |||
|Early annular tear extends to the inner third of the disc | |||
|- | |||
|grade 2 | |||
|More annular tear extends to middle third | |||
|- | |||
|grade 3 | |||
|The tear extends to the outer third of the disc | |||
|- | |||
|grade 4 | |||
|The same as grade 3 + circumferential spread in the outer third | |||
|} | |||
This classification according to the modified Dallas Discograme Scale. Where Grade 0 is the normal disc. Often grade 1, 2 don't associate with pain, and grade 3, 4 presented with pain. <ref>Aprill C, Bogduk N. High-intensity zone: a diagnostic sign of painful lumbar disc on magnetic resonance imaging. The British journal of radiology. 1992 May;65(773):361-9.</ref><ref>Vanharanta H, Sachs BL, Spivey MA, Guyer RD, Hochschuler SH, Rashbaum RF, Johnson RG, Ohnmeiss D, Mooney V. The relationship of pain provocation to lumbar disc deterioration as seen by CT/discography. Spine. 1987 Apr;12(3):295-8.</ref> | |||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
The ideal patient symptoms will present with central low back pain without radiation or minimal radiation to one or both limbs describe the pain as it's deep dull aching pain decreases with extension or lying flat. Sitting, driving, twisting, flexion, coughing, and [[Valsalva Test|Valsalva]] test aggravate symptoms<ref name=":0" />. | |||
'''In the IASP’s Classification of Chronic Pain, IDD has the features of:''' | |||
*< | *Lumbar spinal pain, with or without referred pain in the lower limb girdle or lower limb; | ||
</ | *Aggravated by movements that stress the symptomatic disk<ref name="p1">IASP Taxonomy Working Group, Classification of Chronic Pain: Descriptions of Chronic Pain Syndromes and Definitions of Pain Terms, 2011.</ref> | ||
'''According to Sehgal (2000), most of the patient’s experience:''' | |||
*Diffuse, dull ache | |||
* | |||
*a deep-seated, burning, lancinating pain in the back | *a deep-seated, burning, lancinating pain in the back | ||
* | *Sensation of a weak, unstable back | ||
* | *Referral of pain into the hips and lower limbs is not uncommon. | ||
*a varying degree of sitting intolerance | *a varying degree of sitting intolerance | ||
* | *Lumbar spine movements are slow, guarded and restricted | ||
* | *History of lifting trauma precedes the back pain in acute cases | ||
* | *Pain and muscle spasm are less dramatic and more nondescript in persistent cases<ref name="p6">Sehgal, N. and J.D. Fortin, Internal disc disruption and low back pain. Pain Physician, 2000. 3(2): p. 143-157</ref> | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
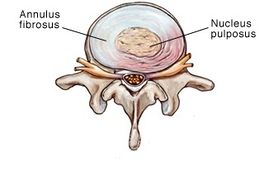
[[File:Annular-bulge-disc-rev.jpg|thumb|269x269px|Grade 1 disc herniation]] | |||
* [http://www.physio-pedia.com/index.php/Disc_Herniaton '''Disc herniation'''] | |||
* '''Ruptured disc''' | |||
* [http://www.physio-pedia.com/Degenerative_Disc_Disease '''Degenerative disc disease''']:<br> | |||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
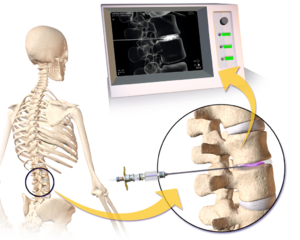
[[File:Discography.png|thumb|Lumbar Discography]] | |||
Physical examination alone is insufficient to establish a diagnosis of IDD. Diagnostic imaging, however, has contributed to the understanding of IDD. The only convincing means to establish the diagnosis is provocation discography. Despite the clinical use of discography, its utility has been questioned due to high false positive rates.<ref name="p2" /><ref name="p4" /><ref name="p5">Crock, H., Internal disc disruption: A challange to disc prolapse fifty years on. Spine (Phila Pa 1976), 1986. 11(6): p. 650-3.</ref> It is also associated with procedural risks, is expensive, and can be difficult to access.<ref name="p6" /> Discography has also been shown to result in accelerated disc degeneration compared to match-controls.<ref name="p7">Fernstrom, U., A discographical study of ruptured lumbar intervertebral discs. Acta Chir Scand Suppl, 1960. Suppl 258: p. 1-60.</ref> | |||
* Provocative discography '''the''' '''gold standard''' for the diagnosis of [[Lumbar Discogenic Pain|lumbar discogenic pain]] it is a physiologic test that explicitly determines whether a disc is painful. The disc suspected of causing pain is injected with radiolucent dye. The aim is to provoke clinical symptoms and reveal morphological abnormalities in the annulus fibrosis.<ref name="p2" />The test is considered positive if the individual’s concordant pain is reproduced upon stimulating the suspected painful disc, and injection of adjacent discs does not reproduce the typical symptoms.<ref name="p3" /> In asymptomatic individuals, discography is not painful, but is frequently painful in those with low back pain. A post-discography CT scan can be used to evaluate the extent of internal disruption within the disc. | |||
'''The criteria for diagnosing IDD from the International Association for the Study of Pain’s Taxonomy Working Group is:''' | |||
# Lumbar spinal pain, with or without referred pain in the lower limb girdle or lower limb | |||
# Aggravated by movements that stress the symptomatic disc | |||
# MRI or CT don't show a visible disc herniation | |||
# Injection of the disc above or below the suspected disc mustn't elicit pain | |||
# Diagnostic criteria for [[Lumbar Discogenic Pain|lumbar discogenic pain]] must be satisfied including either: <br> 1. Selective anesthetization of the putatively symptomatic intervertebral disc completely relieves accustomed pain, or save that whatever pain persists can be ascribed to some other coexisting source or cause<br> 2. Provocative discography of the putatively symptomatic disc reproduces the patient’s accustomed pain, but not at least two adjacent discs, and the pain cannot be ascribed to some other source innervated by the same segments as the symptomatic disc | |||
6. CT-discography must demonstrate a grade 3 or greater grade of annular disruption | |||
== Outcome Measures == | == Outcome Measures == | ||
[[Visual Analogue Scale|Visual Analogue scale VAS]] | |||
== Examination == | == Examination == | ||
It is very difficult to establish a clinical diagnosis only based on history and physical examination when there are no objective clinical findings. There is no clinical test that can make a distinction between IDD patients and patients with other conditions.<ref name=" | It is very difficult to establish a clinical diagnosis only based on history and physical examination when there are no objective clinical findings. There is no clinical test that can make a distinction between IDD patients and patients with other conditions.<ref name="p3" /> The only convincing means to establish IDD is provocative discography as described above. | ||
== Medical Management == | |||
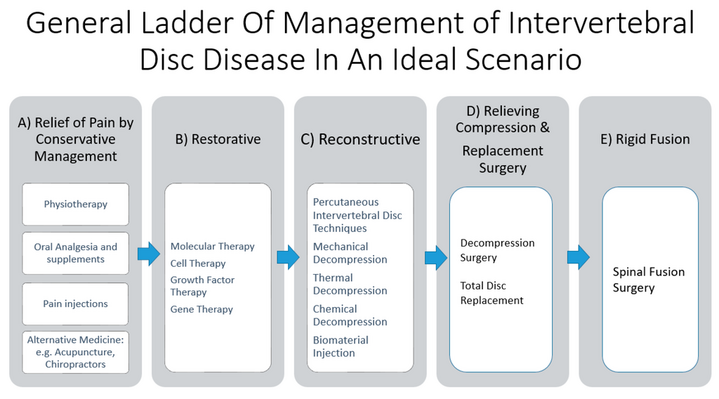
Most causes will respond to conservative treatment of medication, relative rest, and physical therapy intervention<ref name=":1" /> General ladder of management: | |||
<br> | # Pharmacological management: Analgesic purposesand may include the use of Acetaminophen (Paracetamol), non-steroidal anti-inflammatories, muscle relaxants, or opioids.<ref name="p8">Roberts, S., et al., Histology and pathology of the human intervertebral disc. J Bone Joint Surg Am, 2006. 88 Suppl 2(Supplement 2): p. 10-4.</ref> | ||
# Minimally invasive interventional procedures: Intradiscal steroid injection; Radiofrequency denervation; Intradiscal Electrothermal (IDET) Therapy | |||
# Surgical treatment: Internal disc disruption can be managed surgically by fusing the vertebrae at the level of disc disruption.<br>Disadvantages of surgical fusion include:<br> - Failure to maintain the height of the intervertebral disc<br> - Less segmental motion at the fused levels, which may contribute cephalocaudal neuro foraminal stenosis and overloading of adjacent disc levels <ref name="p6" /> | |||
< | Most causes will respond to conservative treatment of medication, relative rest, and physical therapy intervention<ref name=":1">Raj PP. Intervertebral disc: anatomy‐physiology‐pathophysiology‐treatment. Pain Practice. 2008 Jan;8(1):18-44.</ref> | ||
[[File:General ladder of management of intervertebral disc disease in an ideal scenario.png|center|frameless|719x719px]] | |||
== Physical Therapy Management | == Physical Therapy Management == | ||
The main goals of treatment are improving function and quality of life, treat pain and in long term, prevent future back injury and disability. | The main goals of treatment are improving function and [[Quality of Life|quality of life]], treat pain and in long term, prevent future back injury and [[Disability-Adjusted Life Year|disability]]. | ||
<br> | 1) [[Core Stability|Dynamic lumbar stabilisation]]:<br>Traditionally core stability has referred to the active component to the stabilizing system. This includes local muscles that provide segmental stability (eg [[Transversus Abdominis|transversus abdominis]], [[lumbar Multifidus]]) and/or the global muscles (eg [[Rectus Abdominis|rectus abdominis]], [[Erector Spinae|erector spinae]]) that enable trunk movement/torque generation and assistance in the stability in more physically demanding tasks.<ref name="p9">Bogduk, N., Clinical anatomy of the lumbar spine and sacrum. 4th ed. 2005, New York: Churchill Livingstone.</ref> | ||
2) Mechanical Diagnosis and Therapy ([[McKenzie Method|McKenzie Method]]) <ref name="p0">Milette, P., et al., Differentiating lumbar disc protrusions, disc bulges, and disc with normal contour but abnormal signal intensity. Magnetic resonance imaging with discographic correlations. Spine, 1999. 24(1): p. 44-53.</ref>:<br>The McKenzie method utilizes the patient’s response to repeated lumbar movements to assess which movements reduce the individual’s most peripheral symptoms. These movements are then combined into an individualized exercise regimen. | |||
2) Mechanical Diagnosis and Therapy (McKenzie Method) <ref name=" | |||
== References == | == References == | ||
| Line 146: | Line 108: | ||
[[Category:Vrije_Universiteit_Brussel_Project]] | [[Category:Vrije_Universiteit_Brussel_Project]] | ||
[[Category:Lumbar Spine - Conditions]] | |||
[[Category:Musculoskeletal/Orthopaedics]] | |||
Latest revision as of 12:12, 1 December 2022
Introduction[edit | edit source]
Internal disc disruption (IDD) is a common cause of disabling low back pain (LBP) in young, healthy adults. Internal disc disruption is a distortion of the nucleus pulposus, with annular fissures, without developing disc herniation.[1]
- The radial fissure extend from the nucleus to annulus causing annular tearing and irritation of the free nerve endings
- If it reaches the outer third of the annulus fibrosis, the radial fissure stimulate chemical and mechanoreceptors causing pain[2].
Clinically Relevant Anatomy: Click on the link for more specific details about intervertebral disc and Biomechanics of Lumbar Intervertebral Disc Herniation
Epidemiology /Etiology[edit | edit source]
Internal disc disruption is a subgroup of discogenic pain.
Repetitive shearing, axial load, and disc compression is believed to be related to the development of fissure, this leads to vertebral endplate fracture where the fissures can develop containing nuclear material of the degraded disc. This could initiate an autoimmune response.[3]
The prevalence of IDD has been estimated to be 39% (95% CI: 29% to 49%) in ninety-two patients with chronic LBP.[4] In a more recent study, it has been estimated at 42% (95% confidence interval [CI] = 35% to 49%).[5]
Classification of IDD[edit | edit source]
| Grades | Description[6] |
|---|---|
| grade 1 | Early annular tear extends to the inner third of the disc |
| grade 2 | More annular tear extends to middle third |
| grade 3 | The tear extends to the outer third of the disc |
| grade 4 | The same as grade 3 + circumferential spread in the outer third |
This classification according to the modified Dallas Discograme Scale. Where Grade 0 is the normal disc. Often grade 1, 2 don't associate with pain, and grade 3, 4 presented with pain. [7][8]
Characteristics/Clinical Presentation[edit | edit source]
The ideal patient symptoms will present with central low back pain without radiation or minimal radiation to one or both limbs describe the pain as it's deep dull aching pain decreases with extension or lying flat. Sitting, driving, twisting, flexion, coughing, and Valsalva test aggravate symptoms[2].
In the IASP’s Classification of Chronic Pain, IDD has the features of:
- Lumbar spinal pain, with or without referred pain in the lower limb girdle or lower limb;
- Aggravated by movements that stress the symptomatic disk[9]
According to Sehgal (2000), most of the patient’s experience:
- Diffuse, dull ache
- a deep-seated, burning, lancinating pain in the back
- Sensation of a weak, unstable back
- Referral of pain into the hips and lower limbs is not uncommon.
- a varying degree of sitting intolerance
- Lumbar spine movements are slow, guarded and restricted
- History of lifting trauma precedes the back pain in acute cases
- Pain and muscle spasm are less dramatic and more nondescript in persistent cases[1]
Differential Diagnosis[edit | edit source]
- Disc herniation
- Ruptured disc
- Degenerative disc disease:
Diagnostic Procedures[edit | edit source]
Physical examination alone is insufficient to establish a diagnosis of IDD. Diagnostic imaging, however, has contributed to the understanding of IDD. The only convincing means to establish the diagnosis is provocation discography. Despite the clinical use of discography, its utility has been questioned due to high false positive rates.[3][5][10] It is also associated with procedural risks, is expensive, and can be difficult to access.[1] Discography has also been shown to result in accelerated disc degeneration compared to match-controls.[11]
- Provocative discography the gold standard for the diagnosis of lumbar discogenic pain it is a physiologic test that explicitly determines whether a disc is painful. The disc suspected of causing pain is injected with radiolucent dye. The aim is to provoke clinical symptoms and reveal morphological abnormalities in the annulus fibrosis.[3]The test is considered positive if the individual’s concordant pain is reproduced upon stimulating the suspected painful disc, and injection of adjacent discs does not reproduce the typical symptoms.[4] In asymptomatic individuals, discography is not painful, but is frequently painful in those with low back pain. A post-discography CT scan can be used to evaluate the extent of internal disruption within the disc.
The criteria for diagnosing IDD from the International Association for the Study of Pain’s Taxonomy Working Group is:
- Lumbar spinal pain, with or without referred pain in the lower limb girdle or lower limb
- Aggravated by movements that stress the symptomatic disc
- MRI or CT don't show a visible disc herniation
- Injection of the disc above or below the suspected disc mustn't elicit pain
- Diagnostic criteria for lumbar discogenic pain must be satisfied including either:
1. Selective anesthetization of the putatively symptomatic intervertebral disc completely relieves accustomed pain, or save that whatever pain persists can be ascribed to some other coexisting source or cause
2. Provocative discography of the putatively symptomatic disc reproduces the patient’s accustomed pain, but not at least two adjacent discs, and the pain cannot be ascribed to some other source innervated by the same segments as the symptomatic disc
6. CT-discography must demonstrate a grade 3 or greater grade of annular disruption
Outcome Measures[edit | edit source]
Examination[edit | edit source]
It is very difficult to establish a clinical diagnosis only based on history and physical examination when there are no objective clinical findings. There is no clinical test that can make a distinction between IDD patients and patients with other conditions.[4] The only convincing means to establish IDD is provocative discography as described above.
Medical Management[edit | edit source]
Most causes will respond to conservative treatment of medication, relative rest, and physical therapy intervention[12] General ladder of management:
- Pharmacological management: Analgesic purposesand may include the use of Acetaminophen (Paracetamol), non-steroidal anti-inflammatories, muscle relaxants, or opioids.[13]
- Minimally invasive interventional procedures: Intradiscal steroid injection; Radiofrequency denervation; Intradiscal Electrothermal (IDET) Therapy
- Surgical treatment: Internal disc disruption can be managed surgically by fusing the vertebrae at the level of disc disruption.
Disadvantages of surgical fusion include:
- Failure to maintain the height of the intervertebral disc
- Less segmental motion at the fused levels, which may contribute cephalocaudal neuro foraminal stenosis and overloading of adjacent disc levels [1]
Most causes will respond to conservative treatment of medication, relative rest, and physical therapy intervention[12]
Physical Therapy Management[edit | edit source]
The main goals of treatment are improving function and quality of life, treat pain and in long term, prevent future back injury and disability.
1) Dynamic lumbar stabilisation:
Traditionally core stability has referred to the active component to the stabilizing system. This includes local muscles that provide segmental stability (eg transversus abdominis, lumbar Multifidus) and/or the global muscles (eg rectus abdominis, erector spinae) that enable trunk movement/torque generation and assistance in the stability in more physically demanding tasks.[14]
2) Mechanical Diagnosis and Therapy (McKenzie Method) [15]:
The McKenzie method utilizes the patient’s response to repeated lumbar movements to assess which movements reduce the individual’s most peripheral symptoms. These movements are then combined into an individualized exercise regimen.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Sehgal, N. and J.D. Fortin, Internal disc disruption and low back pain. Pain Physician, 2000. 3(2): p. 143-157
- ↑ 2.0 2.1 Simon J, McAuliffe M, Shamim F, Vuong N, Tahaei A. Discogenic low back pain. Physical Medicine and Rehabilitation Clinics. 2014 May 1;25(2):305-17.
- ↑ 3.0 3.1 3.2 Crock, H.V., A reappraisal of intervertebral disc lesions. Med J Aust, 1970. 1(20): p. 983-9.
- ↑ 4.0 4.1 4.2 Schwarzer, A.C., et al., The prevalence and clinical features of internal disc disruption in patients with chronic low back pain. Spine (Phila Pa 1976), 1995. 20(17): p. 1878-83.
- ↑ 5.0 5.1 DePalma, M.J., J.M. Ketchum, and T. Saullo, What is the source of chronic low back pain and does age play a role? Pain Med, 2011. 12(2): p. 224-33.
- ↑ https://freinlazzara.medicalillustration.com/generateexhibit.php?ID=3102&ExhibitKeywordsRaw=&TL=&A=
- ↑ Aprill C, Bogduk N. High-intensity zone: a diagnostic sign of painful lumbar disc on magnetic resonance imaging. The British journal of radiology. 1992 May;65(773):361-9.
- ↑ Vanharanta H, Sachs BL, Spivey MA, Guyer RD, Hochschuler SH, Rashbaum RF, Johnson RG, Ohnmeiss D, Mooney V. The relationship of pain provocation to lumbar disc deterioration as seen by CT/discography. Spine. 1987 Apr;12(3):295-8.
- ↑ IASP Taxonomy Working Group, Classification of Chronic Pain: Descriptions of Chronic Pain Syndromes and Definitions of Pain Terms, 2011.
- ↑ Crock, H., Internal disc disruption: A challange to disc prolapse fifty years on. Spine (Phila Pa 1976), 1986. 11(6): p. 650-3.
- ↑ Fernstrom, U., A discographical study of ruptured lumbar intervertebral discs. Acta Chir Scand Suppl, 1960. Suppl 258: p. 1-60.
- ↑ 12.0 12.1 Raj PP. Intervertebral disc: anatomy‐physiology‐pathophysiology‐treatment. Pain Practice. 2008 Jan;8(1):18-44.
- ↑ Roberts, S., et al., Histology and pathology of the human intervertebral disc. J Bone Joint Surg Am, 2006. 88 Suppl 2(Supplement 2): p. 10-4.
- ↑ Bogduk, N., Clinical anatomy of the lumbar spine and sacrum. 4th ed. 2005, New York: Churchill Livingstone.
- ↑ Milette, P., et al., Differentiating lumbar disc protrusions, disc bulges, and disc with normal contour but abnormal signal intensity. Magnetic resonance imaging with discographic correlations. Spine, 1999. 24(1): p. 44-53.