Lumbosacral Discogenic Pain Syndrome: Difference between revisions
No edit summary |
No edit summary |
||
| (16 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editors ''' - [[User:Sam Verhelpen|Sam Verhelpen]] | '''Original Editors ''' - [[User:Sam Verhelpen|Sam Verhelpen]] | ||
''' | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | |||
== Introduction == | |||
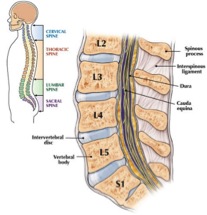
[[File:Spine anatomy.jpg|thumb|Lumbosacral spine]] | |||
Lumbosacral discogenic pain syndrome (LSPS) is a common cause of low back pain which can come from various structures, notably facet joints, spinal muscles, and ligaments. [[Low Back Pain|Low back pain]] is a major clinical and socioeconomic burden in the global health sector | |||
= | This page focuses on the pathophysiology, evaluation, and treatment of LSPS and pain arising from pathology involving the intervertebral disc.<ref name=":0">Pathak S, Conermann T. Lumbosacral discogenic syndrome. 2020 Available:https://www.ncbi.nlm.nih.gov/books/NBK560537/ (accessed 27.11.2022)</ref> | ||
== Relevant Anatomical Structures == | |||
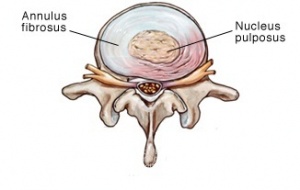
[[File:Annular-bulge-disc-rev.jpg|thumb|Annular IV disc bulge]] | |||
The [[intervertebral disc]] is found between two vertebrae and consist of a semifluid nucleus pulposus with an annulus fibrosus surrounding it. The nucleus consist of 70-80% water but this decreases as people get older.<ref name="one">Windsor R. Lumbosacral Discogenic Pain Syndrome. 2010 http://emedicine.medscape.com/article/94673-overview#a0106 Level of evidence: D</ref> The annulus consists of 10-20 concentric fibrous rings, with fibers of alternating orientation. | |||
= | The main function of the intervertebral disc is to allow movement between two vertebrae and to transmit loads from one vertebral to the next.<ref name="one" /> | ||
== Etiology == | |||
[[File:Truck driver risk factor for LSPS.jpeg|thumb|Truck driver risk factor for LSPS]] | |||
Strong familial predisposition to LSPS | |||
[[Degenerative Disc Disease|Degenerative disk disease]] is associated with advanced age, male sex, and smoking | |||
Linked with particular occupations: (see also [[Biomechanics of Lumbar Intervertebral Disc Herniation]]) | |||
* Sitting positions and vibratory forces may expose discs to stresses, promoting LSPS (truck drivers, manual laborers). Intradiscal pressures increase during sitting. | |||
* Physically strenuous activities and repetitive motion possibly contribute to disc degeneration and favour annular injury.<ref>Singh AD, Pechman K, Zar S. Discogenic Lumbar Pain. Available: https://now.aapmr.org/discogenic-lumbar-pain/<nowiki/>(accessed 27.11.2022)</ref> | |||
== Epidemiology == | |||
Lumbar disc disease is a very common with a high asymptomatic prevalence. | |||
Intervertebral disc anomolies are found in 25% of individuals below the age of 60, and over 50% in those over the age of 60. A disc lesion in someone with non-specific back pain is not therefore necessarily the cause of the pain. Correlation with clinical presentation (e.g. myotomal weakness and dermatomal numbness), along side, with interventional spinal procedures (e.g. spinal epidural injection, facet joint injection, transforaminal injection) is necessary to confirm that a particular disc lesion is causative.<ref>Radiopedia Lumbar disc disease Available:https://radiopaedia.org/articles/lumbar-disc-disease (accessed 27.11.2022)</ref> | |||
== | == Examination == | ||
'''History''' | |||
Discogenic low back pain typically increases when sitting, flexing the back, coughing, sneezing. In general, activities that increase intradiscal pressure.<ref name="one" / | Discogenic low back pain typically increases when sitting, flexing the back, coughing, sneezing. In general, activities that increase intradiscal pressure.<ref name="one" /> | ||
'''Physical Examination''' | |||
There is no typical examination to determine discogenic pain. Some consider biphasic straightening from flexion an indication of problems with the discus.<ref name="two" /> Pain from pressure on the | There is no typical examination to determine discogenic pain. Some consider biphasic straightening from flexion an indication of problems with the discus.<ref name="two">Kallewaard JW, et al. 15. Discogenic low back pain. Pain Practice, Volume 10, Issue 6, 2010 560–579. Level of evidence: A1</ref> Pain from pressure on the spinous is considered an indication for discogenic low back pain.<ref name="two" /> Although these examinations give an indication, they have not been validated and additional examination is needed to determine discogenic low back pain, such as MRI and CT.<ref name="one" /><ref name="two" /><ref name="three">Ohtori S, et al. Surgical Versus Nonsurgical Treatment of Selected Patients With Discogenic Low Back Pain. SPINE Volume 36, Number 5, pp 347–354 Level of evidence: A2</ref> | ||
Another possible test is a lumbar overpressure test. The patient sits on the table, with his back to the therapist. The therapist pushes downwards on the patient’s shoulders. If this provokes pain, the test is considered positive. The patient can also make a rounded back to provoke the anterior part of the disc, and a hollow back to provoke the posterior part of the disc. | Another possible test is a lumbar overpressure test. The patient sits on the table, with his back to the therapist. The therapist pushes downwards on the patient’s shoulders. If this provokes pain, the test is considered positive. The patient can also make a rounded back to provoke the anterior part of the disc, and a hollow back to provoke the posterior part of the disc. | ||
== Differential | == Differential Diagnosis == | ||
As LSPS is axial, other causes of axial back pain need be considered including | |||
* Lumbosacral [[Facet Joint Syndrome]] <ref name="one" /> | |||
*[[Lumbar Radiculopathy|Lumbosacral Radiculopathy]] <ref name="one" /> | |||
* Lumbosacral [[Spondylolisthesis]] <ref name="one" /> | |||
*[[Lumbar Spondylosis|Lumbosacral Spondylolysis]] <ref name="one" /> | |||
* [[Paraspinal Muscles|Paraspinal Muscle]] sprain or strain, ligament sprain or strain.<ref name=":0" /> | |||
Therefore a detailed history and careful physical exam, along with pertinent imaging, can help to make the correct diagnosis. | |||
== Physical Therapy Management == | |||
[[File:Back stretch exercise adherence.jpg|thumb|Back stretch exercise]] | |||
Acute or subacute disc injuries should initially be treated conservatively. This includes physiotherapy, and the emphasis should be to reduce muscular guarding, improve segmental motion, improve mechanical faults and improve the function of the patient with a home exercise program.<ref name="one" /> <br>Later, the patient can start with a [[Exercises for Lumbar Instability|lumbar stabilization program.]] <ref name="one" /> | |||
For a more detailed outline of PT see [[Lumbar Discogenic Pain]] | |||
== | * Kallewaard JW, et al. mention there being a systematic review claiming no evidence of any added value of active exercise therapy in relation to bed rest and other conservative treatments such as traction manipulation, hot packs or corsets.<ref name="two" /> | ||
* Ohtori S, et al. found that patients who received surgery scored significantly lower on pain scales than patients who were treated conservatively at the two-year follow-up.<ref name="three" /> | |||
* Bronfort G, et al found moderate evidence that spinal manipulation (SM) is more effective than normal mobilisations (MOB) in acute low back pain. In chronic low back pain SM and MOB had a short term effect similar to NSAID’s.<ref name="four">Bronfort G, et al. Efficacy of spinal manipulation and mobilization for low back pain and neck pain: a systematic review and best evidence synthesis. The Spine Journal 4 (2004) 335–356 Level of evidence: A1</ref> | |||
== Clinical Bottom Line == | |||
With conflicting evidence for several treatment methods, it’s clear there is no one true treatment method and the therapist should see which kind of therapy the patient responds to best. | |||
== References == | |||
== References | |||
<references /> | <references /> | ||
| Line 61: | Line 71: | ||
<br> <br><br> | <br> <br><br> | ||
[[Category:Lumbar]] | [[Category:Lumbar Spine]] | ||
[[Category:Lumbar Spine - Conditions]] | |||
[[Category:Conditions]] | |||
[[Category:Pain]] | |||
Latest revision as of 03:02, 27 November 2022
Original Editors - Sam Verhelpen
Top Contributors - Admin, Kim Jackson, Lucinda hampton, Sam Verhelpen, Oyemi Sillo and WikiSysop
Introduction[edit | edit source]
Lumbosacral discogenic pain syndrome (LSPS) is a common cause of low back pain which can come from various structures, notably facet joints, spinal muscles, and ligaments. Low back pain is a major clinical and socioeconomic burden in the global health sector
This page focuses on the pathophysiology, evaluation, and treatment of LSPS and pain arising from pathology involving the intervertebral disc.[1]
Relevant Anatomical Structures[edit | edit source]
The intervertebral disc is found between two vertebrae and consist of a semifluid nucleus pulposus with an annulus fibrosus surrounding it. The nucleus consist of 70-80% water but this decreases as people get older.[2] The annulus consists of 10-20 concentric fibrous rings, with fibers of alternating orientation.
The main function of the intervertebral disc is to allow movement between two vertebrae and to transmit loads from one vertebral to the next.[2]
Etiology[edit | edit source]
Strong familial predisposition to LSPS
Degenerative disk disease is associated with advanced age, male sex, and smoking
Linked with particular occupations: (see also Biomechanics of Lumbar Intervertebral Disc Herniation)
- Sitting positions and vibratory forces may expose discs to stresses, promoting LSPS (truck drivers, manual laborers). Intradiscal pressures increase during sitting.
- Physically strenuous activities and repetitive motion possibly contribute to disc degeneration and favour annular injury.[3]
Epidemiology[edit | edit source]
Lumbar disc disease is a very common with a high asymptomatic prevalence.
Intervertebral disc anomolies are found in 25% of individuals below the age of 60, and over 50% in those over the age of 60. A disc lesion in someone with non-specific back pain is not therefore necessarily the cause of the pain. Correlation with clinical presentation (e.g. myotomal weakness and dermatomal numbness), along side, with interventional spinal procedures (e.g. spinal epidural injection, facet joint injection, transforaminal injection) is necessary to confirm that a particular disc lesion is causative.[4]
Examination[edit | edit source]
History
Discogenic low back pain typically increases when sitting, flexing the back, coughing, sneezing. In general, activities that increase intradiscal pressure.[2]
Physical Examination
There is no typical examination to determine discogenic pain. Some consider biphasic straightening from flexion an indication of problems with the discus.[5] Pain from pressure on the spinous is considered an indication for discogenic low back pain.[5] Although these examinations give an indication, they have not been validated and additional examination is needed to determine discogenic low back pain, such as MRI and CT.[2][5][6]
Another possible test is a lumbar overpressure test. The patient sits on the table, with his back to the therapist. The therapist pushes downwards on the patient’s shoulders. If this provokes pain, the test is considered positive. The patient can also make a rounded back to provoke the anterior part of the disc, and a hollow back to provoke the posterior part of the disc.
Differential Diagnosis[edit | edit source]
As LSPS is axial, other causes of axial back pain need be considered including
- Lumbosacral Facet Joint Syndrome [2]
- Lumbosacral Radiculopathy [2]
- Lumbosacral Spondylolisthesis [2]
- Lumbosacral Spondylolysis [2]
- Paraspinal Muscle sprain or strain, ligament sprain or strain.[1]
Therefore a detailed history and careful physical exam, along with pertinent imaging, can help to make the correct diagnosis.
Physical Therapy Management[edit | edit source]
Acute or subacute disc injuries should initially be treated conservatively. This includes physiotherapy, and the emphasis should be to reduce muscular guarding, improve segmental motion, improve mechanical faults and improve the function of the patient with a home exercise program.[2]
Later, the patient can start with a lumbar stabilization program. [2]
For a more detailed outline of PT see Lumbar Discogenic Pain
- Kallewaard JW, et al. mention there being a systematic review claiming no evidence of any added value of active exercise therapy in relation to bed rest and other conservative treatments such as traction manipulation, hot packs or corsets.[5]
- Ohtori S, et al. found that patients who received surgery scored significantly lower on pain scales than patients who were treated conservatively at the two-year follow-up.[6]
- Bronfort G, et al found moderate evidence that spinal manipulation (SM) is more effective than normal mobilisations (MOB) in acute low back pain. In chronic low back pain SM and MOB had a short term effect similar to NSAID’s.[7]
Clinical Bottom Line[edit | edit source]
With conflicting evidence for several treatment methods, it’s clear there is no one true treatment method and the therapist should see which kind of therapy the patient responds to best.
References[edit | edit source]
- ↑ 1.0 1.1 Pathak S, Conermann T. Lumbosacral discogenic syndrome. 2020 Available:https://www.ncbi.nlm.nih.gov/books/NBK560537/ (accessed 27.11.2022)
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 2.9 Windsor R. Lumbosacral Discogenic Pain Syndrome. 2010 http://emedicine.medscape.com/article/94673-overview#a0106 Level of evidence: D
- ↑ Singh AD, Pechman K, Zar S. Discogenic Lumbar Pain. Available: https://now.aapmr.org/discogenic-lumbar-pain/(accessed 27.11.2022)
- ↑ Radiopedia Lumbar disc disease Available:https://radiopaedia.org/articles/lumbar-disc-disease (accessed 27.11.2022)
- ↑ 5.0 5.1 5.2 5.3 Kallewaard JW, et al. 15. Discogenic low back pain. Pain Practice, Volume 10, Issue 6, 2010 560–579. Level of evidence: A1
- ↑ 6.0 6.1 Ohtori S, et al. Surgical Versus Nonsurgical Treatment of Selected Patients With Discogenic Low Back Pain. SPINE Volume 36, Number 5, pp 347–354 Level of evidence: A2
- ↑ Bronfort G, et al. Efficacy of spinal manipulation and mobilization for low back pain and neck pain: a systematic review and best evidence synthesis. The Spine Journal 4 (2004) 335–356 Level of evidence: A1