Fahr's Syndrome: Difference between revisions
Logan Wood (talk | contribs) mNo edit summary |
Kim Jackson (talk | contribs) No edit summary |
||
| (38 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- [ | '''Original Editor '''- [[User:Sarah_Dorsey|Sarah Dorsey]], [[User:Maria_Tyumkin|Maria Tyumkin]], [[User:Megan_Willerth|Megan Willerth]], [[User:Jennifer_Withers|Jennifer Withers]], [[User:Logan_Wood|Logan Wood]] as part of the [[Queen's University Neuromotor Function Project]]<br> | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | |||
== Introduction == | |||
[[File:Basal Ganglia and Related Structures.svg.png|400px|thumb|Fig. 1 Basal Ganglia and Related Structures <ref>John Henkel. Structure of the basal ganglia, including thalamus, globus paladus, substantia nigra, and cerebellum [image on the Internet]. Food and Drug Administration, 23 March 2009, 17:14 (UTC). Available from: https://commons.wikimedia.org/wiki/File:Basal_Ganglia_and_Related_Structures.svg</ref>]] | |||
Fahr’s syndrome is also known as Fahr’s disease, familial idiopathic basal ganglia calcification and primary familial brain calcification. It is a rare neurological disorder characterized by bilateral calcifications of areas in the brain including<ref name=":1">National Institute of Neurological Disorder and Stroke. Fahr’s Syndrome Information Page. https://www.ninds.nih.gov/disorders/all-disorders/fahrs-syndrome-information-page | |||
</ | (accessed 7 May, 2018). | ||
</ref><ref name=":5">Calabro R, Spadaro L, Marra A, Bramanti P. Fahr's disease presenting with dementia at onset: a case report and literature review. Behav Neurol 2014;2014,750975. [http://dx.doi.org/10.1155/2014/750975 doi:10.1155/2014/750975]</ref>: | |||
* Basal ganglia (most commonly the globus pallidus) | |||
* Cerebellum (most commonly the dentate nucleus) | |||
* Thalamus | |||
* Hippocampus | |||
* Cerebral cortex | |||
=== | Calcifications are hypothesized to be due to lipid deposition and demyelination<ref name=":2">Murat Gülsün M, Baykız AF, Kabataş S, Belli B. Fahr’s Syndrome Three cases presenting with psychiatric signs. EJGM 2006;3(1):35-40. http://www.bioline.org.br/pdf?gm06008 (accessed 7 May, 2018).</ref>. The presentation of an individual with Fahr’s disease can vary greatly with some remaining asymptomatic despite receiving imaging confirmation of calcification. In more severe cases individuals will present first and most prominently with extrapyramidal symptoms<ref name=":8">Shafaq S, Aslam HM, Anwar M, Anwar S, Saleem M, Saleem A and Rehmani MAK. Fahr’s syndrome: literature review of current evidence. ORJD 2013;8-156. https://ojrd.biomedcentral.com/articles/10.1186/1750-1172-8-156 (accessed 7 May, 2018).</ref><ref name=":3">Goyal D, Khan M, Qureshi B, Mier C, Lippmann S. Would you recognize Fahr’s Disease if you saw it? ICN 2014;11(1-2):26-28. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3960784/ (accessed 7 May, 2018).</ref>. Further symptoms may include: progressive psychosis, cognitive impairment, [[dementia]], gait disturbance and sensory changes<ref name=":4">Radiopaedia. Fahr’s Syndrome. https://radiopaedia.org/articles/fahr-syndrome-1 (accessed 7 May, 2018).</ref>. Fahr’s syndrome can present at any age, but is typically first diagnosed in individuals between 40-60 years old<ref name=":1" /><ref name=":2" /><ref name=":3" /><ref name=":4" />. | ||
For anatomy of the brain see [[Brain Anatomy|here]] | |||
[[ | |||
== Aetiology == | |||
Fahr's syndrome is familial and inherited, with autosomal dominant cases making up 60% of diagnoses<ref name=":4" />. Some research has shown that fewer cases may be inherited in an autosomal recessive fashion<ref name=":5" />. There are also several other factors that could lead to brain calcification which include: endocrinopathies, vasculitis, mitochondrial disorders, infections, other inherited disorders, radiation, chemotherapy and carbon monoxide poisoning<ref name=":4" />. | |||
== Prognosis == | |||
== | Prognosis differs from person to person and thus is hard to predict<ref name=":1" />. Fahr’s syndrome is a progressive disease with no known cure and no specific treatments at this time<ref name=":4" />. Due to Fahr’s progressive and degenerative features individuals will often lose previously acquired skills and motor control, which can lead to death<ref>Fahr Too Strong Foundation. Commonly asked questions about Fahr’s Disease. http://www.fahrtoostrong.org/FAQ/ (accessed 7 May, 2018).</ref>. There is no direct correlation between the amount of calcium deposits that are seen in the brain and the degree of neurological impairments displayed by an individual with the disease<ref name=":1" /><ref name=":4" />. | ||
Prognosis differs from person to person and thus is hard to predict. Fahr’s syndrome is a progressive disease with no known cure and no specific treatments at this time. Due to Fahr’s progressive and degenerative features individuals will often lose previously acquired skills and motor control, which can lead to death. There is no direct correlation between the amount of calcium deposits that are seen in the brain and the degree of neurological impairments displayed by an individual with the disease. | |||
== Clinical Presentation == | == Clinical Presentation == | ||
Lesions in the basal ganglia can cause patients to present with different motor deficits. These include slowness of movement, involuntary extra movement and alterations in posture and muscle tone. Therefore patients with basal ganglia involvement can present on a continuum of motor behaviour from severely limited as seen in the final stages of [https://www.physio-pedia.com/Parkinson%27s_Disease Parkinson’s disease] to excessive movements apparent in [https://www.physio-pedia.com/Huntington_Disease Huntington’s disease]. In “Fahr’s Disease Registry”, the most common symptoms were movement disorders, in particular parkinsonism, which affects more than half of patients<ref | Lesions in the basal ganglia can cause patients to present with different motor deficits. These include slowness of movement, involuntary extra movement and alterations in posture and muscle tone<ref name=":6">Kandel, ER, Schwartz, JH, and Jessell. Principles of neural science. 4th ed. New York: McGraw-Hill; 2000. p 853.</ref>. Therefore patients with basal ganglia involvement can present on a continuum of motor behaviour from severely limited as seen in the final stages of [https://www.physio-pedia.com/Parkinson%27s_Disease Parkinson’s disease] to excessive movements apparent in [https://www.physio-pedia.com/Huntington_Disease Huntington’s disease]<ref name=":6" />. In “Fahr’s Disease Registry”, the most common symptoms were movement disorders, in particular parkinsonism, which affects more than half of patients<ref name=":5" />. | ||
{| class="wikitable" | {| class="wikitable" | ||
! colspan="2" |Associated Movement Disorders | ! colspan="2" |Associated Movement Disorders | ||
|- | |- | ||
|'''Dystonia''' | |'''Dystonia''' | ||
| | |A movement disorder that causes [https://www.physio-pedia.com/Hypertonicity_vs_spasticity sustained muscle contractions], abnormal postures and repetitive twisting movements that can vary in speed<ref>Velickovic M, Benabou R, Brin MF. Cervical dystonia: pathophysiology and treatment options. Drugs 2001;61(13),1921-1943. [http://dx.doi.org/10.2165/00003495-200161130-00004 doi:10.2165/00003495-200161130-00004]</ref>. Dystonia can affect one or several regions of the body<ref>Bressman SB. Dystonia genotypes, phenotypes, and classification. Adv in Neurol. 2004;94,101-107. https://www.ncbi.nlm.nih.gov/pubmed/14509661 (accessed 1 May 2018).</ref>. There is presently no cure for dystonia, but the goal is to help decrease the severity of muscle spasms, pain and awkward postures to improve overall quality of life<ref>The Dystonia Society. Generalized dystonia. https://www.dystonia.org.uk/generalised-dystonia (accessed 1 May 2018).</ref>. | ||
|- | |- | ||
|'''Athetosis''' | |'''Athetosis''' | ||
| | |A movement disorder characterised by slow, smooth, sinuous, writhing movements, also described as “wormlike movements”<ref>Johnson RK, Goran MI, Ferrara MS, Poehlman ET. Athetosis increases resting metabolic rate in adults with cerebral palsy. Journal of the American Dietetic Association. 1996 Feb 1;96(2):145-8.</ref>. More common in the distal upper extremities, but also prevalent in other areas of the body such as face, trunk, neck and tongue<ref>Haines DE, Ard MD. Fundamental neuroscience: for basic and clinical applications. 3rd ed. Philadelphia: Churchill Livingstone Elsevier; 2006. p413.</ref>. Pure Athetosis is uncommon as it usually presents with a combination of spasticity, tonic spasms or chorea<ref>Fahn S, Jankovic J, Hallett M. Clinical overview and phenomenology of movement disorders. Principles and practice of movement disorders. 2nd ed. Philadelphia: Elsevier Saunders; 2011:P1-35.</ref>. | ||
|- | |- | ||
|'''Chorea''' | |'''Chorea''' | ||
| | |Abnormal movement involving involuntary, irregular, purposeless, non-rhythmic, abrupt, rapid and unsustained, that can flow from one area of the body to another. These movements can vary in amplitude, small movements of the fingers to flailing of limb movements, referred to as ballism<ref>Micheli FE, LeWitt PA, SpringerLink (Online service). Chorea: causes and management. London: Springer London; 2014. https://link.springer.com/content/pdf/10.1007%2F978-1-4471-6455-5.pdf (accessed 1 May, 2018)</ref>. Patients are at an increased falls risk due to impairments in balance, strength and increased fatigue. Musculoskeletal and respiratory changes can result in physical deconditioning and contribute to decreased participation in daily activities and social participation<ref name=":13">European Huntington’s Disease Network. 2013. Physiotherapy clinical guidelines for Huntington’s disease. https://www.huntingtonsociety.ca/wp-content/uploads/2013/10/EHDN-Physio-Guide1.pdf (accessed 3 May 2018).</ref>. | ||
|- | |- | ||
|'''Spasticity''' | |'''[https://www.physio-pedia.com/Spasticity Spasticity]''' | ||
|motor disorder characterized by a velocity dependent increase in muscle tone with increased resistance to stretch, the larger and quicker the stretch, the stronger the resistance of the spastic muscle. During the rapid movement, a sudden inhibition or letting go of the limb termed the “clasp knife” response may follow initial high resistance. Chronic spasticity is associated with contracture, abnormal posturing and deformity, muscle weakness, functional limitations and disability<ref>O’Dwyer NJ, Ada L, Neilson PD. Spasticity and muscle contracture following stroke. Brain 1996;119:1737-1749. | |A motor disorder characterized by a velocity dependent increase in muscle tone with increased resistance to stretch, the larger and quicker the stretch, the stronger the resistance of the spastic muscle. During the rapid movement, a sudden inhibition or letting go of the limb termed the “clasp knife” response may follow initial high resistance. Chronic spasticity is associated with contracture, abnormal posturing and deformity, muscle weakness, functional limitations and disability<ref>O’Dwyer NJ, Ada L, Neilson PD. Spasticity and muscle contracture following stroke. Brain 1996;119:1737-1749. https://pdfs.semanticscholar.org/df70/aa84ee19dc6daed946a1de2d8ff26ed744fd.pdf (accessed 1 May 2018).</ref>. | ||
|- | |- | ||
|'''Tremor''' | |'''Tremor''' | ||
| | |Involuntary shaking movements. Tremor can be seen in the extremities, usually as a resting tremor the presents when a patient is at rest, or in the head and trunk, when the patient is trying to hold an upright posture<ref name=":7">Bilney B, Morris ME, Denisenko S. Physiotherapy for people with movement disorders arising from basal ganglia dysfunction. N Z J Physiother 2013;31(2),94-100. https://pdfs.semanticscholar.org/be52/87e4d93e8576b28fde1ab44b23217bac279d.pdf (accessed 5 May 2018).</ref>. A resting tremor can eventually progress to an action tremor, which is tremor with movement. Although the pathophysiology is slightly different from Fahr's, Parkinson’s patients tend to exhibit a mild tremor first on only one side of the body<ref name=":7" />; there is not enough data to decisively say if this it true for Fahr’s patients. Tremors tend to worsen with stress, anxiety or an excited emotional state<ref name=":7" />. Particularly in later stages, tremors interfere with the ability to perform functional activities, especially fine motor tasks such as picking up or holding objects. | ||
|- | |- | ||
|'''Rigidity''' | |'''Rigidity''' | ||
| | |Increased resistance to passive movement that is not affected by speed or amplitude of motion<ref name=":7" />. There are two types: lead pipe - which is constant throughout range - and cogwheel - which is jerky with tension felt intermittently throughout a movement<ref name=":7" />. Rigidity affects a patient’s ability to move and therefore independently carry out activities of daily living (ADLs). In many patients, rigidity can be increased by stress or active movements. | ||
|- | |- | ||
|'''Hypomimia''' | |'''Hypomimia''' | ||
| | |The reduced ability to portray facial expressions, both automatic and voluntary, that is often seen in Parksinon’s and Fahr’s patients. This frozen, masked expression is often incorrectly interpreted by others as [[depression]], coldness, apathy and reduced cognition<ref name=":0">Tickle-Degnen L, Zebrowitz LA, Ma H. Culture, gender and health care stigma: practitioners' response to facial masking experienced by people with Parkinson's. Soc Sci Med. 2011;73:95-102. [http://dx.doi.org/10.1016/j.socscimed.2011.05.008 doi:10.1016/j.socscimed.2011.05.008]</ref>. This can cause difficulty in communication and relationships, including patient-therapist relationships; studies have shown that practitioners - including physiotherapists - tend to view patients with facial masking as more depressed, less sociable and less cognitively competent<ref name=":0" />. Therefore it is an important component of the treatment of Fahr’s disease to not allow oneself to form negative preconceptions about a client based on a symptom they cannot control. | ||
|- | |- | ||
|'''Gait''' | |'''Gait''' | ||
| | |Affected by Fahr’s disease similarly to Parkinson’s disease. Fahr’s patients can exhibit unsteadiness, clumsiness, a shuffling gait, or freezing of gait<ref>Stamelou M, Kojovic M, Edwards MJ, Bhatia KP. Ability to cycle despite severe freezing of gait in atypical parkinsonism in Fahr's syndrome. Movement Disorders. 2011;26:2141-2142. [http://dx.doi.org/10.1002/mds.23794 doi:10.1002/mds.23794]</ref>. '''Hypokinesia''', which is a generalized slowness of movement, can also manifest in gait as an increased time to initiate and execute movement as well as decreased force generation<ref name=":7" />. | ||
|- | |- | ||
|'''Hypokinesia''' | |'''Hypokinesia''' | ||
| | |A generalized slowness of movement. It can also manifest in gait as an increased time to initiate and execute movement as well as decreased force generation<ref name=":7" />. | ||
|} | |} | ||
'''Neuropsychiatric and Other Symptoms | '''''Neuropsychiatric and Other Symptoms''''' | ||
Due to the heterogeneity of brain calcifications and associated impairments, it is common to see a wide variety of symptoms other than movement disorders. These include epileptic seizures, dysarthria, mood disorders, problems with cognition (memory and concentration), behaviour/personality changes, psychosis and dementia | Due to the heterogeneity of brain calcifications and associated impairments, it is common to see a wide variety of symptoms other than movement disorders<ref name=":8" />. These include epileptic seizures, dysarthria, mood disorders, problems with cognition (memory and concentration), behaviour/personality changes, psychosis and dementia<ref name=":8" /><ref name=":9">National Organization for Rare Disorders. Primary Familial Brain Calcification Information Page. | ||
https://rarediseases.org/rare-diseases/primary-familial-brain-calcification/ (Accessed 7 May, 2018) | |||
</ref>. While some of these symptoms may not be directly treatable with physiotherapy interventions, they do affect considerations for treatment and are important to keep in mind when planning for patient care. Included below are links to resources within Physiopedia and external sources that provide more information regarding these symptoms. | |||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
{| class="wikitable" | {| class="wikitable" | ||
!Diagnostic criteria | !Diagnostic criteria | ||
|- | |- | ||
|1. Genetic abnormality and family history inheritance of autosomal dominant trait or autosomal recessive trait | |''1. Genetic abnormality and family history inheritance of autosomal dominant trait or autosomal recessive trait''<ref name=":4" /><ref name=":10">Ramos EM. Primary Familial Brain Calcification [Internet]. Advances in pediatrics. Gene Reviews.org; 2017 [cited 2018May7]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1421/#bgc.Management</ref> | ||
|- | |- | ||
|2. Bilateral calcification in Basal Ganglia visible on neuroimaging | |''2. Bilateral calcification in Basal Ganglia visible on neuroimaging''<ref name=":8" /><ref name=":10" /> | ||
|- | |- | ||
|3. Exclude secondary causes of Fahr syndrome and biochemical abnormalities (infection, traumatic injury, metabolic, toxic) | |''3. Exclude secondary causes of Fahr syndrome and biochemical abnormalities (infection, traumatic injury, metabolic, toxic)''<ref name=":8" /><ref name=":10" /> | ||
|- | |- | ||
|4. Progressive neurological dysfunction involving movement and psychiatric disorders | |''4. Progressive neurological dysfunction involving movement and psychiatric disorders''<ref name=":8" /><ref name=":4" /><ref name=":9" /><ref name=":10" /> | ||
|} | |} | ||
=== Neuroimaging === | |||
* CT | [[File:Fahr syndrome.jpg|400px|thumb|Fig. 2 Brain CT scan in a patient with Fahr's syndrome<ref>Mikhail Kalinin. Brain CT scan in a patient with Fahr's syndrome [image on the Internet]. 5 October 2009. Available from: https://commons.wikimedia.org/wiki/File:Fahr_syndrome.gif</ref>]] | ||
* CT - used to assess the location and severity of cerebral calcification<ref name=":4" /><ref name=":10" /> | |||
* MRI - | * MRI - generally less useful than CT, may be used to locate calcification in the brain, but appearance varies depending on stage of disease and the amount of calcification<ref name=":4" /><ref name=":10" /> | ||
* | * X-ray - may be used to locate symmetrical calcium clusters lateral to midline<ref name=":4" /><ref name=":10" /> | ||
=== Tests === | |||
* Molecular Genetic testing - assess presence of mutations or deletions in SLC20A2 or PDGFRB gene<ref name=":8" /> | |||
* Urine and blood analysis - assess calcium metabolism and presence of heavy metals in the body<ref name=":8" /> | |||
* CSF analysis - assess possible infectious or autoimmune cause of brain calcification<ref name=":8" /> | |||
=== Physical Exam === | |||
* Complete Neurological Exam | |||
* Assess Strength,Tone and Spasticity | |||
* Assess Balance, Gait, Function Assessment (see Outcome Measures below) | |||
=== Other Assessments === | |||
* Mental Health Screen | |||
* Memory and Cognitive Testing | |||
== Outcome Measures == | == Outcome Measures == | ||
* [[Functional Independence Measure (FIM)]] | |||
* [[Dynamic Gait Index]] | |||
* [[Functional Gait Assessment]] | |||
* [[Timed Up and Go Test (TUG)]] | |||
* [[Fullerton Advanced Balance (FAB) scale]] | |||
* [[Neurological Outcome Measures|Neurology Outcome Measures]] | |||
== Medical Management == | == Medical Management == | ||
There is no cure or standard treatment plan for Fahr’s syndrome. Symptoms and disease presentation are treated on an individual basis. Pharmacologic treatment can be helping in alleviating seizures, headaches and some psychiatric symptoms<ref name=":10" />. There are no known studies on whether dementia medications are helpful in treating associated symptoms in Fahr's Syndrome. Parkinson-like symptoms are generally non-responsive to Levodopa<ref name=":10" />. | |||
== Physiotherapy Intervention == | == Physiotherapy Intervention == | ||
Due to the lack of literature on Fahr’s disease and the similarity of symptoms with Parkinson’s, Huntington’s and other neurological conditions, therapists should use their clinical judgement in combination with evidence about the treatment of the overlapping symptoms in similar populations. Recommendations for treatment include a focus on function, participation and exercise capacity, as well as preventing or slowing the progression of secondary impairments such as muscle weakness<ref name=":11" />. | |||
{| class="wikitable" | {| class="wikitable" | ||
!Treatment Goals May Include | !Treatment Goals May Include | ||
|- | |- | ||
|1. Increase and/or maintain range of motion, prevent contractures | |''1. Increase and/or maintain range of motion, prevent contractures'' | ||
|- | |- | ||
|2. Strengthen weakened muscles that may be underutilized | |''2. Strengthen weakened muscles that may be underutilized'' | ||
|- | |- | ||
|3. Improvement and maintenance of postural stability in static postures and during mobility | |''3. Improvement and maintenance of postural stability in static postures and during mobility'' | ||
|- | |- | ||
|4. Gait retraining and/or falls prevention | |''4. Gait retraining and/or falls prevention'' | ||
|- | |- | ||
|5. Symptom management | |''5. Symptom management'' | ||
|} | |} | ||
# '''Maintaining Range of Motion and Flexibility''' | # '''Maintaining Range of Motion and Flexibility''' | ||
#* Range of motion exercises, passive stretching and facilitated stretching can help maintain tissue extensibility and physical functioning. Stretching can be combined with joint mobilization | #* Range of motion exercises, passive stretching and facilitated stretching can help maintain tissue extensibility and physical functioning<ref name=":11">O’Sullivan SB, Schmitz TJ, Fulk GD. Physical rehabilitation. 6th ed. Philadelphia: F.A. Davis Company, 2014. Chapter 10.</ref>. These exercises should ideally be done 5-7 days per week, but at least 2-3 days, with 3-4 reps of at least 15-60 seconds per stretch<ref name=":12">O’Sullivan SB, Schmitz TJ, Fulk GD. Physical rehabilitation. 6th ed. Philadelphia: F.A. Davis Company, 2014. Chapter 18.</ref>. Stretching can be combined with [https://www.physio-pedia.com/images/c/c0/Principles_of_Joint_Mobilization.pdf joint mobilization]<ref name=":12" />. | ||
#* Note for patients with spasticity, therapist should use constant pressure over bony prominences and avoid direct pressure on spastic muscles. Limb movement out of spastic position should be slow, repeated motions | #* Note for patients with spasticity, therapist should use constant pressure over bony prominences and avoid direct pressure on spastic muscles. Limb movement out of spastic position should be slow, repeated motions<ref name=":11" />. | ||
#* Serial casts may be used for patients at risk of contractures and deformity | #* Serial casts may be used for patients at risk of contractures and deformity<ref name=":11" />. | ||
#* Note for patients with dystonia, braces may be helpful in preventing contractures. However, they tend to be poorly tolerated and are only really used for writer’s cramp to enable the hand to be used more effectively and comfortably | #* Note for patients with dystonia, braces may be helpful in preventing contractures. However, they tend to be poorly tolerated and are only really used for writer’s cramp to enable the hand to be used more effectively and comfortably<ref>Chaudhuri KR, Ondo WG, Logishetty K, Reddy P, Sherman R. Movement disorders in clinical practice. 1st ed. London: Springer; 2010. p49-65.</ref> | ||
# '''Strengthening Underutilized Muscles''' | # '''Strengthening Underutilized Muscles''' | ||
#* A general conditioning program is beneficial for most patients with neurological disorders to maintain strength and function. | #* A general conditioning program is beneficial for most patients with neurological disorders to maintain strength and function<ref name=":12" />. | ||
#* Include the principles of overload, specificity, cross training and reversibility in designing a program. Note with specificity, it is best to attempt to create exercises that will carry over into the client’s daily life, for example following an isometric protocol will not guarantee effects carry over to improved dynamic performance which is more applicable to ADLs. | #* Include the principles of overload, specificity, cross training and reversibility in designing a program. Note with specificity, it is best to attempt to create exercises that will carry over into the client’s daily life, for example following an isometric protocol will not guarantee effects carry over to improved dynamic performance which is more applicable to ADLs<ref name=":11" />. | ||
#* Muscles that commonly become weak in neurological populations include antigravity extensor muscles | #* Muscles that commonly become weak in neurological populations include antigravity extensor muscles<ref name=":12" />. | ||
#* Exercise machines, in contrast to free weights, may be safer for patients with more progressed motor symptoms since movements are more controlled<ref name=":12" />. | |||
#* Exercise machines, in contrast to free weights, may be safer for patients with more progressed motor symptoms since movements are more controlled. | |||
# '''Improving Postural Instability''' | # '''Improving Postural Instability''' | ||
#* Instruct patient in correct sitting posture, using appropriate vertical cuing such as lines on the wall, and the clinician exhibiting appropriate upright posture | #* Instruct patient in correct sitting posture, using appropriate vertical cuing such as lines on the wall, and the clinician exhibiting appropriate upright posture<ref name=":11" /> | ||
#* Patients with basal ganglia dysfunction are recommended to practice maintenance of postural control in a variety of tasks and environments and incorporate activities that require anticipatory responses | #* Patients with basal ganglia dysfunction are recommended to practice [https://www.physio-pedia.com/Balance maintenance of postural control] in a variety of tasks and environments and incorporate activities that require anticipatory responses<ref name=":7" /> | ||
#* Progress activities from wide to narrow base of support, static to dynamic, low to higher levels of cognition – single vs. dual task, also increasing degrees of freedom available | #* Progress activities from wide to narrow base of support, static to dynamic, low to higher levels of cognition – single vs. dual task, also increasing degrees of freedom available<ref name=":11" /> | ||
#* Patients with basal ganglia dysfunction are encouraged to incorporate task specific balance training, specifically during functional activities such as transfers, reaching, and using stairs | #* Patients with basal ganglia dysfunction are encouraged to incorporate task specific balance training, specifically during functional activities such as transfers, reaching, and using stairs<ref name=":7" /> | ||
# '''Gait retraining/Falls Prevention''' | # '''[[Gait]] retraining/[[Falls]] Prevention''' | ||
#* For patients with basal ganglia dysfunction, auditory cueing may assist with step timing, for example counting, stepping to a metronome or music. In particular, common strategies to improve Parkinsonian symptoms such as the regularity of gait and gait freezing, include visual cues like lasers attached to a walker or cane. Individual studies have also shown that participation in other activities, such as dance and high-speed cycling, can potentially improve gait. | #* For patients with basal ganglia dysfunction, auditory cueing may assist with step timing, for example counting, stepping to a metronome or music<ref name=":7" />. In particular, common strategies to improve Parkinsonian symptoms such as the regularity of gait and gait freezing, include visual cues like lasers attached to a walker or cane<ref name=":12" />. Individual studies have also shown that participation in other activities, such as dance and high-speed cycling, can potentially improve gait<ref>Uygur M, Bellumori M, LeNoir K, Poole K, Pretzer-Aboff I, Knight CA. Immediate effects of high-speed cycling intervals on bradykinesia in Parkinson's. Physiother Theor Pr 2015;31:77-82. [http://dx.doi.org/10.3109/09593985.2014.972530 doi:10.3109/09593985.2014.972530]</ref>. | ||
#* Provision of assistive devices when appropriate to improve function | #* Provision of assistive devices when appropriate to improve function<ref name=":12" /> | ||
#* Educate patient on safety awareness, including how to get up after a fall and decreasing clutter in their living space | #* Educate patient on safety awareness, including how to get up after a fall and decreasing clutter in their living space | ||
#* Assessment for orthotic device may be required (for example ankle dystonia) | #* Assessment for orthotic device may be required (for example ankle dystonia)<ref name=":13" /> | ||
#* For hyperkinetic disorders, protective gear such as helmets, pads may be required if at high risk for falls | #* For hyperkinetic disorders, protective gear such as helmets, pads may be required if at high risk for falls<ref name=":13" /> | ||
# '''Symptom Management''' | # '''Symptom Management''' | ||
#* Relaxation techniques, such as deep breathing, are beneficial because patients with neurological conditions such as Fahr’s disease tend to experience a lot of stress and anxiety. Relaxation has documented benefits including elevated energy levels and a greater perception of control. | #* Relaxation techniques, such as deep breathing, are beneficial because patients with neurological conditions such as Fahr’s disease tend to experience a lot of stress and anxiety. Relaxation has documented benefits including elevated energy levels and a greater perception of control<ref name=":11" />. | ||
#* For hyperkinetic disorders, deep brain stimulation. Which involves a surgically implanted device that sends electrical impulses to the brain to help control movement | #* For hyperkinetic disorders, deep brain stimulation. Which involves a surgically implanted device that sends electrical impulses to the brain to help control movement<ref>di Biase L, Munhoz R. Deep brain stimulation for the treatment of hyperkinetic movement disorders. Expert Rev Neurother 2016;16:1067-1078. [http://dx.doi.org/10.1080/14737175.2016.1196139 doi: 10.1080/14737175.2016.1196139]</ref>. | ||
#* Soft tissue release is beneficial for patients experiencing dystonia and spasticity. Case studies have also shown benefits of massage for Parkinson’s symptoms, including gait, range of motion, pain and upper limb function. | #* Soft tissue release is beneficial for patients experiencing dystonia and spasticity<ref>Perrault E. 2010. The effectiveness of muscle energy and massage therapy for the management of symptoms related to chronic cervical dystonia. https://casere3.dspacedirect.org/handle/11106/26 (accessed 3 May 2018).</ref><ref>Bavikatte G, Gaber T. Approach to spasticity in General practice. Brit J of Med Pract 2009;2:29. http://www.bjmp.org/files/sept2009/bjmp0909bavikatte.pdf (accessed 5 May 2018).</ref>. Case studies have also shown benefits of [[massage]] for Parkinson’s symptoms, including gait, range of motion, pain and upper limb function<ref>Donoyama N, Ohkoshi N. Effects of traditional Japanese massage therapy on various symptoms in patients with Parkinson's: a case-series study. J Altern Complement Med 2012;18:294-299. [http://dx.doi.org/10.1089/acm.2011.0148 doi: 10.1089/acm.2011.0148]</ref><ref>Donoyama N, Suoh S, Ohkoshi N. Effectiveness of Anma massage therapy in alleviating physical symptoms in outpatients with Parkinson's: a before-after study. Complement Ther Clin Pract 2014;20:251-261. [http://dx.doi.org/10.1016/j.ctcp.2014.07.010 doi:10.1016/j.ctcp.2014.07.010]</ref>. | ||
#* Sensory stimulation for patients with basal ganglia dysfunction. | #* Sensory stimulation for patients with basal ganglia dysfunction. Note that for patients living with dystonia, many will develop sensory tricks on their own that help to improve dystonic posture, for example touching specific parts of the face. The benefits of these tricks are transient in nature and may have less effect during the later stages of the disease<ref>Ramos VFML, Karp BI, Hallett M. Tricks in dystonia: ordering the complexity. J Neurol Neurosurg Psychiatry 2014;85(9):987-993. [http://dx.doi.org/10.1136/jnnp-2013-306971 doi:10.1136/jnnp-2013-306971]</ref>, | ||
#* There is some evidence that whole body vibration (WBV) may improve gait, tremor, rigidity, proprioception and balance in patients with neurological diseases, including Parkinson’s<ref name=":12" />. However, systematic reviews have concluded that more high-quality research is needed<ref name=":12" />. | |||
#* There is some evidence that whole body vibration (WBV) may improve gait, tremor, rigidity, proprioception and balance in patients with neurological diseases, including Parkinson’s. However, systematic reviews have concluded that more high-quality research is needed | {| class="wikitable" | ||
!Additional Treatment Planning Links | |||
|- | |||
|[https://www.physio-pedia.com/Core_stability Core Stability] | |||
|- | |||
|[[Neurology Treatment Techniques]] | |||
|- | |||
|[[Motor Control and Learning]] | |||
|- | |||
|[[Coordination Exercises]] | |||
|- | |||
|[[Parkinson's and Dance]] | |||
|} | |||
== Resources for Patients == | == Resources for Patients == | ||
* [https://www.caregiver.org Family Caregiver Alliance] | |||
* [http://www.fahrtoostrong.org/Latest-Research/ Fahr Too Strong Foundation] | |||
* [https://rarediseases.info.nih.gov/diseases/6406/primary-familial-brain-calcification#diseaseOverviewSection Genetic and Rare Diseases Information Centre (GARD)] | |||
** [https://rarediseases.info.nih.gov/guides/pages/120/support-for-patients-and-families GARD - Support for Patients and Families] | |||
** [https://rarediseases.info.nih.gov/guides/pages/25/how-to-find-a-disease-specialist GARD - How to Find a Disease Specialist] | |||
* [https://www.ninds.nih.gov/Disorders/All-Disorders/Fahrs-Syndrome-Information-Page National Institute of Neurological Disorders and Stroke] | |||
* [https://rarediseases.org/rare-diseases/primary-familial-brain-calcification/ National Organization of Rare Disorders] | |||
* [https://rareundiagnosed.org Rare and Undiagnosed Network] | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Queen's University Neuromotor Function Project]] | |||
[[Category:Neurology]] [[Category:Neurological | [[Category:Neurology]] | ||
[[Category:Neurological - Conditions]] | |||
[[Category:Conditions]] | |||
Latest revision as of 11:24, 24 May 2022
Original Editor - Sarah Dorsey, Maria Tyumkin, Megan Willerth, Jennifer Withers, Logan Wood as part of the Queen's University Neuromotor Function Project
Introduction[edit | edit source]
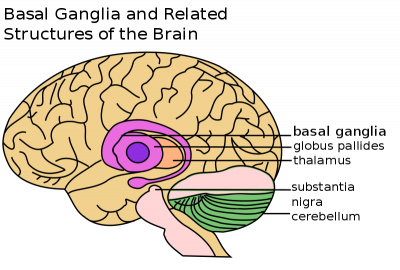
Fahr’s syndrome is also known as Fahr’s disease, familial idiopathic basal ganglia calcification and primary familial brain calcification. It is a rare neurological disorder characterized by bilateral calcifications of areas in the brain including[2][3]:
- Basal ganglia (most commonly the globus pallidus)
- Cerebellum (most commonly the dentate nucleus)
- Thalamus
- Hippocampus
- Cerebral cortex
Calcifications are hypothesized to be due to lipid deposition and demyelination[4]. The presentation of an individual with Fahr’s disease can vary greatly with some remaining asymptomatic despite receiving imaging confirmation of calcification. In more severe cases individuals will present first and most prominently with extrapyramidal symptoms[5][6]. Further symptoms may include: progressive psychosis, cognitive impairment, dementia, gait disturbance and sensory changes[7]. Fahr’s syndrome can present at any age, but is typically first diagnosed in individuals between 40-60 years old[2][4][6][7].
For anatomy of the brain see here
Aetiology[edit | edit source]
Fahr's syndrome is familial and inherited, with autosomal dominant cases making up 60% of diagnoses[7]. Some research has shown that fewer cases may be inherited in an autosomal recessive fashion[3]. There are also several other factors that could lead to brain calcification which include: endocrinopathies, vasculitis, mitochondrial disorders, infections, other inherited disorders, radiation, chemotherapy and carbon monoxide poisoning[7].
Prognosis[edit | edit source]
Prognosis differs from person to person and thus is hard to predict[2]. Fahr’s syndrome is a progressive disease with no known cure and no specific treatments at this time[7]. Due to Fahr’s progressive and degenerative features individuals will often lose previously acquired skills and motor control, which can lead to death[8]. There is no direct correlation between the amount of calcium deposits that are seen in the brain and the degree of neurological impairments displayed by an individual with the disease[2][7].
Clinical Presentation[edit | edit source]
Lesions in the basal ganglia can cause patients to present with different motor deficits. These include slowness of movement, involuntary extra movement and alterations in posture and muscle tone[9]. Therefore patients with basal ganglia involvement can present on a continuum of motor behaviour from severely limited as seen in the final stages of Parkinson’s disease to excessive movements apparent in Huntington’s disease[9]. In “Fahr’s Disease Registry”, the most common symptoms were movement disorders, in particular parkinsonism, which affects more than half of patients[3].
| Associated Movement Disorders | |
|---|---|
| Dystonia | A movement disorder that causes sustained muscle contractions, abnormal postures and repetitive twisting movements that can vary in speed[10]. Dystonia can affect one or several regions of the body[11]. There is presently no cure for dystonia, but the goal is to help decrease the severity of muscle spasms, pain and awkward postures to improve overall quality of life[12]. |
| Athetosis | A movement disorder characterised by slow, smooth, sinuous, writhing movements, also described as “wormlike movements”[13]. More common in the distal upper extremities, but also prevalent in other areas of the body such as face, trunk, neck and tongue[14]. Pure Athetosis is uncommon as it usually presents with a combination of spasticity, tonic spasms or chorea[15]. |
| Chorea | Abnormal movement involving involuntary, irregular, purposeless, non-rhythmic, abrupt, rapid and unsustained, that can flow from one area of the body to another. These movements can vary in amplitude, small movements of the fingers to flailing of limb movements, referred to as ballism[16]. Patients are at an increased falls risk due to impairments in balance, strength and increased fatigue. Musculoskeletal and respiratory changes can result in physical deconditioning and contribute to decreased participation in daily activities and social participation[17]. |
| Spasticity | A motor disorder characterized by a velocity dependent increase in muscle tone with increased resistance to stretch, the larger and quicker the stretch, the stronger the resistance of the spastic muscle. During the rapid movement, a sudden inhibition or letting go of the limb termed the “clasp knife” response may follow initial high resistance. Chronic spasticity is associated with contracture, abnormal posturing and deformity, muscle weakness, functional limitations and disability[18]. |
| Tremor | Involuntary shaking movements. Tremor can be seen in the extremities, usually as a resting tremor the presents when a patient is at rest, or in the head and trunk, when the patient is trying to hold an upright posture[19]. A resting tremor can eventually progress to an action tremor, which is tremor with movement. Although the pathophysiology is slightly different from Fahr's, Parkinson’s patients tend to exhibit a mild tremor first on only one side of the body[19]; there is not enough data to decisively say if this it true for Fahr’s patients. Tremors tend to worsen with stress, anxiety or an excited emotional state[19]. Particularly in later stages, tremors interfere with the ability to perform functional activities, especially fine motor tasks such as picking up or holding objects. |
| Rigidity | Increased resistance to passive movement that is not affected by speed or amplitude of motion[19]. There are two types: lead pipe - which is constant throughout range - and cogwheel - which is jerky with tension felt intermittently throughout a movement[19]. Rigidity affects a patient’s ability to move and therefore independently carry out activities of daily living (ADLs). In many patients, rigidity can be increased by stress or active movements. |
| Hypomimia | The reduced ability to portray facial expressions, both automatic and voluntary, that is often seen in Parksinon’s and Fahr’s patients. This frozen, masked expression is often incorrectly interpreted by others as depression, coldness, apathy and reduced cognition[20]. This can cause difficulty in communication and relationships, including patient-therapist relationships; studies have shown that practitioners - including physiotherapists - tend to view patients with facial masking as more depressed, less sociable and less cognitively competent[20]. Therefore it is an important component of the treatment of Fahr’s disease to not allow oneself to form negative preconceptions about a client based on a symptom they cannot control. |
| Gait | Affected by Fahr’s disease similarly to Parkinson’s disease. Fahr’s patients can exhibit unsteadiness, clumsiness, a shuffling gait, or freezing of gait[21]. Hypokinesia, which is a generalized slowness of movement, can also manifest in gait as an increased time to initiate and execute movement as well as decreased force generation[19]. |
| Hypokinesia | A generalized slowness of movement. It can also manifest in gait as an increased time to initiate and execute movement as well as decreased force generation[19]. |
Neuropsychiatric and Other Symptoms
Due to the heterogeneity of brain calcifications and associated impairments, it is common to see a wide variety of symptoms other than movement disorders[5]. These include epileptic seizures, dysarthria, mood disorders, problems with cognition (memory and concentration), behaviour/personality changes, psychosis and dementia[5][22]. While some of these symptoms may not be directly treatable with physiotherapy interventions, they do affect considerations for treatment and are important to keep in mind when planning for patient care. Included below are links to resources within Physiopedia and external sources that provide more information regarding these symptoms.
Diagnostic Procedures[edit | edit source]
| Diagnostic criteria |
|---|
| 1. Genetic abnormality and family history inheritance of autosomal dominant trait or autosomal recessive trait[7][23] |
| 2. Bilateral calcification in Basal Ganglia visible on neuroimaging[5][23] |
| 3. Exclude secondary causes of Fahr syndrome and biochemical abnormalities (infection, traumatic injury, metabolic, toxic)[5][23] |
| 4. Progressive neurological dysfunction involving movement and psychiatric disorders[5][7][22][23] |
Neuroimaging[edit | edit source]
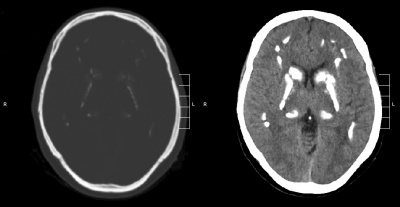
- CT - used to assess the location and severity of cerebral calcification[7][23]
- MRI - generally less useful than CT, may be used to locate calcification in the brain, but appearance varies depending on stage of disease and the amount of calcification[7][23]
- X-ray - may be used to locate symmetrical calcium clusters lateral to midline[7][23]
Tests[edit | edit source]
- Molecular Genetic testing - assess presence of mutations or deletions in SLC20A2 or PDGFRB gene[5]
- Urine and blood analysis - assess calcium metabolism and presence of heavy metals in the body[5]
- CSF analysis - assess possible infectious or autoimmune cause of brain calcification[5]
Physical Exam[edit | edit source]
- Complete Neurological Exam
- Assess Strength,Tone and Spasticity
- Assess Balance, Gait, Function Assessment (see Outcome Measures below)
Other Assessments[edit | edit source]
- Mental Health Screen
- Memory and Cognitive Testing
Outcome Measures[edit | edit source]
- Functional Independence Measure (FIM)
- Dynamic Gait Index
- Functional Gait Assessment
- Timed Up and Go Test (TUG)
- Fullerton Advanced Balance (FAB) scale
- Neurology Outcome Measures
Medical Management[edit | edit source]
There is no cure or standard treatment plan for Fahr’s syndrome. Symptoms and disease presentation are treated on an individual basis. Pharmacologic treatment can be helping in alleviating seizures, headaches and some psychiatric symptoms[23]. There are no known studies on whether dementia medications are helpful in treating associated symptoms in Fahr's Syndrome. Parkinson-like symptoms are generally non-responsive to Levodopa[23].
Physiotherapy Intervention[edit | edit source]
Due to the lack of literature on Fahr’s disease and the similarity of symptoms with Parkinson’s, Huntington’s and other neurological conditions, therapists should use their clinical judgement in combination with evidence about the treatment of the overlapping symptoms in similar populations. Recommendations for treatment include a focus on function, participation and exercise capacity, as well as preventing or slowing the progression of secondary impairments such as muscle weakness[25].
| Treatment Goals May Include |
|---|
| 1. Increase and/or maintain range of motion, prevent contractures |
| 2. Strengthen weakened muscles that may be underutilized |
| 3. Improvement and maintenance of postural stability in static postures and during mobility |
| 4. Gait retraining and/or falls prevention |
| 5. Symptom management |
- Maintaining Range of Motion and Flexibility
- Range of motion exercises, passive stretching and facilitated stretching can help maintain tissue extensibility and physical functioning[25]. These exercises should ideally be done 5-7 days per week, but at least 2-3 days, with 3-4 reps of at least 15-60 seconds per stretch[26]. Stretching can be combined with joint mobilization[26].
- Note for patients with spasticity, therapist should use constant pressure over bony prominences and avoid direct pressure on spastic muscles. Limb movement out of spastic position should be slow, repeated motions[25].
- Serial casts may be used for patients at risk of contractures and deformity[25].
- Note for patients with dystonia, braces may be helpful in preventing contractures. However, they tend to be poorly tolerated and are only really used for writer’s cramp to enable the hand to be used more effectively and comfortably[27]
- Strengthening Underutilized Muscles
- A general conditioning program is beneficial for most patients with neurological disorders to maintain strength and function[26].
- Include the principles of overload, specificity, cross training and reversibility in designing a program. Note with specificity, it is best to attempt to create exercises that will carry over into the client’s daily life, for example following an isometric protocol will not guarantee effects carry over to improved dynamic performance which is more applicable to ADLs[25].
- Muscles that commonly become weak in neurological populations include antigravity extensor muscles[26].
- Exercise machines, in contrast to free weights, may be safer for patients with more progressed motor symptoms since movements are more controlled[26].
- Improving Postural Instability
- Instruct patient in correct sitting posture, using appropriate vertical cuing such as lines on the wall, and the clinician exhibiting appropriate upright posture[25]
- Patients with basal ganglia dysfunction are recommended to practice maintenance of postural control in a variety of tasks and environments and incorporate activities that require anticipatory responses[19]
- Progress activities from wide to narrow base of support, static to dynamic, low to higher levels of cognition – single vs. dual task, also increasing degrees of freedom available[25]
- Patients with basal ganglia dysfunction are encouraged to incorporate task specific balance training, specifically during functional activities such as transfers, reaching, and using stairs[19]
- Gait retraining/Falls Prevention
- For patients with basal ganglia dysfunction, auditory cueing may assist with step timing, for example counting, stepping to a metronome or music[19]. In particular, common strategies to improve Parkinsonian symptoms such as the regularity of gait and gait freezing, include visual cues like lasers attached to a walker or cane[26]. Individual studies have also shown that participation in other activities, such as dance and high-speed cycling, can potentially improve gait[28].
- Provision of assistive devices when appropriate to improve function[26]
- Educate patient on safety awareness, including how to get up after a fall and decreasing clutter in their living space
- Assessment for orthotic device may be required (for example ankle dystonia)[17]
- For hyperkinetic disorders, protective gear such as helmets, pads may be required if at high risk for falls[17]
- Symptom Management
- Relaxation techniques, such as deep breathing, are beneficial because patients with neurological conditions such as Fahr’s disease tend to experience a lot of stress and anxiety. Relaxation has documented benefits including elevated energy levels and a greater perception of control[25].
- For hyperkinetic disorders, deep brain stimulation. Which involves a surgically implanted device that sends electrical impulses to the brain to help control movement[29].
- Soft tissue release is beneficial for patients experiencing dystonia and spasticity[30][31]. Case studies have also shown benefits of massage for Parkinson’s symptoms, including gait, range of motion, pain and upper limb function[32][33].
- Sensory stimulation for patients with basal ganglia dysfunction. Note that for patients living with dystonia, many will develop sensory tricks on their own that help to improve dystonic posture, for example touching specific parts of the face. The benefits of these tricks are transient in nature and may have less effect during the later stages of the disease[34],
- There is some evidence that whole body vibration (WBV) may improve gait, tremor, rigidity, proprioception and balance in patients with neurological diseases, including Parkinson’s[26]. However, systematic reviews have concluded that more high-quality research is needed[26].
| Additional Treatment Planning Links |
|---|
| Core Stability |
| Neurology Treatment Techniques |
| Motor Control and Learning |
| Coordination Exercises |
| Parkinson's and Dance |
Resources for Patients[edit | edit source]
- Family Caregiver Alliance
- Fahr Too Strong Foundation
- Genetic and Rare Diseases Information Centre (GARD)
- National Institute of Neurological Disorders and Stroke
- National Organization of Rare Disorders
- Rare and Undiagnosed Network
References[edit | edit source]
- ↑ John Henkel. Structure of the basal ganglia, including thalamus, globus paladus, substantia nigra, and cerebellum [image on the Internet]. Food and Drug Administration, 23 March 2009, 17:14 (UTC). Available from: https://commons.wikimedia.org/wiki/File:Basal_Ganglia_and_Related_Structures.svg
- ↑ 2.0 2.1 2.2 2.3 National Institute of Neurological Disorder and Stroke. Fahr’s Syndrome Information Page. https://www.ninds.nih.gov/disorders/all-disorders/fahrs-syndrome-information-page (accessed 7 May, 2018).
- ↑ 3.0 3.1 3.2 Calabro R, Spadaro L, Marra A, Bramanti P. Fahr's disease presenting with dementia at onset: a case report and literature review. Behav Neurol 2014;2014,750975. doi:10.1155/2014/750975
- ↑ 4.0 4.1 Murat Gülsün M, Baykız AF, Kabataş S, Belli B. Fahr’s Syndrome Three cases presenting with psychiatric signs. EJGM 2006;3(1):35-40. http://www.bioline.org.br/pdf?gm06008 (accessed 7 May, 2018).
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 5.8 Shafaq S, Aslam HM, Anwar M, Anwar S, Saleem M, Saleem A and Rehmani MAK. Fahr’s syndrome: literature review of current evidence. ORJD 2013;8-156. https://ojrd.biomedcentral.com/articles/10.1186/1750-1172-8-156 (accessed 7 May, 2018).
- ↑ 6.0 6.1 Goyal D, Khan M, Qureshi B, Mier C, Lippmann S. Would you recognize Fahr’s Disease if you saw it? ICN 2014;11(1-2):26-28. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3960784/ (accessed 7 May, 2018).
- ↑ 7.00 7.01 7.02 7.03 7.04 7.05 7.06 7.07 7.08 7.09 7.10 Radiopaedia. Fahr’s Syndrome. https://radiopaedia.org/articles/fahr-syndrome-1 (accessed 7 May, 2018).
- ↑ Fahr Too Strong Foundation. Commonly asked questions about Fahr’s Disease. http://www.fahrtoostrong.org/FAQ/ (accessed 7 May, 2018).
- ↑ 9.0 9.1 Kandel, ER, Schwartz, JH, and Jessell. Principles of neural science. 4th ed. New York: McGraw-Hill; 2000. p 853.
- ↑ Velickovic M, Benabou R, Brin MF. Cervical dystonia: pathophysiology and treatment options. Drugs 2001;61(13),1921-1943. doi:10.2165/00003495-200161130-00004
- ↑ Bressman SB. Dystonia genotypes, phenotypes, and classification. Adv in Neurol. 2004;94,101-107. https://www.ncbi.nlm.nih.gov/pubmed/14509661 (accessed 1 May 2018).
- ↑ The Dystonia Society. Generalized dystonia. https://www.dystonia.org.uk/generalised-dystonia (accessed 1 May 2018).
- ↑ Johnson RK, Goran MI, Ferrara MS, Poehlman ET. Athetosis increases resting metabolic rate in adults with cerebral palsy. Journal of the American Dietetic Association. 1996 Feb 1;96(2):145-8.
- ↑ Haines DE, Ard MD. Fundamental neuroscience: for basic and clinical applications. 3rd ed. Philadelphia: Churchill Livingstone Elsevier; 2006. p413.
- ↑ Fahn S, Jankovic J, Hallett M. Clinical overview and phenomenology of movement disorders. Principles and practice of movement disorders. 2nd ed. Philadelphia: Elsevier Saunders; 2011:P1-35.
- ↑ Micheli FE, LeWitt PA, SpringerLink (Online service). Chorea: causes and management. London: Springer London; 2014. https://link.springer.com/content/pdf/10.1007%2F978-1-4471-6455-5.pdf (accessed 1 May, 2018)
- ↑ 17.0 17.1 17.2 European Huntington’s Disease Network. 2013. Physiotherapy clinical guidelines for Huntington’s disease. https://www.huntingtonsociety.ca/wp-content/uploads/2013/10/EHDN-Physio-Guide1.pdf (accessed 3 May 2018).
- ↑ O’Dwyer NJ, Ada L, Neilson PD. Spasticity and muscle contracture following stroke. Brain 1996;119:1737-1749. https://pdfs.semanticscholar.org/df70/aa84ee19dc6daed946a1de2d8ff26ed744fd.pdf (accessed 1 May 2018).
- ↑ 19.0 19.1 19.2 19.3 19.4 19.5 19.6 19.7 19.8 19.9 Bilney B, Morris ME, Denisenko S. Physiotherapy for people with movement disorders arising from basal ganglia dysfunction. N Z J Physiother 2013;31(2),94-100. https://pdfs.semanticscholar.org/be52/87e4d93e8576b28fde1ab44b23217bac279d.pdf (accessed 5 May 2018).
- ↑ 20.0 20.1 Tickle-Degnen L, Zebrowitz LA, Ma H. Culture, gender and health care stigma: practitioners' response to facial masking experienced by people with Parkinson's. Soc Sci Med. 2011;73:95-102. doi:10.1016/j.socscimed.2011.05.008
- ↑ Stamelou M, Kojovic M, Edwards MJ, Bhatia KP. Ability to cycle despite severe freezing of gait in atypical parkinsonism in Fahr's syndrome. Movement Disorders. 2011;26:2141-2142. doi:10.1002/mds.23794
- ↑ 22.0 22.1 National Organization for Rare Disorders. Primary Familial Brain Calcification Information Page. https://rarediseases.org/rare-diseases/primary-familial-brain-calcification/ (Accessed 7 May, 2018)
- ↑ 23.0 23.1 23.2 23.3 23.4 23.5 23.6 23.7 23.8 Ramos EM. Primary Familial Brain Calcification [Internet]. Advances in pediatrics. Gene Reviews.org; 2017 [cited 2018May7]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1421/#bgc.Management
- ↑ Mikhail Kalinin. Brain CT scan in a patient with Fahr's syndrome [image on the Internet]. 5 October 2009. Available from: https://commons.wikimedia.org/wiki/File:Fahr_syndrome.gif
- ↑ 25.0 25.1 25.2 25.3 25.4 25.5 25.6 25.7 O’Sullivan SB, Schmitz TJ, Fulk GD. Physical rehabilitation. 6th ed. Philadelphia: F.A. Davis Company, 2014. Chapter 10.
- ↑ 26.0 26.1 26.2 26.3 26.4 26.5 26.6 26.7 26.8 O’Sullivan SB, Schmitz TJ, Fulk GD. Physical rehabilitation. 6th ed. Philadelphia: F.A. Davis Company, 2014. Chapter 18.
- ↑ Chaudhuri KR, Ondo WG, Logishetty K, Reddy P, Sherman R. Movement disorders in clinical practice. 1st ed. London: Springer; 2010. p49-65.
- ↑ Uygur M, Bellumori M, LeNoir K, Poole K, Pretzer-Aboff I, Knight CA. Immediate effects of high-speed cycling intervals on bradykinesia in Parkinson's. Physiother Theor Pr 2015;31:77-82. doi:10.3109/09593985.2014.972530
- ↑ di Biase L, Munhoz R. Deep brain stimulation for the treatment of hyperkinetic movement disorders. Expert Rev Neurother 2016;16:1067-1078. doi: 10.1080/14737175.2016.1196139
- ↑ Perrault E. 2010. The effectiveness of muscle energy and massage therapy for the management of symptoms related to chronic cervical dystonia. https://casere3.dspacedirect.org/handle/11106/26 (accessed 3 May 2018).
- ↑ Bavikatte G, Gaber T. Approach to spasticity in General practice. Brit J of Med Pract 2009;2:29. http://www.bjmp.org/files/sept2009/bjmp0909bavikatte.pdf (accessed 5 May 2018).
- ↑ Donoyama N, Ohkoshi N. Effects of traditional Japanese massage therapy on various symptoms in patients with Parkinson's: a case-series study. J Altern Complement Med 2012;18:294-299. doi: 10.1089/acm.2011.0148
- ↑ Donoyama N, Suoh S, Ohkoshi N. Effectiveness of Anma massage therapy in alleviating physical symptoms in outpatients with Parkinson's: a before-after study. Complement Ther Clin Pract 2014;20:251-261. doi:10.1016/j.ctcp.2014.07.010
- ↑ Ramos VFML, Karp BI, Hallett M. Tricks in dystonia: ordering the complexity. J Neurol Neurosurg Psychiatry 2014;85(9):987-993. doi:10.1136/jnnp-2013-306971






