ACE Inhibitors: Congestive Heart Failure: Difference between revisions
(Blanked the page) |
No edit summary |
||
| (27 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:User Name|Lauren Pulliam Southern]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | |||
== Introduction == | |||
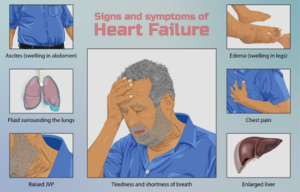
[[File:Heart failure.png|right|frameless|Heart Failure]] | |||
[[Angiotensin Inhibitors and Blockers for Treating Hypertension|Angiotensin Converting Enzyme (ACE) Inhibitors]] are a important class of drugs used in the management of [[Cardiovascular Disease|cardiovascular]] and [[Chronic Kidney Disease|renal disease]]<nowiki/>s, including [[Heart Failure|Congestive Heart Failure]] (CHF), [[Acute Coronary Syndrome|acute coronary syndrome]], nephrotic syndrome, [[diabetes]], and [[hypertension]]. | |||
Using an angiotensin-converting enzyme (ACE) inhibitor drug is an important part of treating heart failure. ACE inhibitors are strongly recommended as first-choice therapy in patients with heart failure<ref>Herman LL, Padala SA, Annamaraju P, Bashir K. Angiotensin converting enzyme inhibitors (ACEI). StatPearls [Internet]. 2021 Jun 18.Available: https://www.ncbi.nlm.nih.gov/books/NBK431051/#!po=6.81818<nowiki/>(accessed 6.4.2022)</ref>. | |||
== Effects == | |||
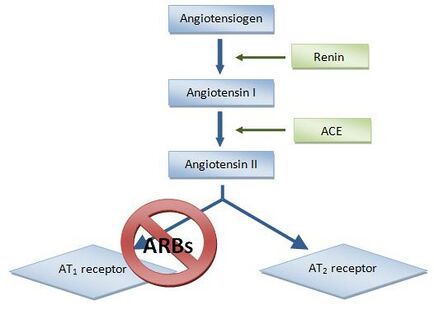
[[File:Renin ang pathway 2.jpeg|right|frameless|434x434px]] | |||
Angiotensin-converting enzyme inhibitors (ACEIs) improve heart failure by decreasing afterload, preload, and systolic wall stress, which results in increased cardiac output without any increase in [[Heart Rate|heart rate]]. | |||
ACE inhibitors play an important role in: | |||
* Promoting salt excretion by augmenting the renal [[Blood Physiology|blood]] flow and reducing [[Aldosterone Receptor Antagonist Diuretics in the treatment of congestive heart failure|aldosterone]] and antidiuretic hormone production. | |||
* Reducing [[Muscle: Cardiac|cardiac myocyte]] hypertrophy (angiotensin II is also responsible for hypertrophy of vascular tissues) | |||
* Increasing bradykinin levels in the blood by decreasing their breakdown. Bradykinin is responsible for vasodilation. | |||
Since the 1980s, several large, prospective, randomized, placebo-controlled trials have proved that treatment with ACE inhibitors reduces overall mortality, especially in patients with heart failure with reduced ejection fraction. | |||
== Common Ace Inhibitors == | |||
Several ACE inhibitors are on the market, and it is generally thought that they are equally beneficial in the treatment of heart failure. Commonly used ACE inhibitors include: | |||
* Accupril (quinapril) | |||
* Altace (ramipril) | |||
* Capoten (captopril) | |||
* Mavik (trandalopril) | |||
* Monopril (fosinopril) | |||
* Vasotec (enalapril) | |||
* Zestril (lisinopril)<ref>Very well health How ACE Inhibitors Treat Heart Failure Available:https://www.verywellhealth.com/ace-inhibitors-for-treating-heart-failure-4120575 (accessed 6.4.2022)</ref> | |||
== Implications for Physiotherapy == | |||
[[File:Syncope.jpeg|thumb|Syncope AKA Fainting, swooning]] | |||
ACE inhibitors cause a reduction in [[Blood Pressure|blood pressure]], this coupled with the naturally occurring post-exercise [[hypotension]] can result in excessive reductions in blood pressure. This can lead to dizziness and, in rare instances, syncope. | |||
Post-exercising clients on ACE inhibitors may need education in adhering to a gradual cool-down after each and every exercise session to prevent these symptoms and benefit the body by enhancing venous return and the prevention of blood pooling in the [[Muscle|skeletal muscle]]. A gradual cool-down of five to 10 minutes of light [[Aerobic Exercise|aerobic]] activity allows the body to return to homeostasis and prevents excessive reductions in blood pressure.<ref>American Council of Exercise [https://www.acefitness.org/certifiednewsarticle/3296/how-common-medications-may-affect-your-clients/ How Common Medications May Affect Your Clients’ Exercise Programs] Available from: https://www.acefitness.org/certifiednewsarticle/3296/how-common-medications-may-affect-your-clients/ (last accessed 17.6.2019)</ref> | |||
[[File:Hf.png|center|frameless|517x517px]] | |||
== References == | |||
<references /> | |||
[[Category:Cardiovascular Disease]] | |||
[[Category:Pharmacology]] | |||
[[Category:Pharmacology for Cardiovascular Disease]] | |||
[[Category:Older People/Geriatrics]] | |||
Latest revision as of 06:04, 6 April 2022
Introduction[edit | edit source]
Angiotensin Converting Enzyme (ACE) Inhibitors are a important class of drugs used in the management of cardiovascular and renal diseases, including Congestive Heart Failure (CHF), acute coronary syndrome, nephrotic syndrome, diabetes, and hypertension.
Using an angiotensin-converting enzyme (ACE) inhibitor drug is an important part of treating heart failure. ACE inhibitors are strongly recommended as first-choice therapy in patients with heart failure[1].
Effects[edit | edit source]
Angiotensin-converting enzyme inhibitors (ACEIs) improve heart failure by decreasing afterload, preload, and systolic wall stress, which results in increased cardiac output without any increase in heart rate.
ACE inhibitors play an important role in:
- Promoting salt excretion by augmenting the renal blood flow and reducing aldosterone and antidiuretic hormone production.
- Reducing cardiac myocyte hypertrophy (angiotensin II is also responsible for hypertrophy of vascular tissues)
- Increasing bradykinin levels in the blood by decreasing their breakdown. Bradykinin is responsible for vasodilation.
Since the 1980s, several large, prospective, randomized, placebo-controlled trials have proved that treatment with ACE inhibitors reduces overall mortality, especially in patients with heart failure with reduced ejection fraction.
Common Ace Inhibitors[edit | edit source]
Several ACE inhibitors are on the market, and it is generally thought that they are equally beneficial in the treatment of heart failure. Commonly used ACE inhibitors include:
- Accupril (quinapril)
- Altace (ramipril)
- Capoten (captopril)
- Mavik (trandalopril)
- Monopril (fosinopril)
- Vasotec (enalapril)
- Zestril (lisinopril)[2]
Implications for Physiotherapy[edit | edit source]
ACE inhibitors cause a reduction in blood pressure, this coupled with the naturally occurring post-exercise hypotension can result in excessive reductions in blood pressure. This can lead to dizziness and, in rare instances, syncope.
Post-exercising clients on ACE inhibitors may need education in adhering to a gradual cool-down after each and every exercise session to prevent these symptoms and benefit the body by enhancing venous return and the prevention of blood pooling in the skeletal muscle. A gradual cool-down of five to 10 minutes of light aerobic activity allows the body to return to homeostasis and prevents excessive reductions in blood pressure.[3]
References[edit | edit source]
- ↑ Herman LL, Padala SA, Annamaraju P, Bashir K. Angiotensin converting enzyme inhibitors (ACEI). StatPearls [Internet]. 2021 Jun 18.Available: https://www.ncbi.nlm.nih.gov/books/NBK431051/#!po=6.81818(accessed 6.4.2022)
- ↑ Very well health How ACE Inhibitors Treat Heart Failure Available:https://www.verywellhealth.com/ace-inhibitors-for-treating-heart-failure-4120575 (accessed 6.4.2022)
- ↑ American Council of Exercise How Common Medications May Affect Your Clients’ Exercise Programs Available from: https://www.acefitness.org/certifiednewsarticle/3296/how-common-medications-may-affect-your-clients/ (last accessed 17.6.2019)