Upper Limb Preservation in Spinal Cord Injury
Original Editor - Ewa Jaraczewska based on the course by Wendy Oelofse
Top Contributors - Ewa Jaraczewska, Jess Bell and Tarina van der Stockt
Introduction[edit | edit source]
Mechanical upper limb problems, including pain, weakness from overuse, range of motion limitations or contracture, are common complications in persons with spinal cord injuries (SCI). An interdisciplinary team assessment is needed to identify risk factors leading to mechanical upper extremity problems. A periodic health review of a person with a spinal cord injury can provide information to help diagnose and treat these problems.[1] This article explores strategies to preserve the upper limb and prevent pain with activities of daily living in clients with spinal cord injuries.
Risk Factors Assessment[edit | edit source]
The primary risk factor for upper limb injuries in clients with spinal cord injury is related to changes in upper limb function from manipulation to weight bearing for mobility. Additional risk factors in patients with spinal cord injuries include:
- Repetitive use of the upper limb
- New medical problems
- Weight gain
- Changes in medical status
Overuse injuries include:[2]
- Shoulder pain (present in 30-60% of clients with paraplegia and tetraplegia)
- Shoulder pain: 71%; wrist pain: 51%; hand pain: 43%; and elbow pain: 35%[3]
- Carpal tunnel syndrome (present in 40-66% of persons with spinal cord injury)
- Median nerve neuropathy (present in 78% of wheelchair users)
- Ulnar nerve entrapment at both the wrist and elbow
- Tendinitis
- Osteoarthritis
- Lateral epicondylitis
- Olecranon bursitis
- Rotator cuff tear
- Shoulder impingement
- Adhesive capsulitis of the glenohumeral joint
- Recurrent shoulder dislocations
- Bicipital tendinitis
Interdisciplinary Team Assessment[edit | edit source]
Periodic assessment is recommended to gain insight into a client's new vs old problems and establish the most effective care plan. At the minimum, this assessment should include the following:
- Pain assessment
- Aetiology
- Intensity
- Functional limitations
- New medical problems influencing function[4]
- The interface between age and length of time from spinal cord injury onset[3]
- Upper extremity joint range of motion and muscle strength limitations or imbalances[3]
- Exercise capacity and tolerance for the physical demands of activities of daily living[3]
- Body mass and composition[3]
- Previous upper extremity injury or disease history[3]
- Psychosocial adjustment
- Assessment of the client's environment
- Home, work, or school environment
- Means of transportation
- Equipment assessment
- Manual vs power wheelchair
- Seating system
- Bathroom equipment
Treatment Plan[edit | edit source]
A treatment plan should include the following:
- Early and appropriate treatment for pain associated with acute musculoskeletal injuries
- Development of a chronic pain prevention programme
- Introduction of alternative techniques for activities
Transfers[edit | edit source]
There is evidence suggesting that transfers can lead to upper limb injury in clients with spinal cord injuries.[4] This is because, during a transfer, the shoulders must support the body's weight and shift the trunk mass between the outreached hands. This activity demands 2.5 times more pressure than when the shoulder is not bearing weight.[4] The forces associated with transfers affect the shoulders, wrists, and hands:
- Shoulders:
- Support body weight
- Shift the trunk mass between hands
- Wrists:
- Positioned in extreme wrist extension
- Hands:
- Palms stay flat
These demands can lead to shoulder pain, increased pressure in the carpal tunnel and median nerve compression.
Interventions[edit | edit source]
- Keep the shoulders open by externally rotating arms[5]
- Lean forward to take the weight off the buttocks[5]
- Create momentum during transfers[5]
- Complete transfers in stages when using a transfer board[5]
- Choose transfer surfaces that are either at equal height or downhill[4]
- Consider a roll-in shower chair/commode to decrease the number of transfers throughout the day
- During transfers, place hands in a position that avoids extreme wrist extension, e.g. draping over and grasping the transfer surface's edge[4]
- Transfer using a closed-fist with the wrist in neutral (but watch for instability!)
- Please note, to preserve a tenodesis grip, the wrist should be extended, and the fingers flexed during transfers
- Lead with the arm experiencing pain when possible during transfers[5]
Pressure Relief[edit | edit source]
All persons with spinal cord injury should complete regular repositioning training. Repositioning movements reduce the pressure around the ischial tuberosity and sacral regions.
Repositioning movements include vertical push-ups and lateral and forward leans. Repositioning movements should be performed every 15-30 minutes for adequate pressure relief.[6] However, research has shown that patients' compliance with these recommendations is poor.[7] Push-up pressure relief is usually held for less than 20 seconds, which is inadequate to achieve tissue reperfusion.[6] It has been found that, overall, the effectiveness of the vertical push-up and lateral lean weight shifts is low.
According to research, forward leans should be the most frequently recommended method to relieve pressure. A 40° forward lean leads to decreased muscle and soft tissue deformation at the ischial tuberosity, while a 45° forward lean produces the most significant decrease in maximum pressure.[6] A forwards lean can be achieved by leaning with the elbows on the knees, on a table, or supported by the back of another chair. This position can be maintained for prolonged periods when stable and secure.[8]
Advantages of lean forward pressure relief:[5]
- Preserves the shoulders
- Allows for more time to replenish the blood supply to the area
- The position can be maintained for an extended time
Disadvantages of lean forward pressure relief:[8]
- May be difficult for a person with arthritis
- May be hard to achieve for a person with obesity
Shoulder Elevation[edit | edit source]
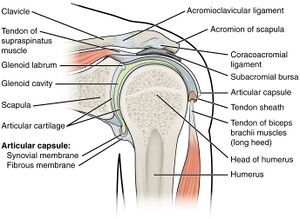
Compression of the supraspinatus tendon is most likely to occur at 30-60 degrees of humerothoracic elevation.[10] Research shows that individuals with a cervical spinal cord injury are frequently in 30-60 degrees of shoulder elevation. For example, during wheelchair propulsion at a self-selected speed, humeral elevation reaches 25-55 degrees.[10] Finley et al.[11] also report that humeral elevation occurs five times more often in wheelchair users than in persons without spinal cord injuries.
Glenohumeral and scapulothoracic kinematics affect subacromial proximities.[12] During overhead-reaching activities, there is a linear relationship between reduced scapular external rotation, posterior tilt and thoracic kyphosis in individuals with spinal cord injury.[11] In addition, the degree of maximal elevation in patients with spinal cord injury decreases as thoracic kyphosis increases. As a result, all tasks that require above-shoulder height movement can increase the risk of shoulder pain and injury in clients with spinal cord injuries.
Interventions[edit | edit source]
- Try to avoid reaching overhead[5]
- Avoid using overhead bars/monkey chains[5]
- Assess for appropriate wheelchair seating and positioning to prevent or reduce a patient's thoracic kyphosis
- When an overhead reach is necessary for car transfers, minimise internal rotation of the arm[5]
- Modify environments where items are stored overhead[5]
Manual Wheelchair Mobility[edit | edit source]
As mentioned, shoulder pain and injury among wheelchair users are common. Shoulder forces during manual wheelchair propulsion can be affected by multiple factors. However, one study showed that personal factors, including a person's body weight, were the primary demographic variable that affected shoulder forces.[13] Other factors include:
- Personal factors
- Shoulder muscle weakness, specifically shoulder adductors,[14] leads to compensatory muscle patterns
- The choice of wheelchair[5]
- Type
- Position of the rear axle
- Seat position
- Tyre pressure
- Biomechanics during wheelchair propulsion
- "Peak shoulder joint loading occurs when the arm is extended and internally rotated, which may leave the shoulder at risk for injury"[13]
- To maintain independence with wheelchair propulsion, persons with spinal cord injury tend to develop "a protective short-term wheelchair propulsion biomechanical response",[15] including decreased glenohumeral flexion/extension and reduced scapular angles[15]
- Increases in wheelchair propulsion speed increase the load on the upper limb muscles and joints[14]
Interventions[edit | edit source]
Personal factors
- Include a body-weight maintenance programme
- A strengthening programme should target the shoulder adductors to decrease the likelihood that shoulder pain will develop[16]
The choice of the wheelchair
- Select a light-weight, customised wheelchair
- Position the rear axle as far forward as possible without compromising the user's stability
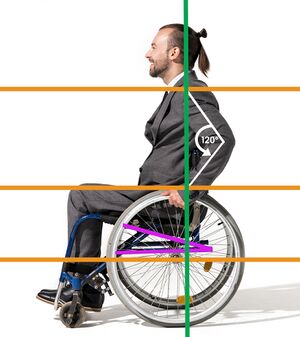
- When the hand is placed at the top-dead-centre position on the push rim, the angle between the upper arm and forearm should fall between 100 and 120 degrees
- Adjust the wheelchair seat to a lower position without compromising the upper limb position; too much shoulder abduction will increase the risk of shoulder impingement
- Inflate the tyres properly to decrease the friction between the tyre and the floor
Biomechanics during wheelchair propulsion
- Use long, smooth strokes that limit impact on the push rim[5]
- Allow the hand to drift down naturally, keeping it below the push rim when not in contact with that part of the wheelchair[5]
Tasks and Environment Modification[edit | edit source]
Environment[edit | edit source]
"A thorough assessment of the environments where routine transfers, activities of daily living, and work are performed is necessary for consumers and clinicians to know when and where to intervene." Wendy Oelofse
Manual wheelchair users face different barriers when accessing outdoor environments. They include slopes, cross-slopes, curbs, and various ground types.[17]
Interventions[edit | edit source]
- Complete a thorough assessment of the client’s environment (school, work, home, outdoors)
- Reduce forces in the extremities
- Reduce the frequency at which difficult-to-perform activities are completed
- Modify the home environment
- For example, transfer overhead cabinets to a lower location and modify a home to ensure that transfers are level
Tasks[edit | edit source]
Interventions[edit | edit source]
- Avoid activities that involve raising the arm above shoulder height
- Use adaptive equipment (e.g. a reacher)
- Keep frequently used items within easy reach
- Incorporate overall health promotion and a wellness-oriented lifestyle programme[1]
Resources[edit | edit source]
- Lawrence RL, Braman JP, Ludewig PM. Shoulder kinematics impact subacromial proximities: a review of the literature. Braz J Phys Ther. 2020 May-Jun;24(3):219-230.
- Slowik JS, Requejo PS, Mulroy SJ, Neptune RR. The influence of wheelchair propulsion hand pattern on upper extremity muscle power and stress. J Biomech. 2016 Jun 14;49(9):1554-1561.
References[edit | edit source]
- ↑ 1.0 1.1 United States. Public Health Service. Office of the Surgeon General, National Center for Chronic Disease Prevention, Health Promotion (US), President's Council on Physical Fitness, Sports (US). Physical activity and health: A report of the surgeon general. US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion; 1996.
- ↑ SPINAL CORD INJURY GUIDELINES 2021. Department of Physical Medicine and Rehabilitation / Trauma Rehabilitation Resources Program. Available from https://medicine.uams.edu/pmr/wp-content/uploads/sites/3/2021/02/Guidelines-SCI-Upper-Extremity-2021.pdf [last access 16.12.2022]
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Nyland J, Quigley P, Huang C, Lloyd J, Harrow J, Nelson A. Preserving transfer independence among individuals with spinal cord injury. Spinal cord. 2000 Nov;38(11):649-57.
- ↑ 4.0 4.1 4.2 4.3 4.4 Paralyzed Veterans of America Consortium for Spinal Cord Medicine. Preservation of upper limb function following spinal cord injury: a clinical practice guideline for health-care professionals. J Spinal Cord Med. 2005;28(5):434-70.
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 5.12 Oelofse W. Spinal Cord Injury Programme - Upper Limb Preservation in Spinal Cord Injury - Occupational Therapy Course. Plus 2022
- ↑ 6.0 6.1 6.2 Stinson M, Schofield R, Gillan C, Morton J, Gardner E, Sprigle S, Porter-Armstrong A. Spinal cord injury and pressure ulcer prevention: using functional activity in pressure relief. Nurs Res Pract. 2013;2013:860396.
- ↑ Yang YS, Chang GL, Hsu MJ, Chang JJ. Remote monitoring of sitting behaviours for community-dwelling manual wheelchair users with spinal cord injury. Spinal Cord. 2009 Jan;47(1):67-71.
- ↑ 8.0 8.1 van Etten M. Repositioning for pressure ulcer prevention in the seated individual. Available from https://www.woundsme.com/uploads/resources/a3f8eea01d76d5a35425663841e79e03.pdf [last access 19.12.2022]
- ↑ Healthy Tomorrow. How To Do Pressure Relief - Leaning Forward (Manual Wheelchair). Available from: https://www.youtube.com/watch?v=BdzcYiI-16g [last accessed 21/12/2022]
- ↑ 10.0 10.1 Goodwin BM, Cain SM, Van Straaten MG, Fortune E, Jahanian O, Morrow MM. Humeral elevation workspace during the daily life of adults with spinal cord injury who use a manual wheelchair compared to age and sex-matched able-bodied controls. PloS one. 2021 Apr 23;16(4):e0248978.
- ↑ 11.0 11.1 Finley MA, Euiler E, Hiremath SV, Sarver J. Movement coordination during humeral elevation in individuals with newly acquired spinal cord injury. Journal of Applied Biomechanics. 2020 Aug 14;36(5):345-50.
- ↑ Lawrence RL, Braman JP, Ludewig PM. Shoulder kinematics impact subacromial proximities: a review of the literature. Braz J Phys Ther. 2020 May-Jun;24(3):219-230.
- ↑ 13.0 13.1 Collinger JL, Boninger ML, Koontz AM, Price R, Sisto SA, Tolerico ML, Cooper RA. Shoulder biomechanics during the push phase of wheelchair propulsion: a multisite study of persons with paraplegia. Arch Phys Med Rehabil. 2008 Apr;89(4):667-76.
- ↑ 14.0 14.1 Walford SL, Rankin JW, Mulroy SJ, Neptune RR. The relationship between the hand pattern used during fast wheelchair propulsion and shoulder pain development. Journal of Biomechanics. 2021 Feb 12;116:110202.
- ↑ 15.0 15.1 Briley SJ, Vegter RJ, Goosey-Tolfrey VL, Mason BS. The longitudinal relationship between shoulder pain and altered wheelchair propulsion biomechanics of manual wheelchair users. Journal of biomechanics. 2021 Sep 20;126:110626.
- ↑ Walford SL, Requejo PS, Mulroy SJ, Neptune RR. Predictors of shoulder pain in manual wheelchair users. Clin Biomech (Bristol, Avon). 2019 May;65:1-12.
- ↑ Rouvier T, Louessard A, Simonetti E, Hybois S, Bascou J, Pontonnier C, Pillet H, Sauret C. Manual wheelchair biomechanics while overcoming various environmental barriers: A systematic review. PloS one. 2022 Jun 23;17(6):e0269657.