Meniscal Lesions
Original Editor - De Wolf Zora Rachael Lowe
Top Contributors - Robine Allart, Vidya Acharya, Kim Jackson, Oyemi Sillo, Thibaut Seys, Amanda Ager, Admin, Tony Lowe, Maarten Cnudde, Daphne Jackson, Naike De Win, WikiSysop, Evan Thomas, Kai A. Sigel, Rucha Gadgil, Wanda van Niekerk, 127.0.0.1 and Jess Bell
Introduction[edit | edit source]
The medial and lateral menisci play an important role in absorbing force and assisting in the role of nourishing the knee joint. An injury can cause altered biomechanics of the knee joint and pain. This page will explore how and what happens when the menisci become injured (a tear and/or a rupture). Meniscal tears are the most common lesions followed by the meniscal cyst. Both of them have 2 causes. The first one is traumatic and the second one is a degenerative meniscal tear. A meniscal cyst may present with signs and symptoms consistent with typical meniscal pathology. The discoid meniscus is a rare congenital disorder where the lateral meniscus remains around instead of its usual cupped shape leading to instability of the lateral compartment. This condition is usually asymptomatic but may become symptomatic if a meniscal tear occurs.
Epidemiology/Etiology[edit | edit source]
Meniscus injuries are often seen in athletes as a result of a sports injury and represent approximately 15% of all cases sports injuries. A meniscus can be torn or can be completely ruptured. There are partial or total ruptures of a lateral or medial meniscus.[1] Medial tears are reported more commonly than lateral tears. In addition to tears occurring in sports, osteoarthritis can also lead to a spontaneous meniscal tear through breakdown and weakening of the meniscal structure.
Epidemiology studies on meniscal lesions are hampered by the fact that probably many such lesions are never recognized, for meniscal tears do not necessarily present with characteristic symptoms, and some may heal spontaneously. [2]
Meniscal injuries are more common in males, because they are more involved in aggressive sporting. Men are more likely to have bucket-handle lesions than women, bucket handle lesions are related to trauma. Women sustained more peripheral detachments. [2] Another striking fact is observed in elderly persons (older than 55 years) where a degenerate meniscus is susceptible to injuries with minor trauma. Nowadays, meniscal lesions appear later in life than earlier. The mean age rose from 28 to 40 years. Meniscal injuries are unusual in children under the age of 10 years. [2]
There are no significant differences in meniscus tear type, location, or zone between different ages, and more importantly, the repair rate is similar. Adolescents were more likely to have concurrent ligamentous injuries, which might be explained in part by increased participation in competitive sports at that age. Among children complex tears were associated with boys (32% vs 10% in girls) and those with higher BMI. The majority of meniscal tears affect the lateral meniscus and involve the posterior horn of the meniscus. [3]
Traumatic meniscal tear:[edit | edit source]
- There are 2 criteria to define a meniscal lesion as traumatic. These two criteria must be met: the meniscal tissue must be healthy of normal macroscopic appearance and there must be an injury to the knee such as a knee sprain or a forced movement.
- Most of the time a traumatic lesion is a vertical or a longitudinal tear.[4] [5] [6]
Meniscal tears are either due to an excessive force applied to a 'normal' meniscus or a normal force acting on a degenerative meniscus. The most common mechanism of injury is a twisting injury on a semi-flexed limb through a weight bearing knee. It may also be associated with other ligamentus injuries, typically the ACL and the MCL. There are two different types of meniscal tears:
- Acute tears - These are commonly the result of a trauma or a sports injury (sports like tennis, jogging, soccer,…). Acute tears have different shapes (horizontal, vertical, radial, oblique and complex). If they do not respond to conservative management, surgical management may be indicated.
- Chronic tears - These most often occur in elderly people, and are degenerative meniscal tears that occur after minimal trauma or stress on the knee. They are mostly treated with physical therapy and anti-inflammatory medication.
Degenerative meniscal tear:[edit | edit source]
- Occurs in the absence of a trauma.
- Is due to the age of the person and everyday activities.
- The meniscal tissue has deteriorated to a certain degree.
- Men are more prone to a degenerative tear than women.
- A degenerative tear can occur early in someone’s life, for example, a young athletes, but it normally occurs in the fourth of the fifth decade of life. [4] [7]
Meniscal rupture:[edit | edit source]
A meniscus injury is generally caused by a torsional movement between the femur and the tibia under load without contact, or making an abrupt movement like a squat. Anything which allows the femur to slip too much forward or backward in relation to the tibia may cause some of the forces to be transmitted to the meniscus, resulting in a meniscus rupture.
Clinically Relevant Anatomy[edit | edit source]
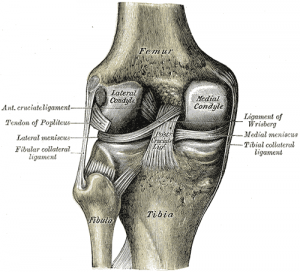
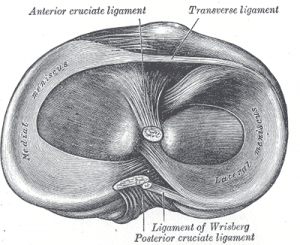
The 2 menisci are crescent-shaped fibrocartilaginous structures that are present in the knee between the femoral condyles and the tibia plateau. Anterior and posterior meniscal horns attach to the intercondylar eminence of the tibial plateau. The coronary ligaments provide peripheral attachments between the tibial plateau and the perimeter of both menisci. The insertional ligament of the anterior horn of the medial meniscus is fan-shaped and attaches to the tibia in the area of the intercondylar fossa, about 6 or 7 mm anterior to the attachment of the anterior cruciate ligament. [8] The anterior intermeniscal ligament, also known as the transverse geniculate ligament, connects the anterior fibers of the anterior horns of the medial and lateral menisci. [9] The relevance of the ligament has not been studied yet, but it may have a role in moving the menisci during tibia internal-external rotation. The length of this ligament is 33mm[9] . The medial meniscus is also attached to the medial collateral ligament, which limits its mobility. The lateral meniscus is connected to the femur via the anterior (ligament of Humphrey) and posterior (ligament of Wrisberg) meniscofemoral ligaments, which can tension its posterior horn anteriorly and medially with increasing knee flexion. The transverse ligament provides a connection between the anterior aspects of both menisci. The increased stability provided by the ligamentous attachments prevents the menisci from being extruded out of the joint during compression.
The meniscus is typically an avascular structure with the primary blood supply limited to the periphery. Only the peripheral 10% to 25% of the meniscus is vascularized by vessels that are derived from the middle, medial, and lateral geniculate arteries. For that reason, when meniscus is damaged in the central portion it is usually unable to undergo a normal healing process. The most peripheral portion of the meniscus has a blood supply and is more likely to heal.
Characteristics/Clinical Presentation[edit | edit source]
The clinical presentation handles the symptoms associated with a meniscal lesion. But we have to make the difference between a traumatic meniscal lesion and a degenerative meniscal lesion. Symptoms for a traumatic meniscal lesion are produced by instability of the torn fragment. [10] These symptoms can result in the locking of the knee in case of ‘bucket-handle’ tears. It is also responsible for popping of the knee and you can also hear the knee clicking when the torn part of the meniscus moves under the femoral condyle. Other more disturbing symptoms include medial or lateral knee pain depending on the affected compartment, which is caused by an abnormal increase in tension of the joint capsule.
With a degenerative meniscus the symptoms are the same as in a traumatic meniscal lesion, although there may also can be problems with the patella or the cartilage. Symptoms are frequently worsened by flexing and loading the knee, activities such as squatting and kneeling are poorly tolerated.
The clinical presentation for a traumatic lesion/rupture:[edit | edit source]
• Joint line tenderness, Mc Murray test,[11] Thessaly test and squat test
• Symptoms are popping sound and intermittent residual pain.
• Occurs mostly in aged population. The age of onset is mostly over 50 years of age.
• Hyper-flexion of the knee for a long period of time under weight-bearing lead to excessive pressure.[12]
• Medial meniscus resists more pressure during weight bearing than the lateral meniscus and therefore it is more likely that tears occurs on the medial menisci.
Risk Factors[edit | edit source]
Possible risk factors for meniscal tears are sports, older age, male sex, and pre-existing pathologies such as osteoarthritis.[13] Additional risk factors are being overweight, intensive training, reduced muscle strength, varus or valgus deformity of the lower leg. Lesions in the meniscus can also increase the risk factor of developing knee osteoarthritis (OA).[14]
Differential Diagnosis [edit | edit source]
An examination of the knee and possible arthroscopy provides a clear classification of meniscus injuries. The size and severity of the meniscus tear or rupture are often indicative for the recovery after surgery and for eventual later degenerative phenomena in the knee joint.
When we speak about a meniscus tear, we must specify what type of injuries we are dealing with. The examination of the knee and any arthroscopy provides a clear classification of meniscal lesions. The extent and severity of the meniscus tear are often indicative of the recovery after the procedure and for any subsequent degenerative symptoms in the knee joint. The classification of meniscal tears can be done according to anatomic abnormality. There are different kind of tears in the meniscus like Tear length, tear depth and tear pattern. We will discuss the different injuries below.
- Tear length - injuries of the meniscus that only occur on the surface of our meniscus.
- Tear depth - a complete meniscal tear describes a tear runs through both superior and inferior surfaces, whereas a partial tear comprises only one surface. Longitudinal injuries are often full cracks; this means that the full thickness of the meniscus is affected. Frequently, when we support our bodyweight the pressure on the meniscus with the femur will push the crack open.
- Tear pattern Tear pattern included seven different lesions of the meniscus. [15] [16]
- Longitudinal/vertical tear - This type of tear can be anywhere along the meniscus. If this tear extends it may result in a bucket-handle tear. The ‘handle’ or ‘bucket-handle’ tears run across nearly the entire length of the meniscus. This often causes the formation of a flap that can get caught between the intercondylar space.[17]
- Horizontal tear or horizontal slit - Often forms part of more complex cracks, which consist of more of the above. This tears begin at the inner edge of the meniscus and continue against the capsule.[18]
- Flap tear - There are two types of flap tears, a horizontal and a vertical. The horizontal flap tear is the same as the horizontal tear but with complications. When you have a horizontal flap tear the inferior and superior surface of the meniscus can be uninjured, which is not the case with a vertical flap tear.
- Complex tear - These are patterns that describe tears in different planes and are seen in the degenerative meniscus.
- Discoid meniscus - This type of tear usually occurs on the lateral side of the meniscus. and is classified as either
- incomplete discoid, this is larger than a normal meniscus and is normally attached.
- complete discoid will cover the entire tibial plateau and is also normally attached.
- default in the posterior attachment at the capsule. This type is also more often symptomatic than the other two types of discoid meniscus.
- Angled tear - Usually occurs at the height of the front or superior horn.
- Radial tear - This begins at the inner edge of the meniscus and continues to the capsule. The radial cracks typically occur in the middle part of the meniscus. A radial tear of the lateral meniscus is often found together with an anterior-cruciate ligament tear. This tears can worsen. [19]
With a meniscus tear as a result of a sports accident, one must give attention to the high frequency of associated anterior-cruciate ligament tears (about 60% associated anterior-cruciate ligament tear). There are also so-called silent meniscus tears; this is a radial tear in the lateral meniscus tear. In many cases one does not recognize acute trauma as the mechanical complaints are absent or only slightly present. In many cases, these are pain during and after sports activities although there be pain at the level of the lateral joint line when pressure is applied, and in certain cases a limited flexion, especially in squat, as well as a painful hyper flexion-rotation test.
Different types of meniscus ruptures:[edit | edit source]
- Radial rupture
- Oblique rupture
- Longitudinal rupture
- Bucket handle
- Horizontal rupture
- Complex rupture
Diagnostic Procedures [edit | edit source]
Degenerative meniscal lesions are often found during MRI (magnetic resonance imaging) or in osteoarthritic knees during arthroscopic procedures. [20]
Traumatic Meniscal Lesions
The diagnosis of anterior knee instability is based on the physical examination and a positive Lachman test. It is extremely important to establish the correct diagnosis, because treatment of a meniscal tear and treatment of instability influence each other.[21]
Degenerative Meniscal Lesions
The prevalence of abnormal meniscal MRI images suggestive of existent lesions should be emphasized, but not be over-interpreted as meniscal tears or as an indication for surgical treatment when they reflect the natural changes related to the ageing of meniscal tissue. Two important questions the examiner needs to answer "are the symptoms related to meniscal problems" and "what is the condition of the articular cartilage?" [21]
Arthroscopy
This procedure allows the doctor to make a thin incision into the knee into which he inserts a camera with a light attached to see directly inside the joint allowing to see any damage and to make a definite diagnosis and an informed decision on management options.
MRI scan
Magnetic Resonance Imaging is the most extensive imaging assessment of the knee and it is also cost effective and can aid in prognosis and further treatment options when it is performed early after injury. [22] [23]
There are 3 orthogonal planes: [24]
- Saggital plane
- Coronal plane
- Transverse plane
CT-scan
Computed tomography is generally reserved for diagnosis of suspected fractures or assessment of complex fractures, although associated ligamentous injuries can be observable on CT scans intended for evaluation of osseous injuries. [24]
Outcome Measures[edit | edit source]
There are many outcome measures for this condition. Here are a few examples; [25] [26] [27]
- Cincinnati Knee Rating System
- Knee Injury and Osteoarthritis Outcome Score (KOOS)
- Lysholm Knee Score
- The Kujala Anterior Knee Pain Scale
- The International Knee Documentation Committee (IKDC)
- The Western Ontario Meniscal Evaluation Tool (WOMET)
- Numeric Rating Scale for pain (NRS)
- Visual Analogue Scale for pain (VAS)
Examination[edit | edit source]
Physical examination should be preceded by careful history taking, this can help the examiner choose the appropriate clinical tests to include in the physical examination. During physical examination, the affected and unaffected legs are compared with qualitative and quantitative findings. A thorough investigation is necessary when there’s a history of sudden pain on hyperflexion of the knee, catching, mechanical locking, and recurrent effusions.[27] Physical examination should include inspection, palpation, range of motion (ROM) and gait, and tests for integrity of menisci and other structures of the knee joint.[27]
Inspection[28]
- Height and weight of patient;
- Alignment of the knee joint;
- Effusion, scars or incisions? Check the state of healing;
- Muscle atrophy;
- Assessment of the skin and muscle tone (abrasions, lacerations, ecchymosis, erythema.
Palpation [27]
- Pain/tenderness or discomfort is reproduced by palpation of the joint line.
- Performing the fluid shift test and evaluate the presence of fluctuation to assess effusion which does not confirm the presence or absence of a meniscal lesion.
Joint line tenderness video provided by Clinically Relevant
ROM and Gait [27]
- Active and passive range of motion.
- Difficulties by full extension of the knee.
- Pain by full flexion of the knee or impossibility to flex the knee fully.
- Deviations or compensations of the gait pattern (antalgic gait).
Clinical Tests[edit | edit source]
In the clinical setting, provocative maneuvers that cause compression of meniscal fragments between the tibia and femur will often lead to pain. Thus, pain with varus stress may suggest medial meniscal injury. This concept is supported by maneuvers such as the Payr and Bohler tests, in the former maneuver, the patient sits cross-legged placing a stress on the medial meniscus, and in the latter, a simple varus and valgus stress elicits pain with compression of the meniscus. It is further suggested through more modern tests in which weightbearing is incorporated into rotatory movements, such as in the Thessaly test. However, when the meniscal fragment is flipped and interposed between the deep fibers of the MCL and the tibia, valgus stress will lead to compression of the fragment between these structures and medial pain.
McMurray Test [29]
- The McMurray test is performed with the patient supine. The examiner stands on the side of the affected knee and places one hand on the heel and the other one with the thumb on the medial aspect of the knee and the other fingers on the lateral part of the knee to stabilize, providing a valgus force. The knee is extended from full flexion to 90° of flexion first, while applying a varus force and rotating the tibia internally and externally.
- The test is considered positive if it causes pain or popping. Pain or popping by internal rotation suggests the presence of a lateral meniscus injury and by external rotation the presence of a medial meniscus injury.
McMurray Test video provided by Clinically Relevant
Apley Grind Test [30]
- The Apley grind test includes a set of provocative maneuvers. It is performed with the patient in prone position with the affected knee flexed to 90°. The tibia is compressed into the distal femur and rotated externally to evaluate the medial meniscus and internally to evaluate the lateral meniscus.
- The thigh is stabilized against the examining table. With the knee flexed to 90°, a distraction force is applied to the lower leg and an external rotation force is again applied.
- Examiner should note if pain is provoked with external rotation and distraction and if there is more pain than without distraction.
- The test is considered positive if it causes pain. But the pain must be less severe or relieved when the maneuver is repeated with distraction.
Apley's Test video provided by Clinically Relevant
Thessaly Test [31]
- The Thessaly test is performed with the patient standing with all weight on one extremity. The foot is planted and knee is flexed at 5° at first and then at 20°. The patient is then asked to internally and externally rotate the body, while holding the examiner’s hand for support. This test combines axial load and rotational forces.
- The test is considered positive by pain.
Thessaly Test video provided by Clinically Relevant
The clinical diagnosis of meniscal tears has been found to be more accurate when the tests are combined. Because some have low diagnostic accuracy when preformed in isolation; when they are combined, they are able to lift sensitivity and specificity. [32]
Medical Management[edit | edit source]
Conservative treatment is rarely successful for treating meniscal tears in young athletes and repair of the torn menisci is often required (LoE: 5) [47][33] Repair of a meniscal lesion should be strongly considered if the tear is peripheral and longitudinal, with concurrent Anterior Cruciate Ligament (ACL) reconstruction, and in younger patients. The probability of healing is decreased in complex or degenerative tears, central tears, and tears in unstable knees. Numerous repair techniques are available. Preservation of meniscal tissue is recommended, regardless of age - in active patients- whenever possible. (LoE: 3a)[48][34]
Another consideration is whether the meniscal repair or meniscectomy is appropriate. If none of the normal surgical treatments seems appropriate total meniscectomy is the last option. The factors that should have been taken in consideration while making decisions should be:
- The clinical evaluation
- Related lesions
- The exact type, location, and extent of the meniscal tear.[35]
Operative:[edit | edit source]
Arthroscopy is a small surgery. They look through a thin tube into the knee joint. The procedure can be performed to obtain information of the knee joint. In many cases, there can during the arthroscopy immediate a treatment be given. It’s possible that a larger operation is necessary.[36][37] You can find more information about arthroscopy at the page Meniscal Repair.
Certain meniscal tears like the bucket –handle rupture require operative treatment to prevent worsening of the rupture, to minimize additional damage to the torn portion of the meniscus and to optimize healing.
There are different kinds of operative treatment for meniscal tears as repair and partial resection.
If a rupture can’t be treated and it involves a large portion of the meniscus, or when repair failed, a significant portion of the meniscus must sometimes be removed. To avoid secondary osteoarthritis and reducing pain, meniscal transplantation may be the best solution.[38]
Meniscal allograft transplantation (MAT) is now considered an effective method of biologically reconstructing symptomatic, meniscectomized knees.[39]
For further reading see Meniscal Repair
Physiotherapy Management[edit | edit source]
Not all meniscal lesions require surgery, conservative treatment is another option. In the treatment regimen we recognize conservative means, arthroscopic resection or a meniscal suture.[40] Physiotherapy is one example of conservative treatment; it focuses on strengthening of the quadriceps muscle to prevent secondary quadriceps atrophy. This treatment is most successful with an incomplete tear or a small stable tear in the zone with blood supply. A meniscus tear that shows few, irregular symptoms, will initially be treated conservatively.
Exercise therapy has been suggested to be an effective treatment option for patients with knee degeneration. The aim of treatment is to improve knee function and limit joint pain. There is strong evidence that physical training plays an important role in reducing symptoms, improving muscle strength and physical ability.[41]
Acute Management[edit | edit source]
The physical therapy consists mainly of RICE (Rest, Ice, Compression, Elevation) when surgery isn’t necessary.
RICE is very important in the first 24 hours after an acute soft tissue injury. Especially when there are damaged blood vessels. It helps to reduce pain and swelling.[42]
Cryotherapy, also known as ice application, is a method in which the body is contacted with a medium with a lower temperature. Applying a cold source would decrease the temperature of the tissues. It causes superficial vasoconstriction and a decrease of the local blood flow.[43] How long, how often? This is the point where few people agree. The most common recommendation is to apply ice for 20 minutes every 2 hours for the first 48 to 72 hours. You must take into account that some people are more sensitive to cold than others are.
Rehabilitation (Conservative treatments)[edit | edit source]
Strengthening and stretch exercises for quadriceps and hamstrings are important.
The method of advancing strength depends on the timing of the rehabilitation program but also on the patient response, availability of equipment and the rehabilitation clinician’s preference.[43]
Strength Exercises[edit | edit source]
Isometric exercises for strengthening the quadriceps
- Quad set: With patient supine, uninvolved knee flexed and involved knee straight. The patient tries to push the knee down on the table
- Straight-leg raise
Isometric exercises for strengthening the hamstrings
- Hamstrings sets: The patient supine, uninvolved knee straight and involved knee in partial flexion.
- Pushing heel into the table or pillow.
Non-weight-bearing isotonic exercises
- Short-arc quad exercise: also called terminal knee extensions.
- Full-arc quad exercise
- Hamstring curls
Weight-bearing resistive exercises (When the patient is able to carry weight on the injured knee)
- Reciprocal training: training on a stationary bike.
- Platform leg press, wall squats, plié, lunge, step-up, step-down, lateral step-ups.
Flexibility Exercises[edit | edit source]
Flexibility exercises and joint mobilization are techniques improve the range of motion and the flexibility.[43]
These exercises can be active or passive. The techniques used depend on the type of tissue.
Prolonged extension stretch is used to increase knee extension. This exercise can be performed in two positions, prone or long sitting. Prolonged flexion stretch is an exercise for increasing flexion in the knee. The position used for this exercise depends on how the flexion movement is present.
Active stretches for quadriceps and hamstrings are also important.
Joint Mobilizations[edit | edit source]
Reduced joint mobility could be the result of injury, edema, surgery and immobilization. If this develops it can refer pain to the knee and even effect ankle mobility.
Joint mobilization is important for the following joints:
• Superior Tibiofibular joint;
• Patellofemoral joint. Patellar mobility is necessary for full flexion- extension motion for the knee;
• Tibiofemoral joint. It’s the most often mobilized joint to improve range of motion in the knee.
Balance & Agility[edit | edit source]
Balance and agility exercises begin with double-support weight-bearing activities and progress to single-limb static balancing on a stable surface.[43]
Post-Surgical Care[edit | edit source]
If surgery is necessary there are two options: a meniscus repair, or a meniscectomy (partial or full).
After surgery, expect for your patient to be on crutches for at least three weeks. Full recovery, using a comprehensive rehabilitation program will generally take between 3-4 months, and athletes involved in high level sports can be back on the field around 6-8 months post-operative (always verify this with the surgeon, and the particular protocol you are following). This timeline does not take into account if other structures (e.g. the ACL), are also involved.
Needless to say, the rehabilitation of a meniscus repair after surgery depends on the size of the operation. The operation and the following rehabilitation plan need to be individualised.
It has been suggested that non-structured rehabilitation after a meniscal repair is safe, but can entail increased failure rates compared to well-structured and evidence-based rehabilitation. [16]
Overall take-home clinical considerations[edit | edit source]
- Control the pain and inflammation - Cryotherapy, analgaesics, NSAIDs.
- To regain good knee control.[41]
- Restore ROM (Range of motion) [41]
- ROM exercises within any limits in range that the consultant has requested[44]
- Restore the flexibility[41]
- Restore muscle function[41]
- specific strengthening exercises including quadriceps (A medial meniscus lesion influences the strength of the M. Vastus medialis. [45], hamstrings, calf, hip. The exercise program should consist of both concentric and eccentric exercises to receive muscular hypertrophy as well as neuromuscular function. [41]
- Optimize neuromuscular coordination - proprioceptive re-education[46]
- Progress weight-bearing and joint stress are necessary to enhance the functionality of the meniscal repair so should be progressed as indicated by the consultant. Excessive shear forces may be disruptive and should be avoided initially.
For further discussion on physiotherapy management see Meniscal Repair
Clinical Bottom Line[edit | edit source]
- The meniscus is quite often damaged by intensive sports like football, it often occurs due to a twisting injury on a semi-flexed limb through a weight bearing knee.
- The surgical approach to meniscal tears is typically determined by the type of the tear in conjuction with the tear location, patient age, and chronicity of the tear.[47]
- Surgery isn’t necessary when meniscus teas are stable and relatively small and is located in a well-perfused region. These can be treated with physical therapy.
- However, surgery is necessary if it affects tears that are unstable and large located on the non-perfused inside of the meniscus. Usually surgeons have to remove the torn part of the meniscus, this is called a partial meniscectomy. The orthopedic surgeon tries to remove as little as possible so that the meniscus keeps its shock absorption effect. Very occasionally the tear in the meniscus can be sutured. Complete removal of the meniscus is justified only when it is irreparably torn, and the meniscal rim should be preserved if at all possible.[48]
References [edit | edit source]
- ↑ Knieslijtage, http://www.knie-slijtage.nl/knie-aandoeningen/meniscus/wat-is-een-meniscusscheur, geraadpleegd on 26 November 2011 ( level of evidence: no references)
- ↑ 2.0 2.1 2.2 Hede, A., Jens|n, D. B., Blyme, P., & Sonne-Holm, S. (1990). Epidemiology of meniscal lesions in the knee: 1,215 open operations in Copenhagen 1982-84.Acta orthopaedica Scandinavica. 1990; 61(5): 435-437.
- ↑ Alvin Shieh, Meniscus tear patterns in relation to skeletal immaturity: children versus adolescents. The American Journal of Sports Medicine. 2013; Sep 26.
- ↑ 4.0 4.1 Zanetti M, Pfirrmann CW, Schmid MR, Romero J, Seifert B, Hodler J. Patients with suspected meniscal tears: prevalence of abnormalities seen on MRI of 100 symptomatic and 100 contralateral asymptomatic knees. AJR Am J Roentgenol 2003; 181:635–641
- ↑ Wang, Dean, et al. "Patient-reported outcome measures for the knee. Journal of knee surgery. March 2010: 137-151
- ↑ Denti, Matteo, et al. "Traumatic Meniscal Lesions. Surgery of the Meniscus. Springer Berlin Heidelberg, 2016; 67-78.
- ↑ Raunest J, Hotzinger H, Burrig KF. Magnetic resonance imaging (MRI) and arthroscopy in the detection of meniscal degenerations: correlation of arthroscopy and MRI with histology findings. Arthroscopy 1994; 10: 634–640
- ↑ ID McDermott, SD Masouros, AMJ Bull, and AA Amis. The Meniscus, 2010; 91(9.6), 11.
- ↑ 9.0 9.1 Nelson EW, LaPrade RF. The anterior intermeniscal ligament of the knee. An anatomic study. Am J Sports Med. 2000; 28:74–76
- ↑ Andrews JR, Norwood LA Jr, Cross MJ. The double bucket handle tear of the medial meniscus. Am J Sports Med. 1975; 3:232–237
- ↑ Akseki D, Ozcan O, Boya H, Pinar H. A new weight bearing meniscal test and a comparison with McMurray’s test and joint line tenderness. Arthroscopy. 2004;20:951–958. Level of evidence 2B
- ↑ Lee, Dwong Won., et al., Medial Meniscus Posterior Root Tear: A Comprehensive Review, Knee surgery and related research, 2014. Level of Evidence: 3A
- ↑ Goossens, Pjotr, et al. "Validity of the Thessaly test in evaluating meniscal tears compared with arthroscopy: a diagnostic accuracy study." journal of orthopaedic & sports physical therapy 45.1 (2015): 18-24. Level of evidence 2A.
- ↑ Sigurdsson U, Delayed gadolinium-enhanced MRI of meniscus (dGEMRIM) and cartilage (dGEMRIC) in healthy knees and in knees with different stages of meniscus pathology, BMC Musculoskelet Disord. 2016; Sep 29.
- ↑ Miller RH III. Knee injuries. In: Canale ST (ed) Campbell’s operative orthopaedics. St Louis: Mosby Elsevier, 2003
- ↑ Milne JC, Marder RA. Meniscus tears. In: Chapman MW (ed) Chapman’s orthopaedic surgery. Philadelphia; Lippincott Williams & Wilkins, 2001
- ↑ Rubin DA, Kneeland JB, Listerud J et al. MR diagnosis of meniscal tears of the knee: value of fast spin-echo vs con- ventional spin-echo pulse sequences. AJR Am J Roentgenol. 1994; 162:1131–1135
- ↑ . Burk DL Jr, Dalinka MK, Kanal E et al. Meniscal and ganglion cysts of the knee: MR evaluation. AJR Am J Roentgenol. 1988; 150:331–336
- ↑ Tuckman GA, Miller WJ, Remo JW et al. Radial tears of the menisci: MR findings. AJR Am Roentgenol. 1994; 163: 395–400
- ↑ Noble J, Hamblen DL (1975) The pathology of the degenerate meniscus lesion. J Bone Joint Surg Br. 1975; 57:180–186
- ↑ 21.0 21.1 Denti, Matteo, et al. Traumatic Meniscal Lesions. Surgery of the Meniscus: pages 67-78. Heidelberg; Springer Berlin, 2016.
- ↑ Oei EH, Nikken JJ, Ginai AZ, et al. Costs and effectiveness of a brief MRI examination of patients with acute knee injury. Eur Radiol 2009;19(2):409–418. CrossRef, Medline
- ↑ Oei EH, Nikken JJ, Ginai AZ, et al. Acute knee trauma: value of a short dedicated extremity MR imaging examination for prediction of subsequent treatment. Radiology 2005;234(1):125–133
- ↑ 24.0 24.1 Naraghi AM, White LM. Imaging of Athletic Injuries of Knee Ligaments and Menisci: Sports Imaging Series.Radiology 2016; 281.1: 23-40.
- ↑ Wang, Dean, et al. Patient-reported outcome measures for the knee. Journal of knee surgery. 2010; 23.03: 137-151.
- ↑ Sihvonen, Raine, et al. Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. New England Journal of Medicine, 2013; 369.26: 2515-2524.
- ↑ 27.0 27.1 27.2 27.3 27.4 Collins,Natalie J., et al., Measures of Knee Function, National Intitution of Health (2011)
- ↑ Hoppenfeld S. Physical examination of the spine & extremities. Upper Saddle River, NJ: Prentice Hall; 1976.
- ↑ McMurray TP. The semilunar cartilages. Br J Surg. 1942;2(116):407–14.
- ↑ Apley AG. The diagnosis of meniscus injuries: some new clinical methods. J Bone Joint Surg. 1947;29(1): 78–84.
- ↑ Karachalios T, Hantes M, Zibis AH, Zachos V, Karantanas AH, Malizos KN. Diagnostic accuracy of a new clinical test (the Thessaly test) for early detection of meniscal tears. J Bone Joint Surg. 2005;87(5): 955–62.
- ↑ Herschmiller T.A et al. The Trapped Medial Meniscus Tear: An Examination Maneuver Helps Predict Arthroscopic Findings; OJSM 2015
- ↑ Poulsen MR, Johnson DL. Meniscal injuries in the young, athletically active patient. fckLRDepartment of Orthopaedic Sugery, University of Kentucky, Lexington, KY. Abstract.
- ↑ Heckmann TP, Barber-Westin SD, Noyes FR. Meniscal repair and transplantation: indications, techniques, rehabilitation, and clinical outcome. J Orthop Sports Phys Ther. 2006 Oct;36(10):795 814.
- ↑ DeHaven Ke. Decision-making factors in the treatment of meniscus lesions. Clinical Orthopedics & Related Research 1990; (252) 49-54
- ↑ OPERATIE,http://www.chirurgenoperatie.nl/pagina/traumatologie/arthroscopie_knie.php, geraadpleegd op 24 november 2011 ( level of evidence: 5)
- ↑ Anderson et al. Interobserver Reliability of the International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine (ISAKOS) Classification of Meniscal Tears. The American Journal of Sports Medicine. 2011; Vol 39(5): 926-932. Level of evidence 1B
- ↑ Abat F, Gelber PE, Erquicia JI, Tey M, Gonzalez-Lucena G, Monllau JC. Prospective comparative study between two different fixation techniques in meniscal allograft transplantation. Knee Surg Sports Traumatol Arthrosc. 2013;21(7):1516-1522. Level of evidence 2B
- ↑ Lee et al. Proper Cartilage Status for Meniscal Allograft Transplantation Cannot Be Accurately Determined by Patient Symptoms. The American Journal of Sports Medicine 2016; Vol 44(3): 646-651 Level of evidence 3B
- ↑ Deyle GD, Henderson NE, Matekel RL, Ryder MG, Garber MB, Allison SC. Effectiveness of manual physical therapy and exercise in osteoarthritis of the knee. A randomized, controlled trial. Ann Intern Med. 2000; 132:173–181
- ↑ 41.0 41.1 41.2 41.3 41.4 41.5 Vervest AMJS, et al : Effectiveness of physiotherapy after meniscectomy; knee surg,sports traumatol, arthrosc. 1999 7: 360-364
- ↑ THE STRETCHING INSTITUTE, http://www.thestretchinghandbook.com/archives/meniscus-tear.php, geraadpleegd op 20 november 2011 (level of evidence: 5)
- ↑ 43.0 43.1 43.2 43.3 Houglum, P.A. Therapeutic Exercise for Musculoskeletal Injuries. 2005 (level of evidence: 5)
- ↑ Brent M,C.D, et al. Effect of early active range of motion rehabilitation on outcome measures after partial meniscectomy. Knee Surg Sports Traumatol Arthrosc. 2009; 17: 607-616
- ↑ Sylvia H, maria H, Et; Arthroscopic or conservative treatment of degenerative medial meniscal tears a prospective randomised trial: Knee Surg Sports Traumatol Arthrosc. 2007; 15: 393-401
- ↑ Zhang, Xiaohui, et al. "Effects of strength and neuromuscular training on functional performance in athletes after partial medial meniscectomy." Journal of exercise rehabilitation 13.1 (2017): 110.
- ↑ Shieh, A. Meniscus tear patterns in relation to skeletal immaturity: children versus adolescents, the American Journal of Sports Medicine, 2013 Sep 26.
- ↑ Ho Yoon, K. et al., Meniscal Repair, Knee Surg Relat Res., 2014 Jun, 68-76.