Friction and its Application
Introduction[edit | edit source]
Friction plays a significant role in physiotherapy, especially in manual therapy techniques and therapeutic exercises. Friction, which is normally taken as a hindrance in everyday life, holds an important role in physiotherapy. It serves as a fundamental concept guiding movement mechanics, exercise selection, and injury prevention strategies.
What is Friction?[edit | edit source]
Friction is the opposing force that occurs between surfaces in contact and parallel to each other. In our body, it manifests in various scenarios, such as the interaction between joint surfaces, the contact between skin and supportive equipment, or the interface between the body and external surfaces during movement.[1]
Laws Governing Friction[edit | edit source]
The laws governing friction are [1]:
- Type of the Surface: Friction depends on the nature of the surfaces in contact, whether rough or smooth.
- Opposition to Motion: Frictional force acts to oppose the motion, serving as a stabilizing force during movement.
- Relative Velocity: The frictional force varies with the relative velocity between surfaces.
- Surface Area: Friction is independent of the surface area of contact between the surfaces
- Reaction Force: The frictional force is proportional to the reaction force pressing the surfaces together.
Friction in the Human Body[edit | edit source]
Friction is the force that opposes the direction of motion. It can be classified into two types of friction:
- static: static friction exists when objects are at rest
- kinetic: when objects move against each other, there is kinetic friction. Static friction tends to be greater than kinetic friction.
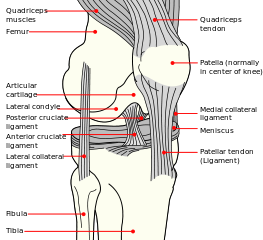
In the knee joint[1], the friction exists between the femoral component and the tibial condyles. The synovial fluid acts as lubricant. Muscles generates force to move the leg, which must be balanced with the frictional force that opposes the tendency of the movement at the knee. Leg remains stationary when the frictional force is equivalent to the horizontal pushing force exerted at the knee joint. But once the pushing force is greater than the frictional force as the body begins to move, the leg will change in position.
Coefficient of friction[edit | edit source]
The coefficient of friction is the ratio of frictional force to normal force that maintains surfaces together.
- Coefficient of friction= Friction/Normal Force, represented by the Greek letter= μ.
- (μ = f/N), For a body that is static, the normal force is the weight of the block.
Every material has its own coefficients of static and kinetic frictions. Coefficients of friction are always positive and most tend to range from 0 to 1.[2] Research suggests friction coefficients in synovial joints ranges from 0.014 to 0.024 in cadaveric human ankle joint, with 0.02 in cadaveric hip joint[3]. It is influenced by change in temperature, the magnitude of the normal force, and speed. Lower coefficients of friction suggest that things slide off the material easily and higher coefficients of friction indicate that things don't glide easily.
Factors Affecting Friction[edit | edit source]
Friction in the human joints is influenced by[1]:
- Synovial fluid: the synovial membrane produces synovial fluid, which is a hydrodynamic fluid that acts as grease or oil in bodily joints where tissues move over one another, such as the wrist, fingers, ankles, toes, and knees.
- Bony Surfaces: The carpals and tarsals act as rollers or ball bearings similar to an axle in a wheel, in the knee joint.
- Articular Cartilage: promotes the formation of fluid films and this reduces friction markedly.
- Meniscus: removal of the meniscus in the medial compartment of the knee leads to the elevation of the friction force.[4]
Lubrication[edit | edit source]
Lubrication affects the friction between the articular surfaces.[3]
- The synovial fluid and formation of fluid films (by articular cartilage) reduces friction markedly.
- Another friction-reduction mechanism is biphasic lubrication in articular cartilage, which consists of both fluid and solid phases. Fluid phase: Immediately after loading, the fluid inside cartilage becomes compressed immediately after loading, causing the fluid to bear the majority of the strain, thereby reducing friction. Solid Phase: As time passes, the weight is shifted to the solid phase, and friction rises. Under sustained stress, boundary lubrication acts as an efficient method for limiting friction in synovial joints.
- Other lubrication mechanisms is a “surface amorphous layer”, also described as “gel layer”, “hydration layer”, or “brush layer”, in which the chondroitin- or keratan sulphates constituting the leaves of the proteoglycan subunit are hydrated.
- Effect of HA on the joint lubrication[5]: HA provides lubrication and thereby decreases wear and tear. Administering HA injections to affected joints is shown to enhance mobility and alleviate pain and inflammation. According to study evaluating the effect of applying different molecular weights of HA to abraded articular cartilage in porcine TMJ, joint friction increased by about 350% following experimental scouring of the cartilage surface and impairment of synovial lubrication and HA application to the eroded cartilage surfaces reduced the frictional coefficient by approximately 50%.
Meniscus[edit | edit source]
The meniscus is crucial for knee joint function and disease progression, including osteoarthritis[3]. Studies in bovine knee joints have showed that the removal of the meniscus considerably raised the friction coefficient between the cartilage surfaces from 0.02 to 0.05 due to the increased contact pressure.
Fat pads[edit | edit source]
Fat pads[3] play an important role in reducing friction in the musculo-skeletal system. These are masses of encapsulated adipose tissue, strategically located to provide mechanical advantage to the musculo-skeletal system. It consist of water, collagens and proteoglycans as the extracellular matrix, and numerous unilocular adipocytes (fat cells) that are swollen with lipid. Under adverse conditions, high friction may lead to abnormity and consequently pain. Read more about Fat Pad Syndrome, common source of Anterior Knee Pain; also called Hoffa's disease, fat pad syndrome or hoffitis that is caused by patella maltracking resulting in the impingement of the superolateral aspect of Hoffa's fat pad between the inferior patella and the lateral femoral condyle.
Tendons[edit | edit source]
Tendons are either subjected to either tension or compression. High friction in tendon is linked with cumulative trauma disorders such as [Carpal Tunnel Syndrome]] and tendonitis as well as tendon suturing failure. [3]
Bursae[edit | edit source]
Bursae contain a lubricating fluid that serves to reduce friction between structures. Subcutaneous bursae prevent friction between the skin and an underlying bone, submuscular bursae protect muscles from rubbing against a bone or another muscle, and a subtendinous bursa prevents friction between bone and a muscle tendon.
Artificial Joint Surfaces[edit | edit source]
Skin[edit | edit source]
Ulcer formation are also closely related to skin friction. Skin friction depends on anatomical site and skin hydration. Prolonged pressure on the skin surface, particularly on the heel, along with friction and shear, contributes to the development of pressure ulcers.[3]
External Surfaces (walkway/shoe contact)[edit | edit source]
When walking on any surface, the relationship between the friction required by the person for the action performed (required friction) and the friction available at the walkway/shoe contact (available friction) is critical. As long as the available friction exceeds the required friction, the person will not fall or slip. Required friction differs in various gaits, e.g. level walking, load carrying, walking up ramps in order to prevent fall. Biomechanical analysis of gait is valuable tool for setting of available friction thresholds to determine whether or not a shoe, walkway surface, or combination of the two will or will not be slip resistant thereby assisting in the reducing of slip-induced fall accidents.[3] Maximum coefficient of friction required occurs at the heel strike and the propulsion phase. Falls or slips happen when the friction between shoe-floor surfaces is lower. It has been proposed that fiction coefficients below 0.24, above 0.36, and within the range of 0.24 to 0.36 correlate to dangerous, safe, and moderately risky situations, respectively. Other influencing factors are age, weight, body shape, surface, dry/wet condition and footwear characteristics.
Applications of Friction in Rehabilitation[edit | edit source]
Frictional effects play a crucial role in various aspects of rehabilitation:[1]
Supportive Equipment:[edit | edit source]
The selection of supportive equipment, such as crutches or walking aids with rubber tips, relies on the high coefficient of friction provided by rubber against ground surfaces.
Joint Functionality[edit | edit source]
Understanding the role of synovial fluid and joint mechanics helps in maintaining joint health and function, as synovial fluid serves as a lubricant to reduce friction between joint surfaces.
Skin Protection[edit | edit source]
Friction management is essential to prevent skin injuries, such as blistering, which may occur in areas of high friction during movement or prolonged pressure.
Attachments[edit | edit source]
Patients often have various attachments in the hospital setting, including electrocardiogram (ECG) leads, arterial and venous lines, central venous catheters, urinary catheters, pulse oximetry, and underwater sealed drains.
Friction arising from the contact of attachments directly results in shear stress that may damage the natural tissue and affect comfort. Care must be exercised while positioning and moving the patient to minimize the skin irritation.
Safety[edit | edit source]
Falls when entering or leaving a bath can pose a significant risk, especially for the elderly.
Exercise Design[edit | edit source]
Physiotherapists consider friction when designing exercises to enhance movement efficiency, reduce joint stress, and improve functional outcomes.
Soft Tissue and Joint Mobilisations[edit | edit source]
Frictional forces can be utilized to improve tissue and joint mobility and reduce stiffness.
Tissue flexibility[edit | edit source]
- Friction massage techniques to mobilize soft structures such a muscles, tendons, ligaments, fascia.[6] It involves applying pressure and rubbing movements directly to the affected area, aiming to break down adhesions, scar tissue, and muscle knots to improve tissue flexibility, reduce pain, and enhance circulation to promote healing.
- Cross-Fiber Friction Massage applied perpendicular to the direction of muscle fibers is commonly used to target specific areas of tissue dysfunction or to break down adhesions between muscle layers. Cross-fiber friction massage can help improve tissue mobility, reduce muscle stiffness, and alleviate pain.[7]
Scar Tissue Management[edit | edit source]
Scar tissue resulting post-surgery or post-injury may limit the range of motion and causing pain and dysfunction. Friction techniques, such as scar massage breaks down scar tissue adhesions and promotes tissue remodeling. By applying controlled friction to the scar tissue can help improve tissue mobility, reduce scar adhesions, and enhance overall function.[8]
Trigger Point Release[edit | edit source]
Friction can be applied to trigger points—hyperirritable spots within taut bands of skeletal muscle—to release muscle tension and alleviate pain. we may use their fingers, thumbs, or specialized tools to apply localized friction to trigger points, helping to deactivate them and restore muscle function.
Joint Mobilization:[edit | edit source]
Joint mobilization techniques improve joint mobility and reduce stiffness. Applying controlled friction to the joint surfaces can help in breaking down adhesions, increase synovial fluid circulation, and promote joint lubrication. This can restore normal joint mechanics and reduce pain and dysfunction.[9]
Taping Techniques:[edit | edit source]
Taping Techniques: such as kinesiology tape applying friction to the adhesive side of the tape activates its heat-sensitive properties, thereby improving its therapeutic effects, such as providing support, reducing swelling, and enhancing proprioception.[10]
Safety Precautions[edit | edit source]
While friction is essential for movement and stability, its excessive or inefficient application can lead to adverse effects[1]:
- Tissue Damage: Prolonged or excessive friction can cause the wearing and tearing of tissues, leading to pain, inflammation, and reduced mobility.
- Energy Consumption: Friction contributes to the use of energy during movement, leading to increased fatigue and potential overheating of tissues.
- Reduced Efficiency: Inefficient frictional interactions can impair movement efficiency, limiting the effectiveness of rehabilitation interventions.
Physiological effects of friction massage[edit | edit source]
- Increased vasodilation[11][12]-Vasodilation refers to the expansion of blood vessels. Friction applied to the skin raises the temperature in localized areas, prompting blood vessels to unwind and expand. This expanded vasodilation facilitates greater delivery of oxygen and nutrient-rich blood to the muscles.
- Improved recovery[13]
- Breakdown / realignment of collagen fibres[8] and scar tissue -Frictions play a role in breaking down and realigning collagen fibers, which are a type of connective tissue characterized by their tough texture and high strength. Scar tissue, predominantly composed of collagen fibers, can develop following injury. However, it may disrupt the normal alignment of muscle fibers, leading to restrictions in movement and subsequent pain. Frictions, a specialized massage technique, target these restrictive tissues, aiming to realign the fibers to their natural orientation.
- Increased range of movement[14] and elasticity-Frictions additionally enhance tissue elasticity. When performed along the direction of muscle fibers, frictions can stretch and lengthen the tissues. Moreover, frictions elevate the temperature, promoting greater mobility of the tissue fibers, and facilitating their manipulation and stretching. Augmenting elasticity is crucial for improving mobility and preventing tightness
Conclusion[edit | edit source]
Friction is essential for regular functioning and has the potential to aid in the creation of diagnostic and interventional medical devices. It also has potential in disease development in certain organs of the body. Increased friction along with increased contact stresses leads to degradation and wear of cartilage. [3] [4] Also, understanding the laws governing friction is essential for rehabilitation professionals to analyze movement patterns and design effective rehabilitation programs.
Reference[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Federal University of Technology, Owerri, & Tropical Publishers Nigeria. (2016). Human biomechanics: Basic and applied. Federal University of Technology, Owerri and Tropical Publishers Nigeria.https://www.researchgate.net/publication/357152541_Human_Biomechanics_Basic_and_Applied
- ↑ Friction - Friction Coefficients and Calculator. Accessed from https://www.engineeringtoolbox.com/friction-coefficients-d_778.html on 23/4/24
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 Jin Z, Dowson D. Bio-friction. Friction. 2013 Jun;1:100-13.
- ↑ 4.0 4.1 McCann L, Ingham E, Jin Z, Fisher J. Influence of the meniscus on friction and degradation of cartilage in the natural knee joint. Osteoarthritis and Cartilage. 2009 Aug 1;17(8):995-1000.
- ↑ Tanaka E, Iwabe T, Dalla-Bona DA, Kawai N, van Eijden T, Tanaka M, Kitagawa S, Takata T, Tanne K. The effect of experimental cartilage damage and impairment and restoration of synovial lubrication on friction in the temporomandibular joint. Journal of orofacial pain. 2005 Oct 1;19(4).
- ↑ Chaves P, Simões D, Paço M, Pinho F, Duarte JA, Ribeiro F. Cyriax's deep friction massage application parameters: Evidence from a cross-sectional study with physiotherapists.Musculoskeletal Science and Practice. 2017 Dec 1;32:92-7.
- ↑ Rasool F, Memon AR, Kiyani MM, Sajjad AG. The effect of deep cross friction massage on spasticity of children with cerebral palsy: A double-blind randomised controlled trial. J Pak Med Assoc. 2017;67:87.https://www.researchgate.net/profile/Aamir-Memon-3/publication/311775535_The_effect_of_deep_cross_friction_massage_on_spasticity_of_children_with_cerebral_palsy_A_double-blind_randomised_controlled_trial/links/585a6b6308aeabd9a58ca55e/The-effect-of-deep-cross-friction-massage-on-spasticity-of-children-with-cerebral-palsy-A-double-blind-randomised-controlled-trial.pdf
- ↑ 8.0 8.1 Barnes SP, Ma Y, Patel B, Muthayya P. Efficacy of massage techniques for hypertrophic burn scars – A systematic review of the literature. J Burn Care Res. 2024;45(2):356-365. doi:10.1093/jbcr/irad140 https://academic.oup.com/jbcr/article-abstract/45/2/356/7270579
- ↑ Nor Azlin MN, Su Lyn K. Effects of passive joint mobilization on patients with knee osteoarthritis. Sains Malaysiana. 2011;40(12):1461-1465.http://www.ukm.edu.my/jsm/pdf_files/SM-PDF-40-12-2011/17%20Nor%20Azlin.pdf
- ↑ Mohamadi M, Piroozi S, Rashidi I, Hosseinifard S. Friction massage versus kinesiotaping for short-term management of latent trigger points in the upper trapezius: a randomized controlled trial. Chiropr Man Therap. 2017;25:25.https://link.springer.com/article/10.1186/s12998-017-0156-9
- ↑ Cambron JA, Dexheimer J, Coe P. Changes in blood pressure after various forms of therapeutic massage: A preliminary study. J Altern Complement Med. 2006;12:65–70.
- ↑ Holey E, Cook E. Evidence-Based Therapeutic Massage. A Practical Guide for Therapists. 2nd ed.Edinburgh: Churchill Livingstone; 2003
- ↑ Leivadi S, Hernandez-Reif M, Field T, et al. Massage therapy and relaxation effects on university dance students. J Dance Med Sci. 1999;3:108–112
- ↑ Hopper D, Deacon S, Das S, et al. Dynamic soft tissue mobilization increases hamstring flexibility in healthy male subjects. Br J Sports Med. 2004;39:594–598