Skeletal Metastases: Difference between revisions
No edit summary |
No edit summary |
||
| Line 7: | Line 7: | ||
== Introduction == | == Introduction == | ||
[[File:Bone_pic_haha.jpg|right|frameless]] | [[File:Bone_pic_haha.jpg|right|frameless]] | ||
Skeletal metastases (a cancer of the bone that has originated from another site) are common and result in significant morbidity in patients with metastatic disease.<ref>Radiopedia Skeletal matastases Available from: (last accessed 6.9.2020)https://radiopaedia.org/articles/skeletal-metastasis-1</ref> | Skeletal metastases (a [[Oncology|cancer]] of the bone that has originated from another site) are common and result in significant morbidity in patients with metastatic disease.<ref>Radiopedia Skeletal matastases Available from: (last accessed 6.9.2020)https://radiopaedia.org/articles/skeletal-metastasis-1</ref> | ||
* Bones are a common site for certain cancers such as breast cancer and prostate cancer. | * Bones are a common site for certain cancers such as [[Breast Cancer|breast cancer]] and [[Prostate Cancer|prostate cancer]]. | ||
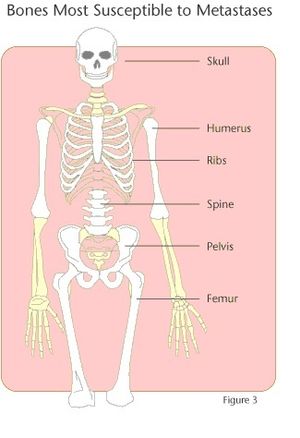
* The most common sites for skeletal metastases are the spine (this is the most common site), pelvis, femur, humerus, ribs, and | * The most common sites for skeletal metastases are the spine (this is the most common site), pelvis, femur, humerus, ribs, and [[Skull|skul]]<nowiki/>l. | ||
* The diagnosis is often straightforward, especially as in many cases there is a well-documented history of metastatic malignancy | * The diagnosis is often straightforward, especially as in many cases there is a well-documented history of metastatic malignancy | ||
* Sometimes they may mimic benign disease or other primary malignancies<ref name=":0">Radiopedia [https://radiopaedia.org/articles/skeletal-metastasis-1 Skeletal Metastases] Available from:https://radiopaedia.org/articles/skeletal-metastasis-1 (last accessed 6.9.2020)</ref> | * Sometimes they may mimic benign disease or other primary malignancies<ref name=":0">Radiopedia [https://radiopaedia.org/articles/skeletal-metastasis-1 Skeletal Metastases] Available from:https://radiopaedia.org/articles/skeletal-metastasis-1 (last accessed 6.9.2020)</ref> | ||
Despite recent advances in therapeutic approaches, bone metastases remain incurable and produce multiple complications called skeletal-related events, including hypercalcemia, pathological fractures, spinal compression, and bone pain, which are associated with poor prognosis<ref>Hiraga T. [https://www.sciencedirect.com/science/article/abs/pii/S1349007919300064 Bone metastasis]: Interaction between cancer cells and bone microenvironment. Journal of Oral Biosciences. 2019 Jun 1;61(2):95-8.Available from:https://www.sciencedirect.com/science/article/abs/pii/S1349007919300064 (last accessed 6.9.2020)</ref>. | Despite recent advances in therapeutic approaches, bone metastases remain incurable and produce multiple complications called skeletal-related events, including [[Hypercalcemia|hypercalcemia,]] [[Stress Fractures|pathological fractures]], [[Cauda Equina Syndrome|spinal]] compression, and [[bone]] pain, which are associated with poor prognosis<ref>Hiraga T. [https://www.sciencedirect.com/science/article/abs/pii/S1349007919300064 Bone metastasis]: Interaction between cancer cells and bone microenvironment. Journal of Oral Biosciences. 2019 Jun 1;61(2):95-8.Available from:https://www.sciencedirect.com/science/article/abs/pii/S1349007919300064 (last accessed 6.9.2020)</ref>. | ||
* Skeletal metastases usually occur in an advanced cancer. | * Skeletal metastases usually occur in an advanced cancer. | ||
* “Its prevalence is rising due to higher rate of diagnosis, better systemic treatment, longer lives with the disease and higher disease burden rate”.<ref name="Indian">Indian Journal of Orthopaedics. Management of skeletal metastases: An orthopaedic surgeon’s guide. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4292329/ (accessed 27 March 2017).</ref><br> | * “Its prevalence is rising due to higher rate of diagnosis, better systemic treatment, longer lives with the disease and higher disease burden rate”.<ref name="Indian">Indian Journal of Orthopaedics. Management of skeletal metastases: An orthopaedic surgeon’s guide. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4292329/ (accessed 27 March 2017).</ref><br> | ||
| Line 22: | Line 22: | ||
== Epidemiology == | == Epidemiology == | ||
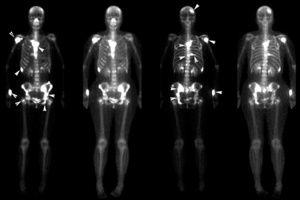
[[File:Bone scan.jpg|right|frameless]] | |||
Skeletal metastases account for 70% of all malignant bone tumours, and are seen in a vast number of primary cancers | Skeletal metastases account for 70% of all malignant bone tumours, and are seen in a vast number of primary cancers | ||
* Lung cancer, breast cancer, renal cell carcinoma and prostate cancer account for approximately 80% of all skeletal metastases. This is due to not only the propensity of these tumours to metastasise to bone, but also the fact that these are some of the most common tumours<ref name=":0" />. | * [[Lung Cancer|Lung cancer]], breast cancer, [[Renal Cancer|renal cell carcinoma]] and prostate cancer account for approximately 80% of all skeletal metastases. This is due to not only the propensity of these tumours to metastasise to bone, but also the fact that these are some of the most common tumours<ref name=":0" />. | ||
* Bone is the third most common site for metastatic cancer<ref name="Society">Society of Interventional Radiology. Nonsurgical Treatments for Metastatic Cancer in Bones. http://www.sirweb.org (accessed 26 March 2013).</ref> | * Bone is the third most common site for metastatic cancer<ref name="Society">Society of Interventional Radiology. Nonsurgical Treatments for Metastatic Cancer in Bones. http://www.sirweb.org (accessed 26 March 2013).</ref> | ||
*More than 2 out of 3 breast and prostate cancers that spread to other parts of the body spread to the bone<ref name="Society" /> | *More than 2 out of 3 breast and prostate cancers that spread to other parts of the body spread to the bone<ref name="Society" /> | ||
| Line 29: | Line 30: | ||
== Clinical Presentation == | == Clinical Presentation == | ||
The majority of metastases to bone are asymptomatic. Symptoms can arise in a number of scenarios | The majority of metastases to bone are asymptomatic. Symptoms can arise in a number of scenarios | ||
# Local bone pain - Pain usually is worse at night and may get better with movement, but can become constant and may be worse during activity.<ref name="ACS" />Pain is usually localized to the site of metastases, but can refer to areas around the site.<ref name="University">University of Michigan Comprehensive Cancer Center. Bone Metastases Symptoms. http://www.cancer.med.umich.edu/cancertreat/tissue_bone/bonesymptoms.shtml</ref> Pain usually increases to severe intensity. | # Local bone pain - [[Cancer Pain|Pain]] usually is worse at night and may get better with movement, but can become constant and may be worse during activity.<ref name="ACS" />Pain is usually localized to the site of metastases, but can refer to areas around the site.<ref name="University">University of Michigan Comprehensive Cancer Center. Bone Metastases Symptoms. http://www.cancer.med.umich.edu/cancertreat/tissue_bone/bonesymptoms.shtml</ref> Pain usually increases to severe intensity. | ||
2. Soft tissue mass resulting in: | 2. Soft tissue mass resulting in: | ||
* direct compression of adjacent structures by extraosseous soft tissue mass (e.g. cord compression) | * direct compression of adjacent structures by extraosseous soft tissue mass (e.g. cord compression) | ||
| Line 42: | Line 43: | ||
== Pathology == | == Pathology == | ||
The major route of spread of tumour to bone is haematogenous, although lymphatic spread is also seen | The major route of spread of tumour to bone is [[Blood Physiology|haematogenous]], although [[Lymphatic System|lymphatic]] spread is also seen | ||
Regardless of the route of spread, metastases lead to: | Regardless of the route of spread, metastases lead to: | ||
| Line 64: | Line 65: | ||
# Sclerotic metastases | # Sclerotic metastases | ||
# Mixed lytic and sclerotic metastases | # Mixed lytic and sclerotic metastases | ||
'''Plain radiograph''' | '''[[X-Rays|Plain radiograph]]''' | ||
* Skeletal metastases can be difficult to identify on plain films since extensive (30-50%) bone mineral loss is required before the density loss is radiographically-visible. | * Skeletal metastases can be difficult to identify on plain films since extensive (30-50%) bone mineral loss is required before the density loss is radiographically-visible. | ||
* In many other cases the lesion is visible due to destruction of cortex, or the presence of visible sclerosis. | * In many other cases the lesion is visible due to destruction of cortex, or the presence of visible sclerosis. | ||
| Line 73: | Line 74: | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
*Multiple Myeloma | *[[Multiple Myeloma]] | ||
*Infection | *Infection | ||
*Primary sarcoma | *Primary sarcoma | ||
*Arthritis | *[[Arthritis]] | ||
*Low Back Pain | *Low Back Pain | ||
*Traumatic Fracture | *Traumatic [[Fracture]] | ||
== Treatment == | == Treatment == | ||
Treatment can be | Treatment can be | ||
| Line 91: | Line 85: | ||
* Local (e.g. radiotherapy or surgery). | * Local (e.g. radiotherapy or surgery). | ||
* Pain management is also often an important part of managing patients with skeletal metastases. | * Pain management is also often an important part of managing patients with skeletal metastases. | ||
Treatment is aimed first at maintaining or improving QOL and then at disease control and possible cure. | Treatment is aimed first at maintaining or improving [[Quality of Life|QOL]] and then at disease control and possible cure. | ||
* The best treatment is the treatment of the primary cancer. | * The best treatment is the treatment of the primary cancer. | ||
* Management is made by a multidisciplinary team to come up with best treatment for each individual. | * Management is made by a multidisciplinary team to come up with best treatment for each individual. | ||
| Line 104: | Line 98: | ||
* general health<ref name="ACS" /><ref name="Indian" /><ref name="Cleveland">Cleveland Clinic. Treatments and Procedures. http://my.clevelandclinic.org(accessed 26 March 2013).</ref><ref name="Prostate">Prostate Cancer Foundation. Managing Bone Metastases and Pain. http://www.pcf.org (accessed 28 March 2013).</ref> | * general health<ref name="ACS" /><ref name="Indian" /><ref name="Cleveland">Cleveland Clinic. Treatments and Procedures. http://my.clevelandclinic.org(accessed 26 March 2013).</ref><ref name="Prostate">Prostate Cancer Foundation. Managing Bone Metastases and Pain. http://www.pcf.org (accessed 28 March 2013).</ref> | ||
The following are potential treatment options for skeletal metastases: | The following are potential treatment options for skeletal metastases: | ||
# [[Chemotherapy Side Effects and Syndromes|Chemotherapy]] | |||
2. Hormone Therapy: | |||
Some hormones contribute to the growth of cancers. By keeping these hormones from affecting the cancer cells, certain types of cancers can be treated. Hormone therapy has multiple approaches. One approach is to surgically remove the organ producing the hormone. The more common approaches are prescribed drugs that can either keep the hormones from being produced or keep the hormones from affecting the cancer cells. The most common side effect of hormone therapy is hot flashes, but can depend of type of hormone therapy used. | Some hormones contribute to the growth of cancers. By keeping these hormones from affecting the cancer cells, certain types of cancers can be treated. Hormone therapy has multiple approaches. One approach is to surgically remove the organ producing the hormone. The more common approaches are prescribed drugs that can either keep the hormones from being produced or keep the hormones from affecting the cancer cells. The most common side effect of hormone therapy is hot flashes, but can depend of type of hormone therapy used. | ||
3. [[Immunotherapy]]: | |||
4. Radiopharmaceuticals | |||
Drugs that have radioactive elements are injected into the body through a vein. The drugs go into the cancerous bones and work to kill the cancer cells. Works better than external beam, but could be combined treatment. This treatment can reduce pain and be done more than once, but with reduced effects. Works best for osteoblastic. The main side effect is a lower blood cell count which can increase the risk for infection and bleeding. | Drugs that have radioactive elements are injected into the body through a vein. The drugs go into the cancerous bones and work to kill the cancer cells. Works better than external beam, but could be combined treatment. This treatment can reduce pain and be done more than once, but with reduced effects. Works best for osteoblastic. The main side effect is a lower blood cell count which can increase the risk for infection and bleeding. | ||
5. Bisphosphonates | |||
Drugs that work to slow the breakdown of bone (this can be caused by certain skeletal metastases) can be taken by mouth or given through a vein. Cancer treatments are usually done intravenously. Benefits of bisphosphonates are that they can help with the following: reduce bone pain, slow down bone damage, lower high blood calcium levels, and decrease risk for broken bones. Common side effects are fatigue, fever, nausea, vomiting, diarrhea, anemia, weakness, arthralgia, myalgia, and bone/joint pain. Something to be cautious about is that another side effect is osteonecrosis of the jaw (a portion of the jaw lacks blood supply and dies). It is important to have routine dental check-ups. | Drugs that work to slow the breakdown of bone (this can be caused by certain skeletal metastases) can be taken by mouth or given through a vein. Cancer treatments are usually done intravenously. Benefits of bisphosphonates are that they can help with the following: reduce bone pain, slow down bone damage, lower high blood calcium levels, and decrease risk for broken bones. Common side effects are fatigue, fever, nausea, vomiting, diarrhea, anemia, weakness, arthralgia, myalgia, and bone/joint pain. Something to be cautious about is that another side effect is osteonecrosis of the jaw (a portion of the jaw lacks blood supply and dies). It is important to have routine dental check-ups. | ||
6. Denosumab | |||
A drug that helps slow down the breakdown of bone and reduces chance of developing a fracture. It is injected under the skin every four weeks. Common side effects are nausea, diarrhea, and fatigue. High likelihood of causing low blood calcium, usually need to take calcium and vitamin D supplements. | A drug that helps slow down the breakdown of bone and reduces chance of developing a fracture. It is injected under the skin every four weeks. Common side effects are nausea, diarrhea, and fatigue. High likelihood of causing low blood calcium, usually need to take calcium and vitamin D supplements. | ||
7. Bone cement | |||
8. External [[Radiation Side Effects and Syndromes|Radiation Therapy]]: | |||
9. Ablation Therapy | |||
10. Surgery | |||
This is done to help reduce a person's symptoms and to help stabilize a weakened bone. Screws, plates, pins, and rods can be used to help keep a bone from staying unstable. Surgery should not be rushed or first choice of treatment. It could cause permanent or irreversible harm to the patient. | This is done to help reduce a person's symptoms and to help stabilize a weakened bone. Screws, plates, pins, and rods can be used to help keep a bone from staying unstable. Surgery should not be rushed or first choice of treatment. It could cause permanent or irreversible harm to the patient. | ||
11. [[Pain Medications|Pain medications]] | |||
Here is the ACR Appropriateness Criteria Narrative and Rating tables. One is for skeletal bone metastases and non-skeletal metastases.: https://acsearch.acr.org/docs/71097/Narrative/ https://acsearch.acr.org/docs/69354/Narrative/ | Here is the ACR Appropriateness Criteria Narrative and Rating tables. One is for skeletal bone metastases and non-skeletal metastases.: https://acsearch.acr.org/docs/71097/Narrative/ https://acsearch.acr.org/docs/69354/Narrative/ | ||
Revision as of 08:03, 6 September 2020
Original Editors - from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Amy Person, Rebecca Porter, Cassandra Ferrett, Elaine Lonnemann, Thomas Mudd, Lucinda hampton, Admin, Selena Horner, Evan Thomas, Wendy Walker, Kim Jackson and Vidya Acharya
Introduction[edit | edit source]
Skeletal metastases (a cancer of the bone that has originated from another site) are common and result in significant morbidity in patients with metastatic disease.[1]
- Bones are a common site for certain cancers such as breast cancer and prostate cancer.
- The most common sites for skeletal metastases are the spine (this is the most common site), pelvis, femur, humerus, ribs, and skull.
- The diagnosis is often straightforward, especially as in many cases there is a well-documented history of metastatic malignancy
- Sometimes they may mimic benign disease or other primary malignancies[2]
Despite recent advances in therapeutic approaches, bone metastases remain incurable and produce multiple complications called skeletal-related events, including hypercalcemia, pathological fractures, spinal compression, and bone pain, which are associated with poor prognosis[3].
- Skeletal metastases usually occur in an advanced cancer.
- “Its prevalence is rising due to higher rate of diagnosis, better systemic treatment, longer lives with the disease and higher disease burden rate”.[4]
There are two types of bone cells, osteoblast and osteoclast. Osteoblast is the forming of new bone, the tumor signals to the bone to overproduce bone cells. Osteoclast is what dissolves the bone, leaving weakened bones. With osteoclast, you develop osteolytic lesions which are when the bone breaks down. This allows excess calcium to be released into the bloodstream. Osteoblastic or osteolytic changes will be seen in most cancers, sometimes both are seen.[5][6][7][4]
This 3-minute computer-animated video explains the process of cancer spreading to bone and how the cancer affects the bone once it has implanted.
Epidemiology[edit | edit source]
Skeletal metastases account for 70% of all malignant bone tumours, and are seen in a vast number of primary cancers
- Lung cancer, breast cancer, renal cell carcinoma and prostate cancer account for approximately 80% of all skeletal metastases. This is due to not only the propensity of these tumours to metastasise to bone, but also the fact that these are some of the most common tumours[2].
- Bone is the third most common site for metastatic cancer[8]
- More than 2 out of 3 breast and prostate cancers that spread to other parts of the body spread to the bone[8]
Clinical Presentation[edit | edit source]
The majority of metastases to bone are asymptomatic. Symptoms can arise in a number of scenarios
- Local bone pain - Pain usually is worse at night and may get better with movement, but can become constant and may be worse during activity.[5]Pain is usually localized to the site of metastases, but can refer to areas around the site.[9] Pain usually increases to severe intensity.
2. Soft tissue mass resulting in:
- direct compression of adjacent structures by extraosseous soft tissue mass (e.g. cord compression)
- palpable mass
- deformity
3. Pathological fracture
4. Hypercalcemia - Some bone metastases can cause the release of calcium from the bones into the bloodstream. This can lead to hypercalcemia which can cause constipation, nausea, loss of appetite, extreme thirst, frequent urination, dehydration, fatigue, and in very serious cases confusion and even coma.[10]
In most cases the diagnosis of metastatic disease is already known.
- If no known primary exists, or there is uncertainty regarding the diagnosis (e.g. no known metastases; unusual imaging appearances) then a bone biopsy can usually allow definitive diagnosis.[2]
Pathology[edit | edit source]
The major route of spread of tumour to bone is haematogenous, although lymphatic spread is also seen
Regardless of the route of spread, metastases lead to:
- Bone loss - most likely due to direct enzymatic destruction and osteoclast activation.
- Bone formation - can be due to stromal bone formation (formation of bone within tumour substrate; the case in prostate cancer metastases) or reactive new bone formation which represents the normal adjacent bone's response to the presence of tumour and is similar to callus formation[2].
Distribution[edit | edit source]
The distribution of skeletal metastases roughly mirrors the distribution of red marrow, presumably reflecting increased blood flow in red-marrow compared to yellow marrow. Thus, metastases are usually found in:
- vertebrae
- especially the posterior vertebral body, extending into the pedicles (see: vertebral metastases)
- pelvis
- proximal femur
- proximal humerus
- skull[2]
Imaging[edit | edit source]
If a person has cancer, lab tests and imaging tests may be done to see if the cancer has spread to other sites. This is how skeletal metastases are discovered in their early stages.
Skeletal metastases invariably incite a mixture of bone resorption and bone formation and can thus take on one of three patterns, depending on the dominant process:
- Lytic metastases
- Sclerotic metastases
- Mixed lytic and sclerotic metastases
- Skeletal metastases can be difficult to identify on plain films since extensive (30-50%) bone mineral loss is required before the density loss is radiographically-visible.
- In many other cases the lesion is visible due to destruction of cortex, or the presence of visible sclerosis.
- Unlike primary bone tumours, in general metastases incite no or only limited periosteal reaction.
Nuclear medicine
Bone scans are the most sensitive routine imaging modality to try and identify both sclerotic and lytic lesions. Often demonstrate increased uptake (hot spot) although occasionally (in very aggressive purely lytic lesions) a photopenic defect (cold spot) may be visible. A superscan is also a possible pattern where extensive diffuse metastatic disease results in uniform increase in uptake.
Differential Diagnosis[edit | edit source]
- Multiple Myeloma
- Infection
- Primary sarcoma
- Arthritis
- Low Back Pain
- Traumatic Fracture
Treatment[edit | edit source]
Treatment can be
- Systemic (e.g. chemotherapy or hormonal therapy)
- Local (e.g. radiotherapy or surgery).
- Pain management is also often an important part of managing patients with skeletal metastases.
Treatment is aimed first at maintaining or improving QOL and then at disease control and possible cure.
- The best treatment is the treatment of the primary cancer.
- Management is made by a multidisciplinary team to come up with best treatment for each individual.
- In most cases treatments do not make the metastases disappear completely.
The treatments offered for skeletal metastases are influenced by many factors including:
- the type of cancer
- which bones are affected
- how many bones are affected
- whether the bones are weak or broken
- previous treatments
- symptoms
- general health[5][4][11][12]
The following are potential treatment options for skeletal metastases:
2. Hormone Therapy:
Some hormones contribute to the growth of cancers. By keeping these hormones from affecting the cancer cells, certain types of cancers can be treated. Hormone therapy has multiple approaches. One approach is to surgically remove the organ producing the hormone. The more common approaches are prescribed drugs that can either keep the hormones from being produced or keep the hormones from affecting the cancer cells. The most common side effect of hormone therapy is hot flashes, but can depend of type of hormone therapy used.
3. Immunotherapy:
4. Radiopharmaceuticals
Drugs that have radioactive elements are injected into the body through a vein. The drugs go into the cancerous bones and work to kill the cancer cells. Works better than external beam, but could be combined treatment. This treatment can reduce pain and be done more than once, but with reduced effects. Works best for osteoblastic. The main side effect is a lower blood cell count which can increase the risk for infection and bleeding.
5. Bisphosphonates
Drugs that work to slow the breakdown of bone (this can be caused by certain skeletal metastases) can be taken by mouth or given through a vein. Cancer treatments are usually done intravenously. Benefits of bisphosphonates are that they can help with the following: reduce bone pain, slow down bone damage, lower high blood calcium levels, and decrease risk for broken bones. Common side effects are fatigue, fever, nausea, vomiting, diarrhea, anemia, weakness, arthralgia, myalgia, and bone/joint pain. Something to be cautious about is that another side effect is osteonecrosis of the jaw (a portion of the jaw lacks blood supply and dies). It is important to have routine dental check-ups.
6. Denosumab
A drug that helps slow down the breakdown of bone and reduces chance of developing a fracture. It is injected under the skin every four weeks. Common side effects are nausea, diarrhea, and fatigue. High likelihood of causing low blood calcium, usually need to take calcium and vitamin D supplements.
7. Bone cement
8. External Radiation Therapy:
9. Ablation Therapy
10. Surgery
This is done to help reduce a person's symptoms and to help stabilize a weakened bone. Screws, plates, pins, and rods can be used to help keep a bone from staying unstable. Surgery should not be rushed or first choice of treatment. It could cause permanent or irreversible harm to the patient.
11. Pain medications
Here is the ACR Appropriateness Criteria Narrative and Rating tables. One is for skeletal bone metastases and non-skeletal metastases.: https://acsearch.acr.org/docs/71097/Narrative/ https://acsearch.acr.org/docs/69354/Narrative/
Prognosis[edit | edit source]
No single statement can be made with regards to the prognosis of patients with skeletal metastases as this will vary greatly depending on the primary tumour.
Physical Therapy Management[13][edit | edit source]
Physical therapy intervention focuses on optimizing the functional capacity of patients, keeping patients from becoming bed-bound, preventing pathological fracture, and helping them to maintain as much independence as possible. Thus, therapy takes on more of a maintenance or palliative role with these individuals. There is a great risk involved with working with skeletal metastasis, with the primary risk being additional fractures. Patients should be informed of this risk and that the alternative treatment of bed rest can have devastating side effects as well.
In a study conducted by Bunting et al. in 1985, fifty-four patients with bony metastases but no evidence of impending fractures on skeletal survey were observed while they underwent rehabilitation programs at a rehabilitation hospital. During this treatment period, 16 fractures occurred in 12 patients, but only 1 of these clearly occurred while the patient was participating in rehabilitation activities. Six fractures clearly occurred while the patients were in bed. This evidence suggests that an intervention of bed rest would not prevent fractures any more than rehabilitation would cause fractures.
The study investigating the factors affecting the discharge destination of patients with spinal bone metastases suggests that the level of activity of daily living at the discharge and motor paralysis predicted the discharge destination of these patients[14].
Manual muscle testing, passive or active-assisted range of motion are not evaluated on an extremity with a bony lesion due to the risk of fracture. Only active movement is assessed, and this is likely to be limited by pain. Likewise, resistive exercise involving an affected area is generally contraindicated. Treatment sessions, when appropriate, should focus on training the patient to use residual function or to develop compensatory techniques, assistive device training, and educating both the patient and family members.
In summary, effective rehabilitation can help prevent a patient with skeletal metastases from becoming unnecessarily or prematurely bed-bound and/or dependent in activities of daily living. While achievements may be limited, they can be invaluable in helping the patient maintain some control over his or her life.
References[edit | edit source]
- ↑ Radiopedia Skeletal matastases Available from: (last accessed 6.9.2020)https://radiopaedia.org/articles/skeletal-metastasis-1
- ↑ 2.0 2.1 2.2 2.3 2.4 Radiopedia Skeletal Metastases Available from:https://radiopaedia.org/articles/skeletal-metastasis-1 (last accessed 6.9.2020)
- ↑ Hiraga T. Bone metastasis: Interaction between cancer cells and bone microenvironment. Journal of Oral Biosciences. 2019 Jun 1;61(2):95-8.Available from:https://www.sciencedirect.com/science/article/abs/pii/S1349007919300064 (last accessed 6.9.2020)
- ↑ 4.0 4.1 4.2 Indian Journal of Orthopaedics. Management of skeletal metastases: An orthopaedic surgeon’s guide. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4292329/ (accessed 27 March 2017).
- ↑ 5.0 5.1 5.2 American Cancer Society. Understanding Your Diagnosis. http://www.cancer.org (accessed 21 March 2013).
- ↑ OncoLink. Bone Metastasis Treatment with Medications. https://www.oncolink.org/cancers/bone/bone-metastases/bone-metastasis-treatment-with-medications (accessed 1 April 2017).
- ↑ Zometa. Bone Metastases. http://www.us.zometa.com (accessed 21 March 2013).
- ↑ 8.0 8.1 Society of Interventional Radiology. Nonsurgical Treatments for Metastatic Cancer in Bones. http://www.sirweb.org (accessed 26 March 2013).
- ↑ University of Michigan Comprehensive Cancer Center. Bone Metastases Symptoms. http://www.cancer.med.umich.edu/cancertreat/tissue_bone/bonesymptoms.shtml
- ↑ National Cancer Institute at the National Institutes of Health. Symptoms of Hypercalcemia. http://www.cancer.gov/cancertopics/pdq/supportivecare/hypercalcemia/Patient/page2
- ↑ Cleveland Clinic. Treatments and Procedures. http://my.clevelandclinic.org(accessed 26 March 2013).
- ↑ Prostate Cancer Foundation. Managing Bone Metastases and Pain. http://www.pcf.org (accessed 28 March 2013).
- ↑ Bunting RW, Shea B. Bone metastasis and rehabilitation. Cancer 2001; 92:1020-1028. http://onlinelibrary.wiley.com/doi/10.1002/1097-0142(20010815)92:4%2B%3C1020::AID-CNCR1415%3E3.0.CO;2-I/full
- ↑ Akezaki Y, Nakata E, Kikuuchi M, Sugihara S. Factors Affecting the Discharge Destination of Patients With Spinal Bone Metastases. Annals of Rehabilitation Medicine. 2020 Feb 29;44(1):69-76.