Multiple Myeloma
Original Editors - Jill Jones from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Jill Jones, Admin, Lucinda hampton, Scott Buxton, Elaine Lonnemann, Nikhil Benhur Abburi, Johnathan Fahrner, Kim Jackson, Wendy Walker, WikiSysop, Vidya Acharya and 127.0.0.1
Description[edit | edit source]
Multiple Myeloma (MM) is a type of cancer formed by cancerous plasma cells (monoclonal proliferation of plasma cells). To date, multiple myeloma is an incurable disease with a poor prognosis. Most individuals die within 1 to 3 years after the diagnosis is made.[1]
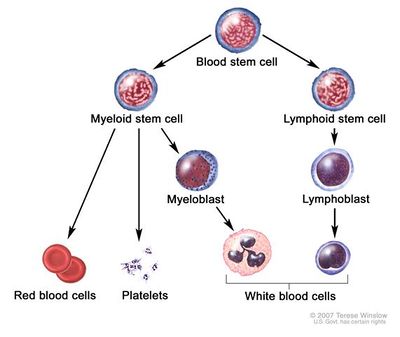
The immune system
- Made up of several types of cells that work together to fight infections.
- Lymph cells (called lymphocytes) are the main type of cell in the immune system.
- There are 2 types of lymph cells: T cells and B cells.
- When B cells respond to an infection, they change into plasma cells. Plasma cells, also called plasma B cells, are white blood cells that originate in the bone marrow and secrete large quantities of proteins called antibodies in response to being presented specific substances called antigens.
- When plasma cells grow out of control, they can form a tumor, usually in the bone marrow.
- This type of tumor is called a myeloma, and if there are many tumors they are called multiple myeloma.[2]
- Tumors of this type initially affect the bones and bone marrow of the vertebrae, ribs, skull, pelvis, and femur. These regions are most often affected because of their high concentrations of bone marrow. The progression of this disease can cause damage to the kidney, lead to recurrent infections, and often affects the nervous system [1].
Etiology[edit | edit source]
The exact etiology of MM is unknown.
- There is evidence that suggests genetic abnormalities in oncogenes such as CMYC, NRAS, and KRAS may play a role in the development of plasma cell proliferation.
- MM has also been associated with other factors such as drinking alcohol, obesity, environmental causes such as insecticides, organic solvents, and radiation exposure.[3]
Epidemiology[edit | edit source]
- MM represents 1.8% of all new cancer cases in the United States.
- Occurs predominantly in the geriatric population with a median age at diagnosis of about 70 years.
- The number of cases diagnosed annually is expected almost to double in 20 years.
- It has a male-to-female ratio of 3 to 2 and is more common among African-Americans[3].
Presentation[edit | edit source]
The presentation can vary from asymptomatic to severely ill.
- Usually, the patient is an older adult complaining of constitutional symptoms such as fatigue, weight loss, and bone pain, particularly in the back and chest.
- Pathological fractures and vertebral collapse lead to a reduction in height, spinal cord compression, radicular pain or kyphosis.
- Anaemia usually causes pallor, palpitation and worsening of previous heart failure or angina.
- Renal failure (acute and/or chronic) can lead to edema, acidosis, and electrolyte disturbances. Hypercalcemia, dehydration, and hypergammaglobulinemia further aggravate renal injury and may lead to confusion and coma.
- Secondary amyloidosis can cause peripheral neuropathy and carpal tunnel syndrome.
- Those with hyperviscosity may have symptoms like paresthesia, headache, dyspnea, nasal bleeding, blurry vision.
- MM patients are more prone to infections, mostly pneumonia, and pyelonephritis.
Physical examination. Variable depending on the extent of disease, usually include
- Pallor, tachycardia, tachypnea, petechiae or ecchymoses, bone tenderness, edema or signs of dehydration and central or peripheral neurologic signs.
- Fundoscopic signs include exudative macular detachment, retinal hemorrhage or cotton-wool spots. Carpal tunnel syndrome may cause positive Tinel and Phalen signs[3]
Radiographic features[edit | edit source]
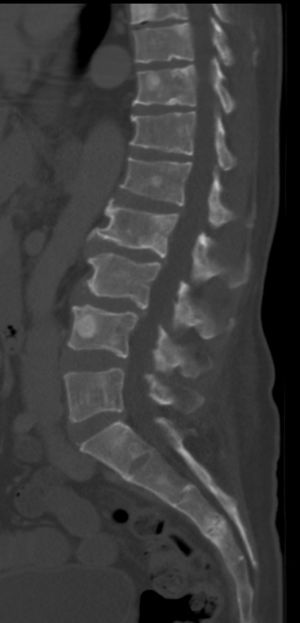
Radiographic features - Include:
- Numerous well circumscribed, lytic bone lesions
- Punched out lucencies
- Raindrop skull
- Endosteal scalloping
- Generalised osteopenia
Treatment / Management[edit | edit source]
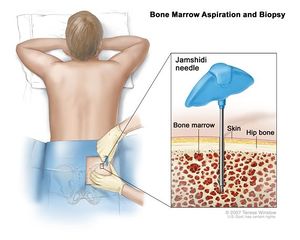
- Initial therapy of MM varies depending on disease risk stratification and functional status, which will help determine transplant eligibility. Patients who are
- Fit for transplant typically receive induction therapy for a few months to decrease the tumor burden, followed by peripheral blood stem cell mobilization and harvesting, and finally, an autologous transplant.
- Transplant-ineligible patients, common regimens include lenalidomide and dexamethasone, bortezomib and dexamethasone, melphalan/prednisone/bortezomib, and other bortezomib-based regimens. Novel agents such as oral proteasome inhibitors have shown promising results.
2. For symptomatic anemia, blood transfusion and sometimes erythropoiesis-stimulating agents are used.
3. Plasmapheresis is used for the hyperviscosity syndrome.
4. Hypercalcemia and renal failure treatments include hydration, glucocorticoids, bisphosphonates, calcitonin, and hemodialysis.
5. MM patients are more prone to infections. Prophylactic measures include yearly influenza vaccine, pneumococcal vaccine at the time of diagnosis, prophylactic antibiotics and hematopoietic growth factors during the first few months of chemotherapy induction, intravenous immunoglobulin for patients with recurrent infections.
6.Bone pain usually requires opioids for control.
7. Spinal cord compression by vertebral fracture or plasmacytoma is a medical emergency and should be managed aggressively with radiotherapy and orthopedic consultation.s into your bloodstream so they can be collected and transplanted back into the body.[3]
Diagnostic Procedures[edit | edit source]
According to the National Comprehensive Cancer Network (NCCN) criteria, MM is defined as smoldering (asymptomatic) or active (symptomatic). Major and minor criteria were created to distinguish multiple myeloma from asymptomatic myeloma and monoclonal gammopathies of undetermined significance (MGUS).
- The Evaluation of the patient is an involved process and beyond the scope of this article[3].
- Diagnosis is not always obvious, especially in older patients, given their increased comorbidities. MM should always be suspected in an elderly patient with normocytic anemia, bone pain and evidence of renal dysfunction.
Prognosis[edit | edit source]
- Older patients will often have serious concomitant diseases affecting survival.
- Younger patients have less treatment-related morbidity, and consequently, fare better.
- In 2003, with high-dose therapy followed by autologous stem cell transplantation, median survival was estimated to be approximately 4.5 years, compared to a median of approximately 3.5 years with standard therapy.
- The overall survival in MM has improved over the last decade due to more accurate diagnosis and risk stratification, a better understanding of how toxicity and frailty can affect prognosis, the discovery of novel agents, and advances in supportive care during the post-transplant period.[3]
- Overall, the 5-year survival rate is around 35%
Systemic Involvement[edit | edit source]
Immune System:
- Recurrent bacterial infections (especially pneumococcal pneumonias)
Circulatory system:
- Anemia with weakness and fatigue Bleeding tendencies
Skeletal System:
- Bone destruction
- Skeletal/bone pain (especially pelvis, spine and ribs)
- Spontaneous fracture
- Osteoporosis
- Hypercalcemia (confusion, increased urination, loss of appetite, abdominal pain, vomiting, and constipation)
Urinary system:
- Renal involvement
- Kidney stones
- Renal insufficiency
Neurological Systems:
- Neurologic abnormalities
- Carpal tunnel syndrome
- Back pain with radicular symptoms
- Spinal cord compression (motor or sensory loss, bowel/bladder dysfunction, paraplegia)[1]
Physical Therapy Management[edit | edit source]
Therapists can assist individuals with multiple myeloma to manage both the disease and treatment-related symptoms, improve overall quality of life, and prevent further complications associated with decreased activity and exercise.
- An important role in various stages of the progression of this disease includes prevention and management of: skeletal muscle wasting; cancer-related fatigue, and pathologic fractures. Exercise interventions to improve function and decrease muscle wasting and cancer-related fatigue during and after cancer treatment for multiple myeloma have been shown effective.[4]
- Individualized exercise programs for individuals receiving aggressive treatment for multiple myeloma may be effective for decreasing fatigue and mood disturbance and for improving sleep.
- The guidelines suggest referral to physical therapy: Fitness assessment and exercise recommendations (emphasis on getting clients to gradually increase their activity level to avoid sustaining an injury or becoming discouraged). Short, low-intensity exercise programs may be helpful at first.
- Implementation of a falls prevention programs can be a life-saving intervention for the individual at risk for pathologic fractures.[4]
Differential Diagnosis[edit | edit source]
Other conditions that can cause symptoms that may be confused with multiple myeloma that should be ruled-out include[5]:
- Connective tissue disorders
- Chronic infections
- Skeletal (bone) metastases from cancers at other sites
- Other causes of monoclonal gammopathy (increased levels of monoclonal antibodies) that include: Smoldering Multiple Myeloma, Solitary Plasmacytoma, Waldernstrom Macroglobulinemia, Plasma cell Leukemia (almost always associated with active multiple myeloma, Amyloidosis
Case Reports[edit | edit source]
- Multiple myeloma and engine exhausts, fresh wood, and creosote: A case-referent study[6] [view article in American Journal of Industrial Medicine]
- Occupational and other environmental factors and multiple myeloma: a population based case-control study[7] [view article in Occupational and Environmental]
- Multiple myeloma: A review of the epidemiologic literature[8] [view article in International Journal of Cancer]
- Familial characteristics of autoimmune and hematologic disorders in 8,406 multiple myeloma patients: A population-based case-control study[9] [view article in International Journal of Cancer]
Resources[edit | edit source]
- Multiple Myeloma Research Foundation: http://www.multiplemyeloma.org/
- American Cancer Society: http://www.cancer.org
- International Myeloma Foundation: http://myeloma.org
- National Cancer Institute: http://www.cancer.gov/
References[edit | edit source]
- ↑ 1.0 1.1 1.2 3. Goodman C, Snyder T. Differential Diagnosis for Physical Therapists: Screening for Referral. St. Louis: Saunders Elsevier; 2007.
- ↑ American Cancer Society website. 2010. Available at: http://www.cancer.org/docroot/CRI/content/CRI_2_2_1x_What_Is_Multiple_Myeloma.asp?sitearea=. Accessed April 4, 2010.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Albagoush SA, Azevedo AM. Cancer, Multiple Myeloma.Available from: https://www.ncbi.nlm.nih.gov/books/NBK534764/ (last accessed 14.7.2020)
- ↑ 4.0 4.1 Goodman C, Fuller K. Pathology: Implications for the Physical Therapist. St. Louis: Saunders Elsevier; 2009.
- ↑ MedifocusHealth.com 2007. Available at: http://www.medifocushealth.com/HM008/Diagnosis-of-Multiple Myeloma_Differential-Diagnosis-for-Multiple-Myeloma.php. Accessed April 4, 2010.
- ↑ Flodin U, Fredriksson M, and Persson B. Multiple myeloma and engine exhausts, fresh wood, and creosote: A case-referent study. American Journal of Industrial Medicine. Jan 2007. Volume 12; 5, 519-529.
- ↑ Eriksson M and Karlsson M. Occupational and other environmental factors and multiple myeloma: a population based case-control study. Br J Ind Med 1992;49:95-103.
- ↑ Alexander D, et. al. Multiple myeloma: A review of the epidemiologic literature. International Journal of Cancer. 2007. Volume 120; 12.
- ↑ Landgren O, et. al. Familial characteristics of autoimmune and hematologic disorders in 8,406 multiple myeloma patients: A population-based case-control study. Int. J. Cancer. 2006. Volume 118, 3095–3098.