Alcoholism
Original Editors - Stephanie Gloyeske from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Stephanie Gloyeske, Mahbubur Rahman, Elaine Lonnemann, Admin, Lucinda hampton, Kim Jackson, WikiSysop, 127.0.0.1, Laura Ritchie, Wendy Walker and Vidya Acharya
Introduction[edit | edit source]
Alcoholism also known as Alcohol use disorder (AUD) is a serious disease where people have an overpowering desire for the physical and mental effects of drinking alcoholic beverages.[1]
- While less than half of the world’s adults have consumed alcohol in the last 12 months, the global burden of disease caused by its harmful use is enormous. Disturbingly, it exceeds those caused by many other risk factors and diseases high on the global health agenda.
- Over 200 health conditions are linked to harmful alcohol use, ranging from liver diseases, road traffic injuries and violence, to cancers, cardiovascular diseases, suicides, tuberculosis and Human Immunodeficiency Virus (HIV).
- Although the highest levels of alcohol consumption are in Europe, Africa bears the heaviest burden of disease and injury attributed to alcohol[2].
Epidemiology[edit | edit source]
Globally, alcohol use disorder affects 240 million people mostly in Europe and the Americas.
- Overall alcohol use disorder tends to be more common in individuals with less education and low income.
- An estimated 20.8 million Americans age 12 and older had a substance use disorder - 15.7 million were alcohol use disorders. Of those, 2.7 million had an illicit drug use disorder as well. This number makes alcohol the leading substance abused in the United States[3].
- It has also be reported that the earlier an individual starts drinking (14 or younger) the more likely they will develop alcohol related problems.[4]
Etiology[edit | edit source]
Pathogenesis of alcohol use disorder is not strictly known - several factors are thought to contribute to its development including:
- Environmental influences, such as home environments, peer interactions
- Genetic factors
- Level of cognitive functioning
- Certain existing personality disorders e.g. disinhibition and impulsivity-type disorders, as well as depressive and socialization-related disorders[3].
Characteristics/Clinical Presentation[edit | edit source]
History taking is important which may often reveal reported episodes of binge drinking of four or five or more drinks at a time. Use of the CAGE questionnaire will reveal a score of 2 or greater (CAGE means (1) have you ever felt you should Cut down on your drinking, (2) have you ever been Annoyed by people criticizing your drinking, (3) have you ever felt Guilty about your alcohol use, or (4) have you ever needed an Eye-opener to steady your nerves or get rid of a hangover). The patient may also report frequent falls, blackout spells, unsteadiness, or visual disturbances like symptoms; seizures if they went a few days without drinking as withdrawal symptoms, or tremors, confusion, emotional disturbances; frequent job changes; social issues, such as job termination, separation/divorce, estrangement from family; sleep disturbances may also found.[5]
In later stages, the patient may complain of nausea/vomiting, hematemesis, abdominal distension, epigastric pain, weight loss, jaundice, or other symptoms or signs indication of liver dysfunction. They may be not produce any symptoms on early stage.[5]
During the objective examination patients may exhibit: signs of cerebellar dysfunction, such as ataxia or difficulty with fine motor skills; slurred speech, tachycardia, memory impairment, nystagmus, disinhibited behavior, or hypotension; tremors, confusion/mental status changes, ruddy palms, jaundice, ascites, or other signs of advanced liver disease; spider angiomata, hepatomegaly/splenomegaly. Labs test may reveal anaemia, thrombocytopenia, coagulopathy, hyponatremia, hyperammonemia, elevated ammonia levels, or decreased B12/folate levels if the advanced liver disease develops.[5]
Associated Co-morbidities[edit | edit source]
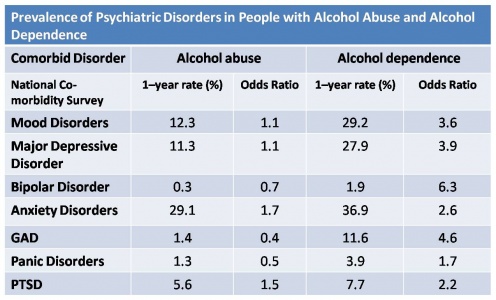
Co-morbidities associated with alcoholism are usually psychological in nature. The following table shows the prevalence of different psychological disorders than have gone along with alcoholism.
The odds ratio represents the increased chance that someone with alcohol abuse or dependence will have the co-morbid psychiatric disorder.[4] From looking at the table, a person with alcohol dependence is 3.6 times more likely to also have a mood disorder compared to a person without alcohol dependence.
Treatment[edit | edit source]
Treatment approaches should be a combination of nonpharmacological and pharmacological interventions. Nonpharmacological or psychologically based treatment methods include motivational interviewing, motivational enhancement therapy (MET), and cognitive behavioral therapy (CBT).[3]
Some treatment foci that have demonstrated promise include,
- Evidence-based motivational interviewing - helps the patients explore the reasons behind their ambivalence with respect to changing their behavior or alcohol cessation to change their substance abuse-related behaviors with a personalized assessment of risks and needs
- Cognitive behavior therapy
- 24-hour residential facilities that aim to treat medical as well as psychiatric complications or comorbidities associated with the alcohol use and process of cessation.
- Multiple programs, such as Alcoholics Anonymous (AA) or other 12-step programs that focus on group support/mentors that can provide a source of assistance with the maintenance of abstinence. Many patients have lapses during their lifetime and will require initiation of differing intensities of therapy throughout their lifetime.[3]
Current Guidelines by American Psychiatric Association includes:
- Clinician advice on harms of alcohol makes a big difference
- Hospitalize patients with delirium tremens. Patients with no social support, major psychiatric disorders, and history of relapse should be admitted
- Recommend AA
- Urge patient to remove all alcohol from the home
- Encourage family members to attend AA
- Both naltrexone and acamprosate can be used to treat alcohol abuse disorder when non-pharmacological methods do not work
- Disulfiram is no longer recommended
- Second line drugs of choice include gabapentin and topiramate[3]
Additionally,
- Alcoholics tend to have poor dietary choices, and folate deficiency is common
- Encourage a healthy diet of fruits and vegetables[3]
Prognosis[edit | edit source]
Alcoholism is associated with many adverse affects. Based on WHO reports, it is associated with at least 3 million deaths each year, most of these occurring in men. Besides death, alcohol use disorder is associated with:
- Motor vehicle collisions
- Cirrhosis
- Oral cancer
- Esophageal, liver and breast cancer
- Homicide and suicide
- Hemorrhagic stroke[3]
The prognosis for most alcoholics is guarded; with less than 20-30% discontinuing drinking.
- In many instances, some of the organ damage is often irreversible.
- The key is to educate the patient and the family about the destruction that alcohol can cause.
- Referral to Alcoholics Anonymous (AA) is recommended, but data indicate that compliance is often low.[3]
Physical Therapy Management[edit | edit source]
Substance Abuse: Preferred Practice Patterns:[6]
- 4A: Primary Prevention/Risk Reduction for Skeletal Demineralization (alcohol and tobacco use/abuse)
- 5G: Impaired Motor Function and Sensory Integrity Associated with Acute or Chronic Polyneuropathies (alcohol-related)
- 7A:Primary Prevention/Risk Reduction for Integumentary Disorders (injection, drug use, tobacco use, and delayed wound healing, SCI population)
Substance abuse, including alcoholism, can impair or slow the rehabilitation process, especially delay wound healing. The individual should be encouraged to reduce or eliminate if possible the intake, during the rehabilitation process to accelerate the healing process. Many people who seek medical attention fail to disclose their alcohol or drug use.
Physical therapists must be alert to alcohol and other drug use and abuse. Since physical therapists generally spend more time with patients/clients than many other health professionals, they may be the ones best able to recognize substance abuse that would be hidden from those who spend less time with the client or who do not have the skills to recognize impairments of the cognitive and motor systems.[6] It may be helpful to assess the behavioral impact by asking the following questions:
- When is it that you feel you need these substances?
- How do these activities help you?
- Are you concerned about your dependence?
- Do you have a pattern of cutting back or stopping the use of alcohol, but then restarting it?
- Have you been concerned or has anyone around you raised concern about your use of alcohol?
If an individual reports the use of alcohol, the therapist should ask whether the person has discussed it with their physician or other health care personnel. The individual should be encouraged to seek medical attention or that it will be addressed as part of the medical problem with the physician.
Alcoholism and Rehabilitation[edit | edit source]
Patients with physical injuries requiring rehabilitation may be at particular risk to being alcoholism due to many factors, such as pain, impairments, mood disturbances, employment related difficulties, and problems of self-image. Often, alcohol abuse or alcoholism are involved in the cause of physical injuries. Post injury alcohol abuse is particularly important as it may interrupt the rehabilitation process.[7] Physical therapists and other rehabilitation professionals should consider this pivotal factor during their practices.
Differential Diagnosis[edit | edit source]
Case Reports[edit | edit source]
Resources[edit | edit source]
Alcoholics Anonymous
National Association for Children of Alcoholics Al-Anon/Alateen National Institute on Alcohol Abuse and Alcoholism National Council on Alcoholism and Drug Dependence
References[edit | edit source]
- ↑ World Book Encyclopedia. Alcoholism. 2001 Edition. pg. 337-338
- ↑ World Health Organization. Global status report on alcohol and health 2018. World Health Organization; 2019 Feb 14.Available from:https://apps.who.int/iris/bitstream/handle/10665/274603/9789241565639-eng.pdf?ua=1 (last accessed 31.10.2020)
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 Nehring SM, Freeman AM. Alcohol Use Disorder [Internet]. PubMed. Treasure Island (FL): StatPearls Publishing; 2020. Available from: https://www.ncbi.nlm.nih.gov/books/NBK436003/
- ↑ 4.0 4.1 National Institute of Alcohol Abuse and Alcoholism. FAQ for the General Public. Retrieved March 30, 2010, from www.niaaa.nih.gov/FAQs/General-English/default.htm
- ↑ 5.0 5.1 5.2 Nehring SM, Freeman AM, Doerr C. Alcohol Use Disorder (Nursing) [Internet]. PubMed. Treasure Island (FL): StatPearls Publishing; 2021. Available from: https://www.ncbi.nlm.nih.gov/books/NBK568739/
- ↑ 6.0 6.1 Fuller, K. and Goodman, C. Pathology: Implications for the Physical Therapist. St. Louis, Missouri: Saunders Elsevier
- ↑ Hubbard JR, Everett AS, Khan MA. Alcohol and drug abuse in patients with physical disabilities. The American Journal of Drug and Alcohol Abuse [Internet]. 1996 [cited 2021 May 5];22(2):215–31. Available from: https://pubmed.ncbi.nlm.nih.gov/8727056/