Radiation Side Effects and Syndromes
Original Editors -Alicia Dupilka & Kristin Gramling from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Kristin Gramling, Alicia Dupilka, Lucinda hampton, Vidya Acharya, Kim Jackson, Admin, Elaine Lonnemann, WikiSysop, 127.0.0.1 and Wendy Walker
Definition/Description [edit | edit source]
Radiation therapy, or radiotherapy, is a common oncologic treatment modality utilising ionising radiation to control or eliminate malignant cells. Radiotherapy may be used alone, or synergistically with chemotherapy or immunotherapy. The type of radiation therapy employed depends on the disease and the specific type of cancer being treated.
Radiotherapy plays a part in:
- Primary curative treatment (eg. head and neck cancer),
- Adjuvant therapy (e.g. reducing recurrence rate after local breast cancer surgery)
- Palliation of cancer symptoms (e.g. reducing pain from bone metastases).
- Treating non-malignant disease, e.g. Graves thyroiditis, keloid scarring.[1]
- Nearly two-thirds of all cancer patients will receive radiation therapy [2]
- There are no good estimates of how many of these patients will develop complications due to the radiation therapy [3]
Techniques[edit | edit source]
Radiotherapy is customarily divided into three main categories:
- External beam radiotherapy (EBRT) where a medical linear accelerator (linac) directs ionising radiation at the tumour from outside the body eg
- Conventional Radiation Therapy. This refers to the old techniques of radiation therapy where treatments would be planned by defining a limited number of beams with the boundaries delineated on orthogonal x-rays of the patient. It has been largely replaced by other highly conformal external beam radiation therapies, which use CT images to plan the treatment.[4] Examples of these newer techniques include: three-dimensional conformal radiation therapy (3D-CRT); intensity-modulated radiation therapy (IMRT); stereotactic radiosurgery; electron therapy; particle (hadronic) therapy.[1]
- Sealed source radiotherapy (brachytherapy) where a radiation source(s) is placed, under the guidance of imaging, within or next to the area requiring treatment.
- Unsealed source radiotherapy (systemic radioisotope therapy) where a radioisotope is delivered through: infusion e.g. for neuroendocrine tumours ; ingestion e.g for thyroid cancer.[1]
Characteristics/Clinical Presentation[edit | edit source]
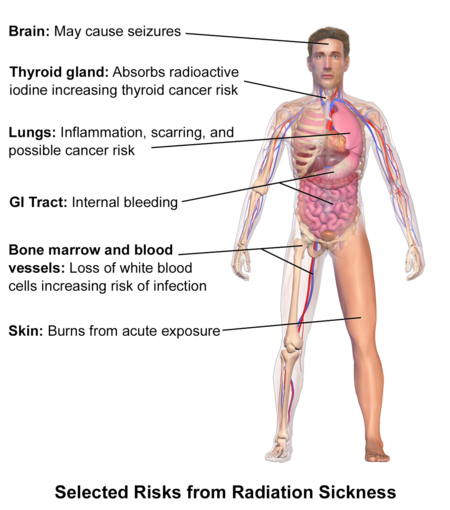
Side Effects
Depend on the area of the body being treated, dose given per day, total dosage, general medical condition and other treatments being given.
- Acute radiation injury
- Nausea, malaise, dysphagia, vomiting immediately following irradiation
- Erythema
- Mucosal inflammation (stomatitis, esophagitis, enteritis, etc.)
- Bone marrow damage: Anaemia, thrombocytopenia, and/or leukocytopenia (pancytopenia)
- Infection due to immunocompromise
- Early radiation-induced lung injury (radiation pneumonitis): Dyspnea, dry cough, hemoptysis, and fever may occur several weeks following radiation.
- Partial respiratory insufficiency is an early sign.
- Chronic radiation damage
- Radiation Fibrosis Syndrome
- Late radiation-induced lung injury (radiation fibrosis)
- Bone: fractures
- Bone marrow damage: anemia, thrombocytopenia, and/or leukocytopenia (pancytopenia); Infection due to immunocompromise
- Heart: increased risk of myocardial infarction
- Gastrointestinal: impaired function
- Thyroid: impaired function (hypothyroidism)
- Impaired fertility: Fibrosis in ovaries involving amenorrhea; Azoospermia
- Radiation of the head: Leukoencephalopathy; Hormone imbalances and their outcomes, such as stunted growth due to low growth hormone levels
- Xerostomia
- Malignancies: especially leukemias, MDS, lymphoma, thyroid cancer[5]
Common general side effects of radiation therapy[edit | edit source]
Fatigue: Is different from the fatigue of everyday life, and it might not get better with rest. It can last a long time and can get in the way of usual activities. It will usually go away gradually after treatment ends. It’s very common for people with cancer and with radiation therapy. Usually starts after a few weeks of radiation therapy as a result of radiation treatments which destroys some healthy cells as well as the cancer cells. Fatigue usually gets worse as treatment goes on. Stress from being sick and daily trips for treatment can make fatigue worse. Managing fatigue is an important part of care[6].
Radiation Dermatitis/ Erythema: Skin in the radiation treatment area might look red, irritated, swollen, blistered, sunburned, or tanned. After a few weeks, the skin might become dry, flaky, or itchy, or it may peel.
Hair loss: Radiation therapy can cause hair to be thinned or lost in the area being treated. Eg radiation to the head may cause hair loss on your head (even eyebrows and lashes). Most people find that their hair grows back after treatment ends. When it does grow back, the hair may be thinner or a different texture than it was before.
Low blood count: Rarely, radiation therapy can cause changes in blood count levels, making clients more vulnerable to bleeding and infections. If blood tests show low blood counts, treatment might be stopped for a week or so to allow blood counts to return to normal (this side effect is more likely if you’re also getting chemotherapy)[6].
Specific side effects of radiation therapy[edit | edit source]
Gastrointestinal
- Radiation Esophagitis: often involved in radiation treatment for lung cancer especially when a chemosensitizer is also used. Symptoms usually resolve in 1 to 3 weeks after radiation is finished. Symptoms: abnormal peristalsis, odynophagia (pain with swallowing) and dysphagia
- Radiation Enterocolitis: often results in fibrosis leading to strictures in the intestines, bowel obstruction, fistulas with abscess formation, ulceration with bleeding and malabsorption
- Acute or Chronic Radiation Enteritis[2].
Pulmonary
Cardiovascular
- Radiation Heart Disease - may result in pericarditis, Coronary artery disease, myocardial disease and aortic-valve disease
Musculoskeletal
Connective Tissue Involvement - late changes such as fibrosis, atrophy and contraction is common especially in collagen
- In bones and limbs it can cause weakness, limb-length discrepancies and scoliosis
- It can result in edema and decreased range of motion
- It can cause pelvic adhesions that result in painful motion and sometimes plexopathy (a disorder affecting a network of nerves in the brachial or lumbosacral plexus, resulting in pain and loss of motor control).
- In the circulatory and lymphatic system it can cause loss of elasticity on contractility of vessels. Even though the actual lymph vessels may maintain their shape, fibrosis in the surrounding tissue can inhibit growth of the vessels into tissues that need to be healed.
Nervous System
- Acute symptoms: occur during treatment and include debilitating fatigue; cranial radiation may result in short-term memory loss, changes in behavior and cognition, decreased appetite, dry skin, hearing loss, hair loss and decreased salivation
- Subacute symptoms: occur 1 to 4 months after treatment and are not as common. Radiation to the cervical spine may result in subacute myelopathy (Lhermitte's sign). Radiation to the brainstem may result in ataxia, nystagmus and dysarthria
- Chronic symptoms: occur months to years after therapy and can include damage to the cerebral vasculature leading to coronary artery disease, transient ischemic attacks, stroke or myocardial infarction.
- Radionecrosis - results from whole-brain radiotherapy. Secondary tumors may develop and the hypothalamic system may be affected. Symptoms: headache, changes in cognition and personality, focal neurological deficits and seizures.
- Myelopathy - results from radiation of the spinal cord. May present as Brown-Sequard syndrome or motor neuron syndrome.
- Plexopathy - results from damage to the brachial and lumbar plexuses. Symptoms may include paresthesias, motor deficits, lymphedema and pain.
Radiation Fibrosis Syndrome (RFS)
Radiation affects healthy cells within the treatment field, and can cause an increased production of fibrin (a protein found in the body that accumulates and causes damage in radiated tissue over time). Radiation fibrosis can affect any tissues in the radiation field. This damage can cause shortening of tissues, contracture and atrophy of muscle, cause bones to become weak and brittle, cause heart, lung and nerve damage (neuropathy) and lymphedema.
Patients may notice signs and symptoms of RFS anywhere from a few weeks to years after treatment has ended. These symptoms will progress over time.
Patients being treated with radiation for head and neck cancer are at a higher risk of developing radiation fibrosis syndrome (RFS) due to the high doses of radiation to parts of the body with structures crucial to activities of daily living eg eating, moving head. Some examples of the problems encountered include:
- Decreased ability to fully open the mouth (trismus)
- Neck pain and tightness (cervical dystonia)
- Lymphedema (swelling)
- Difficulty with speech and swallowing
The treatment for RFS depends upon the symptoms and side effects the patient is having. Physical therapy, occupational therapy, speech and swallow therapy, and surgery may all play a part in treatment for RFS.[7]
Medical Management[edit | edit source]
- Clinical trials to learn how to use radiation therapy more safely and effectively are being conducted by doctors and scientists. [5]
- Working on improving image-guided radiation. [5]
- Research is also being done on radiosensitizers and radioprotectors. [5]
- The use of carbon ion beams is still being investigated and remain experimental. This type of therapy are not currently available in the US. [5]
Physical Therapy Management[edit | edit source]
Cancer and treatment can cause physical problems including, but not limited to, pain, fatigue and muscle weakness. These often interfere with life in physical, emotional and practical ways.
Physiotherapy rehabilitation services can work on: improving strength and stamina; pain resolution; site specific problems eg contractures, lymphedema, RFS; education re skin care, importance of remaining physically active and good nutrition.
- Physical therapists should always wash their hands before treating a patient who has undergone radiation therapy to protect that client from possible infection.[2]
Skin Care[2]
- Avoid use of alcohol/drying agents, lotion, gel, or oil. Creams and gels can increase the dosage received on the skin and increase the likelihood of side effects
- Do not wash away markings of the targeted area
- Position the patient so they are not lying on the targeted area
- Avoid exposing the patient to sources of heat, including direct sunlight and modalities
- Monitor wound healing
Musculoskeletal [2]
- If adhesions are present in the hip after radiation of the pelvis, be sure to incorporate range of motion activities; early intervention is important to prevent contractures and restrictive scarring.
- Post-radiated tissue can tear when stretching so it is important to observe for blanching of the skin during stretching and not to stretch beyond that point. Stretching should be continued 18 to 24 months after radiation therapy has been discontinued.
Nervous System [2]
- Anyone with neurological signs or symptoms of an unknown cause should be asked about a previous history or cancer and radiation therapy
Infection[2]
- Therapists should observe carefully for signs of infection in patients who have undergone radiation treatment. The first and only sign may be a fever because the patient may be immunosuppressed and their body cannot create a normal inflammatory response.
- A successful protocol should include patient education, exercise evaluation and an individualized exercise prescription. - Therapists must monitor vital signs in patients who have undergone radiation treatment because radiation and chemotherapy can leave the lungs and heart tissue permanently scarred. Patients should be taught to monitor their own vitals including heart rate, respiration rate and rate of perceived exertion (should not exceed 15 to 17) and taught to detect signs of complications such as dyspnea, pallor, excessive perspiration, or fatigue while exercising. Patients should be told not to exercise within 2 hours of chemotherapy or radiation therapy because it increases the circulation and may increase the effects of the treatment.
- Studies have shown low to moderate intensity aerobic exercise during the same weeks of radiation treatment can help improve physical function and lower subjective levels of fatigue, anxiety, depression and sleep disturbances.
Management of Syndromes Associated with Radiation Fibrosis Syndrome[3]
Physical Therapy is usually the first line of treatment for the dysfunctions listed below.
- Neck Extensor Weakness - emphasize postural retraining through core strengthening, flexibility of the shoulder musculature, and strengthening the cervicothoracic and rotator cuff muscles. This will help reduce energy demands and pain. It is also important to develop a long-term home exercise program
- Shoulder Pain and Dystonia - treated through conservative measures because shoulder surgery should be avoided in patients with RFS because damage of the neruomuscular structures often results in poor surgical outcomes. Work on core strength and posture, neck extensor and rotator cuff strength and stretching of pectoral girdle musculature in order to try to restore normal anatomical alignment of the shoulders. There is a potential long-term benefit if the patient consistently follows a home exercise program.
- Cervical Dystonia - the goal is to restore and maintain neck range of motion and a long-term home exercise program should be utilized.
- Trismus - Literature is limited but a variety of jaw-opening devices are available to help treat trismus.
Resources[edit | edit source]
Radiation Side Effects Worksheet http://www.cancer.org/acs/groups/content/@nho/documents/document/acsq-009503.pdf
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Radiopedia Radiation Therapy Available from:https://radiopaedia.org/articles/radiation-therapy (last accessed 25.8.2020)
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 Goodman CC, Fuller KS. Pathology: Implications for the Physical Therapist. 3rd ed. St. Louis. Missouri: Saunders, 2009.
- ↑ 3.0 3.1 Stubblefield MD. Radiation Fibrosis Syndrome: Neuromuscular and Musculoskeletal Complications in Cancer Survivors. PM R. 2011;3:1041-1054.
- ↑ Radiopedia CRT Available from:https://radiopaedia.org/articles/conventional-radiation-therapy?lang=gb (last accessed 25.8.2020)
- ↑ 5.0 5.1 5.2 5.3 5.4 National Cancer Institute. Radiation Therapy for Cancer. National Institutes of Health. http://www.cancer.gov/cancertopics/factsheet/Therapy/radiation. Reviewed May 30, 2010. Accessed April 3, 2013.
- ↑ 6.0 6.1 ACS Radiation Therapy Available from:https://www.cancer.org/treatment/treatments-and-side-effects/treatment-types/radiation/effects-on-different-parts-of-body.html (last accessed 26.8.2020)
- ↑ Oncolink RFS Available from:https://www.oncolink.org/cancers/head-and-neck/side-effect-management-support-resources/radiation-fibrosis-syndrome (last accessed 26.8.2020)