Low Back Pain and Pregnancy: Difference between revisions
Kim Jackson (talk | contribs) m (Text replacement - "''' ==" to "==") |
m (reference hyperlinked, formatting text re arrangement) |
||
| (20 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editors ''' - [[User:Timothy Assi|Timothy Assi]] | '''Original Editors ''' - [[User:Timothy Assi|Timothy Assi]] | ||
| Line 5: | Line 4: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} <br> | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} <br> | ||
</div> | </div> | ||
== Definition | == Definition == | ||
<div> | <div> | ||
Pregnancy related low back pain is a common complaint that occurs in | Pregnancy related low back pain is a common complaint that occurs in 20–90% of pregnancies<ref name="Mogren et al">Weis CA, Barrett J, Tavares P, Draper C, Ngo K, Leung J, Huynh T, Landsman V. [https://www.sciencedirect.com/science/article/abs/pii/S1701216317307363 Prevalence of low back pain, pelvic girdle pain, and combination pain in a pregnant Ontario population.] Journal of Obstetrics and Gynaecology Canada. 2018 Aug 1;40(8):1038-43.</ref> and can be defined as pain between the 12th rib and the gluteal folds/pubic symphysis during the course of pregnancy, possibly radiating to the posterolateral thigh, the knee, and the calf but not to the foot<ref name="Mogren et al" />This pain is not the result of a known pathology such as disc herniation and can begin at any point during pregnancy. Although most cases are mild, approximately one-third of women experience severe pain.<ref name="Hall et al">Robey JH, Boyle K. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3811731/ The role of prism glass and postural restoration in managing a collegiate baseball player with bilateral sacroiliac joint dysfunction: A case report.] International Journal of Sports Physical Therapy. 2013 Oct;8(5):716.</ref> Pregnancy-related low back pain has been coined multiple times and can be referred to as one of the following : [[Low Back Pain]] (LBP), Peripartum Posterior Pelvic Pain (PPPP), Pregnancy-related low back pain (PLBP) or [http://www.physio-pedia.com/Pregnancy_Related_Pelvic_Pain pregnancy-related pelvic girdle pain (PPGP)]. The last two patterns can occur separately or combined.<ref name="Mogren et al" /> | ||
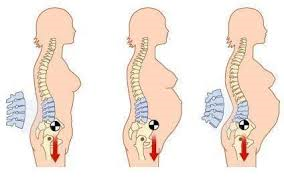
<div></div>[[ | <div></div><div>[[File:Definition1.png|200x200px]]<br> <br> | ||
<br> | ''Figure A ''<ref name="Perkins et al">Perkins J, Hammer RL, Loubert PV. [https://deepblue.lib.umich.edu/bitstream/handle/2027.42/90043/j.1542-2011.1998.tb03313.x.pdf?sequence=1&isAllowed=y Identification and management of pregnancy-related low back pain]. Journal of nurse-midwifery. 1998 Sep 1;43(5):331-40.</ref><br> | ||
</div></div> | |||
Unfortunately, there is limited research available regarding physical therapy intervention for pregnant women experiencing | Unfortunately, there is limited research available regarding physical therapy intervention for pregnant women experiencing LBP, so a homogenous approach tends to be used. However, back pain is not homogenous; therefore special considerations and precautions should be taken when treating this population. | ||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
The [http://www.physio-pedia.com/Anatomy lumbar region] is | The [http://www.physio-pedia.com/Anatomy lumbar region] is composed of [http://www.physio-pedia.com/Lumbosacral_Biomechanics five unique vertebrae] that are designed to withstand increased weight and retain a lordotic curve. The vertebral canal of the lumbar region houses the tail end of the spinal cord and the [[Cauda Equina Syndrome|cauda equina]]. | ||
To maintain stability and provide support, the lumbar region is connected and held secure by an intricate web of ligaments: the ligamentum longitudinale anterior and superior, the ligamentum flava, the ligamentum interspinata,the ligamentum intertransversarium and, the ligamentum supraspinale. All the mentioned ligaments provides stability, whereas the longitudinal ligamentattachesd to the intervertebral disc in order to keep the discs in position. Additionally, the lumbar region is supported by strong low back muscles, pelvic muscle,s an, abominal muscles. | |||
== Epidemiology == | |||
A number of reviews investigated the prevalence of low-back pain during pregnancy in different populations. The results are inconsistent, ranging from 8% to more than 89% of women who complain of low back pain during pregnancy. The prevalence of pregnancy related low-back pain is the highest during the third trimester.<ref name="Ansari et al">Ansari NN, Hasson S, Naghdi S, Keyhani S, Jalaie S. [https://www.tandfonline.com/doi/abs/10.3109/09593980802664968 Low back pain during pregnancy in Iranian women: Prevalence and risk factors]. Physiotherapy theory and practice. 2010 Jan 1;26(1):40-8.</ref><ref name="Bekkering">Bekkering GE, Hendriks HJ, Koes BW, Oostendorp RA, Ostelo RW, Thomassen JM, Van Tulder MW. [https://www.sciencedirect.com/science/article/pii/S0031940605605792 Dutch physiotherapy guidelines for low back pain. Physiotherapy.] 2003 Feb 1;89(2):82-96.</ref> The discomfort starts mostly between the fifth and seventh msonth of pregnancy. The influence of the postural change and body weight rises at this moment. <ref name="Glinkowski et al">Glinkowski WM, Tomasik P, Walesiak K, Głuszak M, Krawczak K, Michoński J, Czyżewska A, Żukowska A, Sitnik R, Wielgoś M. [https://journals.viamedica.pl/ginekologia_polska/article/view/48615 Posture and low back pain during pregnancy]—3D study. Ginekologia Polska. 2016;87(8):575-80.[https://journals.viamedica.pl/ginekologia_polska/article/view/48615]</ref><ref name="Katonis et al" /> | |||
== Etiology == | |||
The cause of pregnancy related LBP can be due to a combination of mechanical, hormonal, circulatory and psychosocial factors.<ref name="Chang">Chang HY, Lai YH, Jensen MP, Shun SC, Hsiao FH, Lee CN, Yang YL. [https://onlinelibrary.wiley.com/doi/abs/10.1111/jan.12258 Factors associated with low back pain changes during the third trimester of pregnancy. Journal of advanced nursing.] 2014 May;70(5):1054-64.</ref><ref name="Katonis et al">Katonis P, Kampouroglou A, Aggelopoulos A, Kakavelakis K, Lykoudis S, Makrigiannakis A, Alpantaki K. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3306025/ Pregnancy-related low back pain]. Hippokratia. 2011 Jul;15(3):205.</ref><ref name="Glinkowski et al" /> | |||
== | === Mechanical === | ||
There are several possible mechanisms of injury which could be causing pregnancy related LBP. During pregnancy, changes occur in the facet joints, in the back muscles, and in ligaments. This is mainly caused by the increased release of the hormone relaxin,<ref name="Hall et al" /> which causes ligament laxity, and therefore can affect the stability of the spine and lead to back pain. | |||
During pregnancy, the enlarging gravid uterus changes the load and body mechanics. It’s shifts the centre of gravity forwards, increasing the stress on the lower back. Postural changes can be used to balance the anterior shift possibly causing an extra lordosis. This increases the natural inward curvature of the spine, which increases the mechanical strain on the lower back. It also puts an extra stress on the intervertebral disc, possibly causing a decreased height an overall compression of the spine. <ref name="Chang" /><ref name="Katonis et al" /><br> | |||
The cause | Another contributor is the increase in weight that comes with pregnancy. On average, about 11-15 kilograms are gained during pregnancy. The weight gain increases the amount of force placed across joints, changes the center of gravity, and forces the patient into an anterior pelvic tilt. The anterior displacement of the [[Centre of Gravity|center of gravity]] will cause women to shift their heads and upper body posteriorly over the pelvis, causing [http://www.physio-pedia.com/Low_Back_Pain_Related_to_Hyperlordosis hyperlordosis] of the lumbar spine. This in turn, places additional stress on the intervertebral discs, ligaments, and facet joints and can lead to joint inflammation.<ref name="Wong">To WW, Wong MW. [https://www.tandfonline.com/doi/abs/10.1046/j.1600-0412.2003.00235.x Factors associated with back pain symptoms in pregnancy and the persistence of pain 2 years after pregnancy.] Acta obstetricia et gynecologica Scandinavica. 2003 Jan 1;82(12):1086-91.</ref> In addition, abdominal muscles are stretched and weakened, and the added weight can compress on the [[Lumbosacral Biomechanics|lumbosacral plexus]]. | ||
<br>The abdominal muscles also stretch to accommodate the expanding uterus. As they stretch, the muscles become tired and lose their ability to maintain normal body posture, causing the lower back to support the majority of the increased weight of the torso. <ref name="Katonis et al" /><br> | |||
=== Hormonal === | |||
<br>A significant portion of women first experience pain during the first trimester of pregnancy. At that moment mechanical changes do not yet play a significant role in the onset of pain. This suggests that hormonal changes during pregnancy can cause inflammation and pain in the back. It has been suggested that the hormone relaxin increases 10-fold in concentration during pregnancy, softening the collagen and causes ligamentous laxity and discomfort. The sacroiliac ligaments, but also other ligaments who surround the pelvic girdle become loose. This causes a decrease in the stability and brings on a potential strain in the pelvic girdle and low back area. | <br>A significant portion of women first experience pain during the first trimester of pregnancy. At that moment mechanical changes do not yet play a significant role in the onset of pain. This suggests that hormonal changes during pregnancy can cause inflammation and pain in the back. It has been suggested that the hormone relaxin increases 10-fold in concentration during pregnancy, softening the collagen and causes ligamentous laxity and discomfort. The sacroiliac ligaments, but also other ligaments who surround the pelvic girdle become loose. This causes a decrease in the stability and brings on a potential strain in the pelvic girdle and low back area. <ref name="Chang" /><ref name="Katonis et al" /><ref name="Glinkowski et al" /><br> | ||
=== Circulatory === | |||
<br>The expanding uterus can press on the vena cava, particularly at night when the patient is lying down. The pain is possibly severe enough to wake the patient up. This combined with the increased fluid volume from fluid retention during pregnancy leads to venous congestion and hypoxia in the pelvic and lumbar spine. | <br>The expanding uterus can press on the vena cava, particularly at night when the patient is lying down. The pain is possibly severe enough to wake the patient up. This combined with the increased fluid volume from fluid retention during pregnancy leads to venous congestion and hypoxia in the pelvic and lumbar spine. <ref name="Katonis et al" /> | ||
=== Psychosocial Factors === | |||
<br>Psychosocial factors can also increase low back pain. Pain-related catastrophizing, depression, pain intensity and time result in an increases in pain interference. The findings support the potential utility of the biopsychosocial model. Pain catastrophizing can be considered as a risk factor in the third trimester of pregnancy. <ref name="Chang" /> | <br>Psychosocial factors can also increase low back pain. Pain-related catastrophizing, depression, pain intensity and time result in an increases in pain interference. The findings support the potential utility of the biopsychosocial model. Pain catastrophizing can be considered as a risk factor in the third trimester of pregnancy. <ref name="Chang" /> | ||
=== <u></u>Risk Factors === | |||
Several factors have been associated with the development of low back pain during pregnancy. More specifically, laborious work, a history of low back pain before pregnancy, and a previous history of pregnancy-related low back pain have been identified as risk factors for the development of pregnancy-related low back pain. Pain syndromes during pregnancy impact the abdominopelvic musculoskeletal system, thereby causing abnormal strain on the axial low back elements. <ref name="Shah et al">Shah S, Banh ET, Koury K, Bhatia G, Nandi R, Gulur P. [https://downloads.hindawi.com/archive/2015/987483.pdf Pain management in pregnancy: multimodal approaches.] Pain research and treatment. 2015;2015.</ref> | |||
{| width="500" border="1" cellpadding="1" cellspacing="1" | {| width="500" border="1" cellpadding="1" cellspacing="1" | ||
|- | |- | ||
! scope="col" | Risk factors | ! scope="col" | Risk factors | ||
! scope="col" | No risk factors | ! scope="col" | No risk factors | ||
|- | |- | ||
| LBP history | | LBP history | ||
| Line 80: | Line 86: | ||
|} | |} | ||
<br>There is relative agreement in literature that excessive body weight may be a risk factor for LBP during pregnancy however, there are studies claiming that being overweight is not a risk. The same goes for number of pregnancies before the current one. <ref name="Mogren et al" /><ref name="Chang" /><ref name="Katonis et al" /> | |||
[[Image:Pregnancy.png|left]] | == Clinical Presentation <span> </span> == | ||
[[Image:Pregnancy.png|left]] | |||
<br>The most common onset tends to be during the | === Onset === | ||
<br>The most common onset tends to be during the fifth and sixth month of pregnancy, and the pain is usually worse in the evening. Often, the onset of pain occurs around the 18th week and reaches peak intensity between the 24th and 36th week of pregnancy. The pain can spontaneously disappear within 3 months, but 7-8% of the patients have a persisting, chronic pain. However it may start as early as the first trimester or be delayed as late s 3 weeks after delivery. <ref name="Verstraete et al">Verstraete EH, Vanderstraeten G, Parewijck W. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3987347/ Pelvic Girdle Pain during or after Pregnancy: a review of recent evidence and a clinical care] path proposal. Facts, views & vision in ObGyn. 2013;5(1):33.</ref> <ref name="Wu et al">Wu WH, Meijer OG, Uegaki K, Mens JM, Van Dieen JH, Wuisman PI, Östgaard HC. https://link.springer.com/article/10.1007/s00586-003-0615-y. European Spine Journal. 2004 Nov;13:575-89.</ref><ref name="Gutke et al">Gutke A, Östgaard HC, Öberg B. [https://journals.lww.com/spinejournal/Abstract/2006/03010/Pelvic_Girdle_Pain_and_Lumbar_Pain_in_Pregnancy__A.24.aspx Pelvic girdle pain and lumbar pain in pregnancy: a cohort study of the consequences in terms of health and functioning.] Spine. 2006 Mar 1;31(5):E149-55.</ref> | |||
< | About 67% of women experience pain at night. Factors that aggravate the pain include: standing, sitting, coughing or sneezing, walking, and straining during a bowel movement.<ref name="Wong" /> However pain and a disability of the lumbopelvic region are usually proven to be experienced as mild to moderate, except for a minor part (20%) of the pregnant women that will describe the pain as severe.<ref name="Mens and Huis">Mens JM, Huis YH, Pool-Goudzwaard A. [https://www.sciencedirect.com/science/article/pii/S1356689X11002463 Severity of signs and symptoms in lumbopelvic pain during pregnancy.] Manual therapy. 2012 Apr 1;17(2):175-9.</ref> | ||
The localization of pain is deep. It’s even possible that localization of the pain changes over time. | === Area and Quality of Pain === | ||
The localization of pain is deep. It’s even possible that localization of the pain changes over time. Pelvic girdle pain has been described as “stabbing’’ , pain in the lower back as a “dull ache’’ and the pain in the thoracic spine is rather “burning’’. Other pain-descriptions are: shooting pain, feeling of oppression and a sharp twinge.<br>Pregnancy-related low back pain is characterized by a dull pain <ref name="Vermani et al">Vermani E, Mittal R, Weeks A. [https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1533-2500.2009.00327.x Pelvic girdle pain and low back pain in pregnancy: a review.] Pain Practice. 2010 Jan;10(1):60-71.</ref> and is more pronounced in forward flexion with associated restriction in spine movement and palpation of the erector spinae muscles exacerbates pain. <ref name="Ostgaard and Roos-Hansson">Östgaard HC, Roos-Hansson E, Zetherström G. [https://journals.lww.com/spinejournal/Abstract/1996/12010/Regression_of_Back_and_Posterior_Pelvic_Pain_After.13.aspx Regression of back and posterior pelvic pain after pregnancy.] Spine. 1996 Dec 1;21(23):2777-80.</ref> | |||
== Differential Diagnosis == | == Differential Diagnosis == | ||
Some other diagnoses that can be commonly mistaken for pregnancy related low back pain are: [http://www.physio-pedia.com/Sciatica Sciatica], [[Meralgia Paraesthetica|Meralgia Paresthetica]], thoracic/rib pain, [http://www.physio-pedia.com/Hip_Pain_%26_Mobility_Deficits hip pain], [http://www.physio-pedia.com/Coccygodynia coccygodynia], spontaneous abortions, [http://www.physio-pedia.com/Osteomyelitis osteomyelitis], [[Osteoarthritis in young people|osteoarthritis]] of spine or hip, [[Cauda Equina Syndrome]], Osteitis Condensans Ilii, metastatic cancers, and [http://www.physio-pedia.com/Diastasis_Recti Diastasis Rectus Abdominis]. Other more common differential diagnoses are: disc disease, facet joint involvement and [http://www.physio-pedia.com/Sacroiliac_Joint_Force_and_Form_Closure sacroiliac joint] involvement. It is important to be able to recognize the subtle differences and differentiate between the comorbidities.<ref name="Sandler" /><ref name="Vermani et al" /> | Some other diagnoses that can be commonly mistaken for pregnancy related low back pain are: [http://www.physio-pedia.com/Sciatica Sciatica], [[Meralgia Paraesthetica|Meralgia Paresthetica]], thoracic/rib pain, [http://www.physio-pedia.com/Hip_Pain_%26_Mobility_Deficits hip pain], [http://www.physio-pedia.com/Coccygodynia coccygodynia], spontaneous abortions, [http://www.physio-pedia.com/Osteomyelitis osteomyelitis], [[Osteoarthritis in young people|osteoarthritis]] of spine or hip, [[Cauda Equina Syndrome]], Osteitis Condensans Ilii, metastatic cancers, and [http://www.physio-pedia.com/Diastasis_Recti Diastasis Rectus Abdominis]. Other more common differential diagnoses are: disc disease, facet joint involvement and [http://www.physio-pedia.com/Sacroiliac_Joint_Force_and_Form_Closure sacroiliac joint] involvement. It is important to be able to recognize the subtle differences and differentiate between the comorbidities.<ref name="Sandler" /><ref name="Vermani et al" /> | ||
* ''' | * '''Disc Disease''' - Morning pain and stiffness, pain when weight bearing, pain with increased abdominal pressure, history of repeated micro trauma, pain when going uphill, pain with prolonged sitting, pain with sit to stand activity. Sleep is usually undisturbed, pain eases as day progresses and then gets worse again, movement eases pain but not for long (e.g. fidgets).”<ref name="Sandler" /> | ||
* ''' | * '''Facet Joint Involvement''' - Non weight bearing pain, pain with related to movement (specifically rotation), pain increased by lateral compression, history of minor injury, pain is not usually referred to an extremity, pain eases with rest, not affected by coughing or sneezing”<ref name="Sandler" /> | ||
* ''' | * '''Sacroiliac Involvement''' - Pain is usually unilateral and does not midline, can refer to lower extremities, turning while in supine provokes pain, getting out of the car provokes pain, pain is referred to the groin or genitals, pain is related to menstruation prior to pregnancy because of the effects of cyclic hormones on pre-pregnant SIJ ligaments.”<ref name="Sandler" /> | ||
It is also important to differentiate between pregnancy-related low back pain (PLBP) and pregnancy-related pelvic girdle pain (PPGP), as the management and prognosis of the two conditions may differ. | It is also important to differentiate between pregnancy-related low back pain (PLBP) and pregnancy-related pelvic girdle pain (PPGP), as the management and prognosis of the two conditions may differ. Useful methods of differentiation include the site of pain, its character and severity, provoking factors, resultant disability, and the pain provocation tests. Recommended provocation tests are the posterior pelvic pain provocation test, Patrick’s Faber test, and the long dorsal sacroiliac ligament test. <ref name="Vleeming et al" /> In PPGP, the pain is typically concentrated under the posterior superior iliac spine, in the gluteal area, the posterior thigh, and the groin, meanwhile patients with PLBP show the pain to be concentrated in the lumbar region above the sacrum. <ref name="Vleeming et al">Vleeming A, Albert H, Ostgaard HC, Stuge B, Sturesson B. [https://pubmed.ncbi.nlm.nih.gov/18259783/ European guidelines on the diagnosis and treatment of pelvic girdle pain] [European Commission Research Directorate General Web site]. 2005. Available online at: www. backpain europe. org, accessed April. 2008.</ref> | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
In order to formulate the correct diagnosis, the patient should be questioned about her past medical history. It is important to concentrate on experienced symptoms, limitations in activities, and movement possibilities. Questions about past pregnancies such as – "Have you experienced any complications with prior pregnancy | In order to formulate the correct diagnosis, the patient should be questioned about her past medical history. It is important to concentrate on experienced symptoms, limitations in activities, and movement possibilities. Questions about past pregnancies such as – "Have you experienced any complications with prior pregnancy/ies?" are appropriate. This will help the therapist understand the patient’s health problems and needs. Knowledge of the anatomical and functional disorders, activity limitations and restriction of participation will help the therapist determine her/his role and the need for appropriate interventions. It is important to recognize red flag complaints and contact a doctor to seek further investigation, if they are present.<ref name="Bekkering" /><br> | ||
It is important at the time of initial assessment to differentiate between the lumbar spine and pelvic dysfunction. This can be done during the subjective by inquiring about aggravating factors. Activities such as turning in bed, getting out of a car, walking and climbing stairs may indicate that the origin of pain may be due to [[Pelvic Floor Dysfunction - A patient guide.|pelvic dysfunction]]. This can then be confirmed with a range of tests for assessing the sacroiliac joint and pubic symphysis. | |||
== Outcome Measures == | == Outcome Measures == | ||
Several validated instruments to assess back pain exist for general population who can be used in the diagnosis to estimate the complaints more objectively: | Several validated instruments to assess back pain exist for general population who can be used in the diagnosis to estimate the complaints more objectively: | ||
* [[Visual Analogue Scale|Visual Analogue Scale (VAS)]] | * [[Visual Analogue Scale|Visual Analogue Scale (VAS)]] | ||
* [[Roland‐Morris Disability Questionnaire|Roland Disability Questionnaire (RDQ)]] | * [[Roland‐Morris Disability Questionnaire|Roland Disability Questionnaire (RDQ)]] | ||
* Québec Pain disability index (QPDI) <ref name="Mens Jan">Mens, | * Québec Pain disability index (QPDI) <ref name="Mens Jan">Mens JM, Vleeming A, Snijders CJ, Ronchetti I, Ginai AZ, Stam HJ. Responsive[https://journals.lww.com/spinejournal/Abstract/2002/05150/Responsiveness_of_Outcome_Measurements_in.19.aspx ness of outcome measurements in rehabilitation of patients with posterior pelvic pain since pregnancy.] Spine. 2002 May 15;27(10):1110-5.</ref> | ||
* PHotograph series Of Daily Activities (PHODA) | * PHotograph series Of Daily Activities (PHODA) | ||
* Impact on Participation and Autonomy (IPA) | * Impact on Participation and Autonomy (IPA) | ||
* Pain Behavior Scale (PBS) | * Pain Behavior Scale (PBS) | ||
* [[Oswestry Disability Index]]. <ref name="Glinkowski et al" /><br> | * [[Oswestry Disability Index]]. <ref name="Glinkowski et al" /><br> | ||
<br>Due to a lack of pregnancy-specific outcome measures, a pregnancy-specific self-report questionnaire assessing mobility in relation to both back and pelvic pain, called the [https://obgyn.onlinelibrary.wiley.com/doi/10.1080/00016340500456373 Pregnancy Mobility Index] (PMI), was developed and validated. Van De Pol et al. developed the Pregnancy Mobility Index (PMI) to assess the ability of doing normal household activities. The patient can answer on a scale from ‘no problem’ to ‘impossible’ or ‘only with aid of others’. The PMI is used to evaluate the mobility and quality of life of pregnant women who suffer from LBP. <ref name="Van De Pol et al">Van De Pol, G., et al. The Pregnancy [https://www.tandfonline.com/doi/abs/10.1080/00016340500456373 Mobility Index: a mobility scale during and after pregnancy]. Acta obstetricia et gynecologica Scandinavica 85.7 (2006): 786-791. (Evidence level: 2B)</ref> | |||
== Examination == | == Examination == | ||
<div> | <div> | ||
During an examination of a pregnant patient, positioning is a key consideration. Excessive time in supine is not recommended due to the weight of the uterus on the vena cava and vital structures.<ref name="Sandler"> | During an examination of a pregnant patient, positioning is a key consideration. Excessive time in supine is not recommended due to the weight of the uterus on the vena cava and vital structures.<ref name="Sandler">Östgaard HC, Roos-Hansson E, Zetherström G. [https://journals.lww.com/spinejournal/Abstract/1996/12010/Regression_of_Back_and_Posterior_Pelvic_Pain_After.13.aspx Regression of back and posterior pelvic pain after pregnancy]. Spine. 1996 Dec 1;21(23):2777-80.</ref> Based on the level of pain and disability of the patient, and potentially the size of the pregnant abdomen, certain tests and measures may need to be modified for this population.Excessive time in supine is not recommended due to the weight of the uterus on the vena cava and vital structures.<ref name="Sandler" /> | ||
</div> | </div> | ||
==== | ===Physical Exam=== | ||
<br>Examination should include observation of the posture and gait, neurologic screen to rule out underlying pathology, range of motion, muscle tests, palpation, muscle length tests, and assessment of joint mobility. | |||
<div>The [[Straight Leg Raise Test|Active Straight Leg Raise test]] can prove that patients suffering from LBP use significantly more muscle activity, but produce less force, compared to the healthy groups. Healthy controls achieve more hip flexion force at both 0 and 20 cm than PLBP.<ref name="Mirthe et al">de Groot M, Pool-Goudzwaard AL, Spoor CW, Snijders CJ. [https://www.sciencedirect.com/science/article/pii/S1356689X06001482 The active straight leg raising test (ASLR) in pregnant women: differences in muscle activity and force between patients and healthy subjects]. Manual Therapy. 2008 Feb 1;13(1):68-74.</ref><ref name="Roussel et al">Roussel NA, Nijs J, Truijen S, Smeuninx L, Stassijns G. [https://www.sciencedirect.com/science/article/pii/S0161475407000735 Low back pain: clinimetric properties of the Trendelenburg test, active straight leg raise test, and breathing pattern during active straight leg raising.] Journal of manipulative and physiological therapeutics. 2007 May 1;30(4):270-8.</ref><br>It’s important to distinguish posterior pelvic pain from low back pain during physical examination. Recommended provocation tests are the [[Posterior Pelvic Pain Provocation Test|Posterior Pelvic Pain Provocation (PPPP) test]], [[FABER Test|FABER test,]] long dorsal sacroiliac ligament test and standing on one leg. As mentioned above, the pain is typically concentrated under the posterior superior iliac spine, in the gluteal area, the posterior thigh and the groin in case of PPGP. Patients with PLBP show pain concentrated in the lumbar region above the sacrum. <ref name="Mens et al">Mens JM, Huis YH, Pool-Goudzwaard A. [https://www.sciencedirect.com/science/article/pii/S1356689X12000082 The Active Straight Leg Raise test in lumbopelvic pain during pregnancy.] Manual therapy. 2012 Aug 1;17(4):364-8.</ref><ref name="Vleeming et al" /> Palpation over soft tissue of the sacroiliac, pubic symphysis, and gluteal regions can also distinguish pelvic pain from tenderness over the back above the waist. Studies show that both methods are effective although pain provocation tests are more reliable than palpation tests. | |||
</div><div>The [[Trendelenburg Sign|Trendelenberg sign]] examine the ability of the lower back, pelvis and hip to transfer load unilaterally in a weight-bearing position. The test occurs positive when the patient drops the pelvis on the non stance side. In this case the patient has weakness of the abductor muscles. <ref name="Roussel et al" /> The following findings are commonly revealed: Paravertebral muscles are tender to palpation, back muscles weakness, decreased ROM in flexion. The description of the pain is often not localized and may be intermittent. It is possible for the pain to radiate down as far as the calf.</div> | |||
</div> | |||
==== | ==== Modified Tests ==== | ||
< | Some tests cannot be performed as per usual given the patient's growing abdomen therefore the following modifications are needed.<ref name="Cullaty">Cullaty M. [https://journals.lww.com/jwphpt/Pages/default.aspx Suspected sacroiliac joint dysfunction: modifying examination and intervention during pregnancy.] Journal of Women’s Health Physical Therapy. 2006 Jul 1;30(2):18-24.</ref><br><div>[[Image:Modified Hip Flexor Assessment small.jpg|left|150x190px|Figure B: Walk B. Texas State University's Evidence-based Practice project.]]</div>'''<u><br></u>''' | ||
<u>Hip Flexor Length:</u> To modify the test position of the [http://www.physio-pedia.com/Thomas_Test ‘Thomas Test’] the patient will have to sit on the edge of a table or mat, and extend the test leg as much as possible, while maintaining slight knee flexion. The pelvis should be kept in a neutral alignment. A patient with non-impaired flexibility should be able to extend her hip perpendicular to the floor. | |||
<u>SI Joint Examination:</u> If the patient is unable to stand, instruct the patient to lie in supine and perform a pelvic bridge. The bridge will place the pelvis in neutral - the ASIS’ can be palpated for symmetry.'''''<br>'''<br>'' | <u>SI Joint Examination:</u> If the patient is unable to stand, instruct the patient to lie in supine and perform a pelvic bridge. The bridge will place the pelvis in neutral - the ASIS’ can be palpated for symmetry.'''''<br>'''<br>'' | ||
Figure B: Walk B. Texas State University's Evidence-based Practice project. | |||
== Medical Management == | == Medical Management == | ||
It is important to encourage the patient to receive regular checkups by her obstetrician. During the therapy session, continually check on pain levels and any aches radiating from the low back or stomach. Some patients tolerate pain and discomfort better than others and will therefore mask their distress – Use a chart for Rate of Perceived Exertion to determine the patient's true status and take note of any changes that occur between the begging and end of the session. | It is important to encourage the patient to receive regular checkups by her obstetrician. During the therapy session, continually check on pain levels and any aches radiating from the low back or stomach. Some patients tolerate pain and discomfort better than others and will therefore mask their distress – Use a chart for Rate of Perceived Exertion to determine the patient's true status and take note of any changes that occur between the begging and end of the session. | ||
Although there are numerous interventions promoted for low back pain during pregnancy, the most common and widely used is a specific exercise program designed by a physical/physiotherapist (see below)<ref name="Stuge et al" / | Although there are numerous interventions promoted for low back pain during pregnancy, the most common and widely used is a specific exercise program designed by a physical/physiotherapist (see below)<ref name="Stuge et al">Stuge B, Hilde G, Vøllestad N. [https://www.tandfonline.com/doi/abs/10.1080/j.1600-0412.2003.00125.x Physical therapy for pregnancy-related low back and pelvic pain: a systematic review]. Acta obstetricia et gynecologica Scandinavica. 2003 Jan 1;82(11):983-90.</ref> <ref name="Snijders et al">Mens JM, Snijders CJ, Stam HJ. [https://academic.oup.com/ptj/article/80/12/1164/2842429 Diagonal trunk muscle exercises in peripartum pelvic pain:] a randomized clinical trial. Physical therapy. 2000 Dec 1;80(12):1164-73.</ref>. Another intervention that is getting tractions and shows prominent research is acupuncture. Recent studies show that a week of continuous acupuncture at specific auricular points can decrease pain and increase the capacity for some physical activity which can help diminish the need for drugs.<ref name="Wang et al">Wang SM, DeZinno P, Lin EC, Lin H, Yue JJ, Berman MR, Braveman F, Kain ZN. [https://www.sciencedirect.com/science/article/pii/S0002937809004244 Auricular acupuncture as a treatment for pregnant women who have low back and posterior pelvic pain: a pilot study]. American journal of obstetrics and gynecology. 2009 Sep 1;201(3):271-e1.</ref><br> | ||
===Other Interventions=== | |||
* | * Side lying while sleeping or resting using a wedge shaped pillow to support stomach | ||
* | * Use of pillow between the legs while side lying (squeeze the pillow/legs together while rolling) | ||
* | * Compression socks to promote venous return and decrease edema | ||
* | * Support belt (The Love Comfort support belt is covered by Medicaid) <ref name="Sandler" /> | ||
* | * Soft tissue [[massage]] | ||
* | * Acetaminophen as prescribed by physician | ||
* | * Yoga | ||
* [http://www.physio-pedia.com/Aquatherapy | * [http://www.physio-pedia.com/Aquatherapy Aquatherapy]<ref name="Granath et al">Granath AB, Hellgren MS, Gunnarsson RK, Water aerobics reduces sick leave due to low back pain during pregnancy. J Obstet Gynecol Neonatal Nurs. 2006 Jul-Aug;35(4):465-71 (Evidence level: 1B)</ref> | ||
Intra-articular sacroiliac joint injections (under imaging guidance) for ankylosing spondylitis can be recommended. There are indications that acupuncture during pregnancy may reduce pain, but high quality studies are required for sacroiliac joint therapeutic injection therapy. <ref name="Vleeming et al" /> | * Intra-articular sacroiliac joint injections (under imaging guidance) for ankylosing spondylitis can be recommended. There are indications that acupuncture during pregnancy may reduce pain, but high quality studies are required for sacroiliac joint therapeutic injection therapy. <ref name="Vleeming et al" /> <ref name="Shah et al" /> | ||
* Most therapeutic strategies encourage preventive measures among pregnant women and those who are planning to become pregnant. It has been shown that women who participate in prophylactic education and strengthening programs during early pregnancy can avoid problems from low back pain. | |||
Most therapeutic strategies encourage preventive measures among pregnant women and those who are planning to become pregnant. It has been shown that women who participate in prophylactic education and strengthening programs during early pregnancy can avoid problems from low back pain. < | == Physical Therapy Management == | ||
<div>When treatment is necessary for low back pain, conservative management is the ideal option. Treatment starts with education and activity adjustments. Educational strategies focus on back care measures, such as ergonomics, which teaches women correct posture; pregnant women learn how to stand, walk, or bend properly, without causing stress on the spine. Accurate posture is essential to improve low back pain. Braces that ensure correct body posture are also available if the instructions are not enough. In regard to activity modifications, scheduled rest during the day is helpful for relieving muscle spasms and acute pain. During this time, posture is again important as both feet should be elevated, which will help flex the hips and decrease the lumbar lordosis of the spine. <ref name="Shah et al" /> <ref name="Borg-Stein et al">Borg-Stein J, Dugan SA. [https://www.sciencedirect.com/science/article/pii/S1047965107000496 Musculoskeletal disorders of pregnancy, delivery and postpartum.] Physical medicine and rehabilitation clinics of North America. 2007 Aug 1;18(3):459-76.</ref> | |||
When treatment is necessary for low back pain, conservative management is the ideal option. Treatment starts with education and activity adjustments. Educational strategies focus on back care measures, such as ergonomics, which teaches women correct posture; pregnant women learn how to stand, walk, or bend properly, without causing stress on the spine. Accurate posture is essential to improve low back pain. Braces that ensure correct body posture are also available if the instructions are not enough. In regard to activity modifications, scheduled rest during the day is helpful for relieving muscle spasms and acute pain. During this time, posture is again important as both feet should be elevated, which will help flex the hips and decrease the lumbar lordosis of the spine. <ref name="Shah et al" /> | Studies have found that pregnant women with low back pain, who participate in both education and physical therapy, have less pain and disability, higher quality of life, and improvement on physical tests. Physical therapy encompasses several factors such as postural modifications, back strengthening, stretching, and self-mobilization techniques. Functional stability can be maintained throughout pregnancy by strengthening the muscles around the lumbar spine through various back exercises. <ref name="Shah et al" /> <ref name="Borg-Stein et al" /> | ||
Treatment depends on the diagnosis and timing of pregnancy (before or after childbirth). The patient should understand her own symptoms and be motivated to remain active. | |||
</div> | </div> | ||
==== | === Red Flags === | ||
The following are crucial to identify during treatments:<ref name="Perkins et al" /> | |||
* Vaginal bleeding | |||
* Dizziness/feeling faint | |||
* Shortness of breath | |||
* Chest pain | |||
* Headache | |||
* Muscles weakness | |||
* Calf pain or swelling | |||
* Uterine contractions | |||
* Decreased fetal movement | |||
* Vaginal fluid leakage | |||
* Neurological symptoms | |||
==== | == Physical Therapy Goals == | ||
<div> | The focus of physiotherapy is to:<div> | ||
* Restore [http://www.physio-pedia.com/Lumbosacral_Biomechanics biomechanics] during daily activities | * Restore [http://www.physio-pedia.com/Lumbosacral_Biomechanics biomechanics] during daily activities | ||
* | * Improve lumbo-pelvic stabilization | ||
* | * Educate and prevent<ref name="Stuge et al" /></div>Physical therapy should be focused on the following strategies<ref name="Haugland et al">Beales DJ, O'Sullivan PB, Briffa NK. [https://www.sciencedirect.com/science/article/pii/S1356689X09001908 The effects of manual pelvic compression on trunk motor control during an active straight leg raise in chronic pel]vic girdle pain subjects. Manual therapy. 2010 Apr 1;15(2):190-9.</ref> | ||
</div> | |||
1) Patient Instructions | |||
= | <br>It’s important to communicate with the patient and provide information about the relevant anatomy, ergonomics, [http://www.physio-pedia.com/Back_Education_Program back education] (to prevent unnecessary mechanical stress on the back), and how to manage ADL activities (walking, standing, sitting, lying, and work position, learning how to control pain). Research shows that when the symptoms are explained, patients can feel more at ease and their anxiety may decrease. | ||
* Using a small pillow between the legs while sitting and rolling in order to stabilize the back. | |||
* Postural correction by standing upright with a neutral posture, avoiding hyperlordosis | |||
* Do not sit or stand for a long time, alternate it with walking or stretching | |||
* Taking breaks and resting in a comfortable position, with the back supported to relieve tired muscles | |||
* Sleeping lying on one side with the top leg on a pillow | |||
* “Use of a small footstool for one foot in sitting or standing, alternate feet”<ref name="Haugland et al" /> | |||
* Avoiding spine twisting while lifting | |||
2) Active Back Exercises | |||
Even though most pregnant patients will be advised to exercises within their safe and pain free range, studies show that less than 50% will actually do so. <ref name="George et al">George JW, Skaggs CD, Thompson PA, Nelson DM, Gavard JA, Gross GA. [https://www.sciencedirect.com/science/article/pii/S0002937812019692 A randomized controlled trial comparing a multimodal intervention and standard obstetrics care for low back and pelvic pain in pregnancy.] American journal of obstetrics and gynecology. 2013 Apr 1;208(4):295-e1.</ref>. Furthermore it has also been proven that training the rectus abdominus muscles will be useless due to his weakness during the pregnancy. | |||
<br>Stability, coordination and functional preservation should be trained with [http://www.physio-pedia.com/Back_Education_Program active back exercises] – endurance training for back muscles stabilization. Pelvic tilts, knee pull, straight leg raising, curl up, lateral straight leg raising and water aerobics are recommended because these exercises could relieves lumbar pain in pregnancy. Relaxation exercises while paying close attention to proper respiration also show to be beneficial. | |||
<br>Management includes specific interventions to address pain, weakness, and mobility in the low back region. The Ottawa Panel also recommends massage therapy in order to treat subacute and chronic low back pain. | |||
3) Manual Therapy Techniques | |||
{| width="100%" border="1" align="left" cellspacing="1" cellpadding="1" | |||
{| width=" | |||
|- | |- | ||
| Posterior/Anterior mobilizations in side lying position | | Posterior/Anterior mobilizations in side lying position | ||
| Addresses pain and mobility (Grades 1-4). | | Addresses pain and mobility (Grades 1-4). | ||
| | | | ||
[[Image:Modified PA Mob small.jpg|150x190px]] | [[Image:Modified PA Mob small.jpg|150x190px]] | ||
| Line 208: | Line 220: | ||
| <span style="line-height: 19.90625px;">Muscle Energy Technique by resisting hip flexion in side laying while stabilizing the sacrum</span> | | <span style="line-height: 19.90625px;">Muscle Energy Technique by resisting hip flexion in side laying while stabilizing the sacrum</span> | ||
| <span style="line-height: 19.90625px;">Corrects anterior innominate rotation. </span> | | <span style="line-height: 19.90625px;">Corrects anterior innominate rotation. </span> | ||
| | | | ||
[[Image:Hip Flexion Side-laying.png|200x160px]]<br> | [[Image:Hip Flexion Side-laying.png|200x160px]]<br> | ||
| Line 214: | Line 226: | ||
|- | |- | ||
| <span style="line-height: 19.90625px;">[http://www.physio-pedia.com/Spinal_Manipulation Spinal manipulation] | | <span style="line-height: 19.90625px;">[http://www.physio-pedia.com/Spinal_Manipulation Spinal manipulation](Level of evidence:2A)</span> | ||
| <span style="line-height: 19.90625px;">Are used to relax soft tissues</span> | | <span style="line-height: 19.90625px;">Are used to relax soft tissues</span> | ||
| | | | ||
|} | |} | ||
{| width="100%" border="1" align="left" cellspacing="1" cellpadding="1" | {| width="100%" border="1" align="left" cellspacing="1" cellpadding="1" | ||
|- | |- | ||
| <span style="line-height: 19.90625px;">Strengthening Gluteus | | <span style="line-height: 19.90625px;">Strengthening Gluteus Mediu</span> | ||
| | | | ||
<span style="line-height: 1.5em;">Position the patient in a side lying and place an elastic around both legs above the knees.</span> | <span style="line-height: 1.5em;">Position the patient in a side lying and place an elastic around both legs above the knees.</span> | ||
<span style="line-height: 1.5em;">Ask the patient to perform an external rotation of her leg in order to strengthen the Gluteus Medius. Perform this exercise on both sides. | <span style="line-height: 1.5em;">Ask the patient to perform an external rotation of her leg in order to strengthen the Gluteus Medius. Perform this exercise on both sides.</span> | ||
<span style="line-height: 1.5em;">Feet need to be kept together during the whole exercise. Also, prevent the pelvis from externally rotating.</span> | <span style="line-height: 1.5em;">Feet need to be kept together during the whole exercise. Also, prevent the pelvis from externally rotating.</span> | ||
| | | | ||
[[Image:Gluteus medius Strengthening.png|200x160px]] | [[Image:Gluteus medius Strengthening.png|200x160px]] | ||
| Line 238: | Line 248: | ||
|- | |- | ||
| <span style="line-height: 19.90625px;">Abdominal Drawing in Maneuver with Physioball (ADIM).</span> | | <span style="line-height: 19.90625px;">Abdominal Drawing in Maneuver with Physioball (ADIM).</span> | ||
| | | | ||
Ask the patient to sit on a physioball and simulate a walk movement with the lower extremities. This will encourage the back muscle memory to stabilize back during ADL's. | Ask the patient to sit on a physioball and simulate a walk movement with the lower extremities. This will encourage the back muscle memory to stabilize back during ADL's. | ||
<br>The patient will have to keep her back strait during the whole exercise. | <br>The patient will have to keep her back strait during the whole exercise. | ||
| | | | ||
[[Image:Abdominal Drawing.png|200x160px]] | [[Image:Abdominal Drawing.png|200x160px]] | ||
| Line 250: | Line 260: | ||
|- | |- | ||
| <span style="line-height: 19.90625px;">Latissimus dorsi pull-downs</span> | | <span style="line-height: 19.90625px;">Latissimus dorsi pull-downs</span> | ||
| | | | ||
The patient will be positioned on a physioball, which will force the pelvic, abdomen and back muscles to stay active in order to find a balanced sitting position. This part of the exercise will provoke a contraction of the glutei to increase the strength of the posterior oblique sling muscles which compress the SIJ.<br>In the meantime the patient will perform a latissimus dorsi pull-down by bringing the strait arms with the arms positioned in front and above the head to a position with flexed arms with the arms in front of the chest and bring the arms back to the prior position.<br>This second part of the exercise will improve the latissimus dorsi muscle strength. | The patient will be positioned on a physioball, which will force the pelvic, abdomen and back muscles to stay active in order to find a balanced sitting position. This part of the exercise will provoke a contraction of the glutei to increase the strength of the posterior oblique sling muscles which compress the SIJ.<br>In the meantime the patient will perform a latissimus dorsi pull-down by bringing the strait arms with the arms positioned in front and above the head to a position with flexed arms with the arms in front of the chest and bring the arms back to the prior position.<br>This second part of the exercise will improve the latissimus dorsi muscle strength. | ||
Keep the back straight during the whole exercise. | Keep the back straight during the whole exercise. | ||
| | | | ||
[[Image:Lat Pull Down.png|160x200px]] | [[Image:Lat Pull Down.png|160x200px]] | ||
| Line 261: | Line 271: | ||
|- | |- | ||
| <span style="line-height: 19.90625px;">Angry Cat | | <span style="line-height: 19.90625px;">Angry Cat (Level of evidence:5)</span> | ||
| <span style="line-height: 19.90625px;">Starting from the hands-and knees-position the patient will move her back up and down. </span><br><span style="line-height: 19.90625px;">During this exercise it is important to keep the arms stretched out with the hands positioned right under the shoulders and to keep the stomach muscles tight throughout the entire exercise.</span> | | <span style="line-height: 19.90625px;">Starting from the hands-and knees-position the patient will move her back up and down. </span><br><span style="line-height: 19.90625px;">During this exercise it is important to keep the arms stretched out with the hands positioned right under the shoulders and to keep the stomach muscles tight throughout the entire exercise.</span> | ||
| | | | ||
[[Image:Angry Cat.png|160x210px]] | [[Image:Angry Cat.png|160x210px]] | ||
''Figure H: <ref name="Stahmann" />(Level of evidence:5)'' | ''Figure H: <ref name="Stahmann">Stahmann Dilfer C. Your Baby, Your Body (Fitness during pregnancy) New York: Crown publishers, inc. 1977 (Evidence level: 5)</ref>(Level of evidence:5)'' | ||
|- | |- | ||
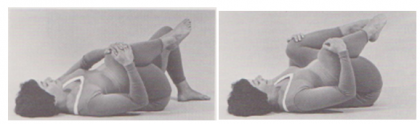
| <span style="line-height: 19.90625px;">Pelvic Tilt | | <span style="line-height: 19.90625px;">Pelvic Tilt (Level of evidence:5)</span> | ||
| <span style="line-height: 19.90625px;">Lay down with flexed knees and move the pelvic in an anterior and posterior position.</span> | | <span style="line-height: 19.90625px;">Lay down with flexed knees and move the pelvic in an anterior and posterior position.</span> | ||
| | | | ||
[[Image:Pelvic Tilt.png|200x150px]] | [[Image:Pelvic Tilt.png|200x150px]] | ||
| Line 284: | Line 294: | ||
|} | |} | ||
<br><br> | <br><br> | ||
<br> | |||
4) TENS | |||
< | There is no strong evidence on the benefits of Tens on Low back pain in pregnancy but it can be used as a supplementary therapy. It’s important to use a low intensity and avoid the acupuncture points which may induce throes. Precautions and contra-indications must be respected.<ref name="Vermani et al" /><ref name="Khadilkar et al">Khadilkar A, Odebiyi DO, Brosseau L, Wells GA. [https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD003008.pub3/full Transcutaneous electrical nerve stimulation (TENS) versus placebo for chronic low‐back pain.] Cochrane Database of Systematic Reviews. 2008(4).</ref> | ||
Patients should take caution when using ultrasound and electrical stimulation and avoid placing those modalities anywhere near the stomach or low back. | |||
5) Yoga | |||
<br>Yoga can effectively decrease low back pain intensity. <ref name="Martins et al">Martins, Roseny Flávia, and João Luiz Pinto e Silva. Treatment of pregnancy-related lumbar and pelvic girdle pain by the yoga method: a randomized controlled study. The Journal of Alternative and Complementary Medicine 20.1 (2014): 24-31. (Evidence level: 1B)</ref>(Level of evidence:1B)<br> | <br>Yoga can effectively decrease low back pain intensity. <ref name="Martins et al">Martins, Roseny Flávia, and João Luiz Pinto e Silva. Treatment of pregnancy-related lumbar and pelvic girdle pain by the yoga method: a randomized controlled study. The Journal of Alternative and Complementary Medicine 20.1 (2014): 24-31. (Evidence level: 1B)</ref>(Level of evidence:1B)<br> | ||
| Line 302: | Line 312: | ||
<br> | <br> | ||
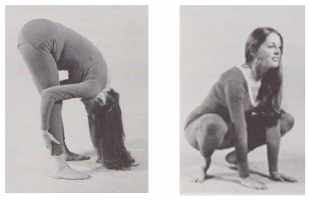
6) Stretching | |||
<br>''1. Lower Back Stretch:'' it is plausible that stretching lower back and hip extensor muscles can lead to increased lower back and pelvic flexibility. | |||
<br>''1. Lower Back Stretch:'' it is plausible that stretching lower back and hip extensor muscles can lead to increased lower back and pelvic flexibility.<br> | |||
[[Image:Low Back Stretch.png|420x180px]] | [[Image:Low Back Stretch.png|420x180px]] | ||
''Figure J + K: <ref name="Stahmann" /> | ''Figure J + K: <ref name="Stahmann" />Stahmann Dilfer C.; Your Baby, Your Body (Fitness during pregnancy); Crown publishers, inc., New York, 1977'<nowiki/>'''<br>''''' | ||
<span> </span><br> <u>Instructions:</u> | <span> </span><br> <u>Instructions:</u> | ||
# Clasp your fingers around your right knee. | # Clasp your fingers around your right knee. | ||
# Gently pull your knee as close to your chest as possible. Relax your lower back and try to let your glutes (butt) roll of the floor as you pull. | # Gently pull your knee as close to your chest as possible. Relax your lower back and try to let your glutes (butt) roll of the floor as you pull. | ||
| Line 335: | Line 346: | ||
# Try to keep your knees over your feet and slowly lower your gluts until you return to starting position. | # Try to keep your knees over your feet and slowly lower your gluts until you return to starting position. | ||
<br> | <br> | ||
7) Aerobic Exercises<div><br>Walking, swimming (Level of evidence: 1B),Tai chi, recumbent bicycle (or nu-step), are plausible to be beneficial at a low to moderate intensity. The stress on the back should be minimal.<ref name="Field">Field T., Prenatal exercise research, Infant Behavior & Development 35 (2012) 397– 407 (Evidence level: 2A)</ref>(Level of evidence:2A)</div><div></div>8) Home Exercises [[Image:Back Tuck Arch.png|right|120x230px]] | |||
<br>The exercises explained above could also be performed at home if both the patient and therapist feel confident that | <br>The exercises explained above could also be performed at home if both the patient and therapist feel confident that the exercises will be performed correctly without supervision. | ||
<br>Back tuck arch <ref name="Stahmann" /> | <br>Back tuck arch <ref name="Stahmann" />Lean with the back against the wall and alternate between anterior and posterior pelvic tilt. | ||
<br> | <br> | ||
| Line 371: | Line 381: | ||
We concluded there is a dearth in good quality research. Future studies should more concentrate on the specific low back pain of pregnant woman. | We concluded there is a dearth in good quality research. Future studies should more concentrate on the specific low back pain of pregnant woman. | ||
== Presentations == | |||
== | |||
{| class="FCK__ShowTableBorders" width="100%" border="0" cellspacing="4" cellpadding="4" | {| class="FCK__ShowTableBorders" width="100%" border="0" cellspacing="4" cellpadding="4" | ||
|- | |- | ||
| Line 392: | Line 395: | ||
|} | |} | ||
== References == | == References == | ||
| Line 401: | Line 403: | ||
[[Category:Lumbar Spine]] | [[Category:Lumbar Spine]] | ||
[[Category: | [[Category:Lumbar Spine - Conditions]] | ||
[[Category:Sacroiliac_Conditions]] | [[Category:Sacroiliac_Conditions]] | ||
[[Category:Womens_Health]] | [[Category:Womens_Health]] | ||
[[Category:Musculoskeletal/Orthopaedics]] | [[Category:Musculoskeletal/Orthopaedics]] | ||
[[Category:Pregnancy]] | [[Category:Pregnancy]] | ||
[[Category:Pelvis]] | |||
[[Category:Pelvis - Conditions]] | |||
[[Category:Conditions]] | |||
Latest revision as of 00:11, 30 June 2023
Original Editors - Timothy Assi
Top Contributors - Lynse Brichau, Aiko Deckers, Admin, Brenda Walk, Corin Arundale, Timothy Assi, Christine Utskot, Joanne Garvey, Kim Jackson, Lauren Lopez, Nicole Hills, Chris Slininger, Rachael Lowe, Temitope Olowoyeye, Joshua Samuel, Evan Thomas, Uchechukwu Chukwuemeka, Laura Ritchie, George Prudden, 127.0.0.1 and Jeremy Brady
Definition[edit | edit source]
Pregnancy related low back pain is a common complaint that occurs in 20–90% of pregnancies[1] and can be defined as pain between the 12th rib and the gluteal folds/pubic symphysis during the course of pregnancy, possibly radiating to the posterolateral thigh, the knee, and the calf but not to the foot[1]This pain is not the result of a known pathology such as disc herniation and can begin at any point during pregnancy. Although most cases are mild, approximately one-third of women experience severe pain.[2] Pregnancy-related low back pain has been coined multiple times and can be referred to as one of the following : Low Back Pain (LBP), Peripartum Posterior Pelvic Pain (PPPP), Pregnancy-related low back pain (PLBP) or pregnancy-related pelvic girdle pain (PPGP). The last two patterns can occur separately or combined.[1]
Unfortunately, there is limited research available regarding physical therapy intervention for pregnant women experiencing LBP, so a homogenous approach tends to be used. However, back pain is not homogenous; therefore special considerations and precautions should be taken when treating this population.
Clinically Relevant Anatomy[edit | edit source]
The lumbar region is composed of five unique vertebrae that are designed to withstand increased weight and retain a lordotic curve. The vertebral canal of the lumbar region houses the tail end of the spinal cord and the cauda equina.
To maintain stability and provide support, the lumbar region is connected and held secure by an intricate web of ligaments: the ligamentum longitudinale anterior and superior, the ligamentum flava, the ligamentum interspinata,the ligamentum intertransversarium and, the ligamentum supraspinale. All the mentioned ligaments provides stability, whereas the longitudinal ligamentattachesd to the intervertebral disc in order to keep the discs in position. Additionally, the lumbar region is supported by strong low back muscles, pelvic muscle,s an, abominal muscles.
Epidemiology[edit | edit source]
A number of reviews investigated the prevalence of low-back pain during pregnancy in different populations. The results are inconsistent, ranging from 8% to more than 89% of women who complain of low back pain during pregnancy. The prevalence of pregnancy related low-back pain is the highest during the third trimester.[4][5] The discomfort starts mostly between the fifth and seventh msonth of pregnancy. The influence of the postural change and body weight rises at this moment. [6][7]
Etiology[edit | edit source]
The cause of pregnancy related LBP can be due to a combination of mechanical, hormonal, circulatory and psychosocial factors.[8][7][6]
Mechanical[edit | edit source]
There are several possible mechanisms of injury which could be causing pregnancy related LBP. During pregnancy, changes occur in the facet joints, in the back muscles, and in ligaments. This is mainly caused by the increased release of the hormone relaxin,[2] which causes ligament laxity, and therefore can affect the stability of the spine and lead to back pain.
During pregnancy, the enlarging gravid uterus changes the load and body mechanics. It’s shifts the centre of gravity forwards, increasing the stress on the lower back. Postural changes can be used to balance the anterior shift possibly causing an extra lordosis. This increases the natural inward curvature of the spine, which increases the mechanical strain on the lower back. It also puts an extra stress on the intervertebral disc, possibly causing a decreased height an overall compression of the spine. [8][7]
Another contributor is the increase in weight that comes with pregnancy. On average, about 11-15 kilograms are gained during pregnancy. The weight gain increases the amount of force placed across joints, changes the center of gravity, and forces the patient into an anterior pelvic tilt. The anterior displacement of the center of gravity will cause women to shift their heads and upper body posteriorly over the pelvis, causing hyperlordosis of the lumbar spine. This in turn, places additional stress on the intervertebral discs, ligaments, and facet joints and can lead to joint inflammation.[9] In addition, abdominal muscles are stretched and weakened, and the added weight can compress on the lumbosacral plexus.
The abdominal muscles also stretch to accommodate the expanding uterus. As they stretch, the muscles become tired and lose their ability to maintain normal body posture, causing the lower back to support the majority of the increased weight of the torso. [7]
Hormonal[edit | edit source]
A significant portion of women first experience pain during the first trimester of pregnancy. At that moment mechanical changes do not yet play a significant role in the onset of pain. This suggests that hormonal changes during pregnancy can cause inflammation and pain in the back. It has been suggested that the hormone relaxin increases 10-fold in concentration during pregnancy, softening the collagen and causes ligamentous laxity and discomfort. The sacroiliac ligaments, but also other ligaments who surround the pelvic girdle become loose. This causes a decrease in the stability and brings on a potential strain in the pelvic girdle and low back area. [8][7][6]
Circulatory[edit | edit source]
The expanding uterus can press on the vena cava, particularly at night when the patient is lying down. The pain is possibly severe enough to wake the patient up. This combined with the increased fluid volume from fluid retention during pregnancy leads to venous congestion and hypoxia in the pelvic and lumbar spine. [7]
Psychosocial Factors[edit | edit source]
Psychosocial factors can also increase low back pain. Pain-related catastrophizing, depression, pain intensity and time result in an increases in pain interference. The findings support the potential utility of the biopsychosocial model. Pain catastrophizing can be considered as a risk factor in the third trimester of pregnancy. [8]
Risk Factors[edit | edit source]
Several factors have been associated with the development of low back pain during pregnancy. More specifically, laborious work, a history of low back pain before pregnancy, and a previous history of pregnancy-related low back pain have been identified as risk factors for the development of pregnancy-related low back pain. Pain syndromes during pregnancy impact the abdominopelvic musculoskeletal system, thereby causing abnormal strain on the axial low back elements. [10]
| Risk factors | No risk factors |
|---|---|
| LBP history | Age |
| Multiple abortions | Fetal weight |
| Smoking | Oral contraceptives |
| Pain during previous pregnancy | |
| Number of pregnancies | Number of pregnancies |
| History of hypermobility | |
| Periods of amenorrhea | |
| Increased physical workload | |
| High body mass index | High body mass index |
| Lack of exercise/sedentary lifestyle | |
| Pain catastrophizing |
There is relative agreement in literature that excessive body weight may be a risk factor for LBP during pregnancy however, there are studies claiming that being overweight is not a risk. The same goes for number of pregnancies before the current one. [1][8][7]
Clinical Presentation [edit | edit source]
Onset[edit | edit source]
The most common onset tends to be during the fifth and sixth month of pregnancy, and the pain is usually worse in the evening. Often, the onset of pain occurs around the 18th week and reaches peak intensity between the 24th and 36th week of pregnancy. The pain can spontaneously disappear within 3 months, but 7-8% of the patients have a persisting, chronic pain. However it may start as early as the first trimester or be delayed as late s 3 weeks after delivery. [11] [12][13]
About 67% of women experience pain at night. Factors that aggravate the pain include: standing, sitting, coughing or sneezing, walking, and straining during a bowel movement.[9] However pain and a disability of the lumbopelvic region are usually proven to be experienced as mild to moderate, except for a minor part (20%) of the pregnant women that will describe the pain as severe.[14]
Area and Quality of Pain[edit | edit source]
The localization of pain is deep. It’s even possible that localization of the pain changes over time. Pelvic girdle pain has been described as “stabbing’’ , pain in the lower back as a “dull ache’’ and the pain in the thoracic spine is rather “burning’’. Other pain-descriptions are: shooting pain, feeling of oppression and a sharp twinge.
Pregnancy-related low back pain is characterized by a dull pain [15] and is more pronounced in forward flexion with associated restriction in spine movement and palpation of the erector spinae muscles exacerbates pain. [16]
Differential Diagnosis[edit | edit source]
Some other diagnoses that can be commonly mistaken for pregnancy related low back pain are: Sciatica, Meralgia Paresthetica, thoracic/rib pain, hip pain, coccygodynia, spontaneous abortions, osteomyelitis, osteoarthritis of spine or hip, Cauda Equina Syndrome, Osteitis Condensans Ilii, metastatic cancers, and Diastasis Rectus Abdominis. Other more common differential diagnoses are: disc disease, facet joint involvement and sacroiliac joint involvement. It is important to be able to recognize the subtle differences and differentiate between the comorbidities.[17][15]
- Disc Disease - Morning pain and stiffness, pain when weight bearing, pain with increased abdominal pressure, history of repeated micro trauma, pain when going uphill, pain with prolonged sitting, pain with sit to stand activity. Sleep is usually undisturbed, pain eases as day progresses and then gets worse again, movement eases pain but not for long (e.g. fidgets).”[17]
- Facet Joint Involvement - Non weight bearing pain, pain with related to movement (specifically rotation), pain increased by lateral compression, history of minor injury, pain is not usually referred to an extremity, pain eases with rest, not affected by coughing or sneezing”[17]
- Sacroiliac Involvement - Pain is usually unilateral and does not midline, can refer to lower extremities, turning while in supine provokes pain, getting out of the car provokes pain, pain is referred to the groin or genitals, pain is related to menstruation prior to pregnancy because of the effects of cyclic hormones on pre-pregnant SIJ ligaments.”[17]
It is also important to differentiate between pregnancy-related low back pain (PLBP) and pregnancy-related pelvic girdle pain (PPGP), as the management and prognosis of the two conditions may differ. Useful methods of differentiation include the site of pain, its character and severity, provoking factors, resultant disability, and the pain provocation tests. Recommended provocation tests are the posterior pelvic pain provocation test, Patrick’s Faber test, and the long dorsal sacroiliac ligament test. [18] In PPGP, the pain is typically concentrated under the posterior superior iliac spine, in the gluteal area, the posterior thigh, and the groin, meanwhile patients with PLBP show the pain to be concentrated in the lumbar region above the sacrum. [18]
Diagnostic Procedures[edit | edit source]
In order to formulate the correct diagnosis, the patient should be questioned about her past medical history. It is important to concentrate on experienced symptoms, limitations in activities, and movement possibilities. Questions about past pregnancies such as – "Have you experienced any complications with prior pregnancy/ies?" are appropriate. This will help the therapist understand the patient’s health problems and needs. Knowledge of the anatomical and functional disorders, activity limitations and restriction of participation will help the therapist determine her/his role and the need for appropriate interventions. It is important to recognize red flag complaints and contact a doctor to seek further investigation, if they are present.[5]
It is important at the time of initial assessment to differentiate between the lumbar spine and pelvic dysfunction. This can be done during the subjective by inquiring about aggravating factors. Activities such as turning in bed, getting out of a car, walking and climbing stairs may indicate that the origin of pain may be due to pelvic dysfunction. This can then be confirmed with a range of tests for assessing the sacroiliac joint and pubic symphysis.
Outcome Measures[edit | edit source]
Several validated instruments to assess back pain exist for general population who can be used in the diagnosis to estimate the complaints more objectively:
- Visual Analogue Scale (VAS)
- Roland Disability Questionnaire (RDQ)
- Québec Pain disability index (QPDI) [19]
- PHotograph series Of Daily Activities (PHODA)
- Impact on Participation and Autonomy (IPA)
- Pain Behavior Scale (PBS)
- Oswestry Disability Index. [6]
Due to a lack of pregnancy-specific outcome measures, a pregnancy-specific self-report questionnaire assessing mobility in relation to both back and pelvic pain, called the Pregnancy Mobility Index (PMI), was developed and validated. Van De Pol et al. developed the Pregnancy Mobility Index (PMI) to assess the ability of doing normal household activities. The patient can answer on a scale from ‘no problem’ to ‘impossible’ or ‘only with aid of others’. The PMI is used to evaluate the mobility and quality of life of pregnant women who suffer from LBP. [20]
Examination[edit | edit source]
During an examination of a pregnant patient, positioning is a key consideration. Excessive time in supine is not recommended due to the weight of the uterus on the vena cava and vital structures.[17] Based on the level of pain and disability of the patient, and potentially the size of the pregnant abdomen, certain tests and measures may need to be modified for this population.Excessive time in supine is not recommended due to the weight of the uterus on the vena cava and vital structures.[17]
Physical Exam[edit | edit source]
Examination should include observation of the posture and gait, neurologic screen to rule out underlying pathology, range of motion, muscle tests, palpation, muscle length tests, and assessment of joint mobility.
It’s important to distinguish posterior pelvic pain from low back pain during physical examination. Recommended provocation tests are the Posterior Pelvic Pain Provocation (PPPP) test, FABER test, long dorsal sacroiliac ligament test and standing on one leg. As mentioned above, the pain is typically concentrated under the posterior superior iliac spine, in the gluteal area, the posterior thigh and the groin in case of PPGP. Patients with PLBP show pain concentrated in the lumbar region above the sacrum. [23][18] Palpation over soft tissue of the sacroiliac, pubic symphysis, and gluteal regions can also distinguish pelvic pain from tenderness over the back above the waist. Studies show that both methods are effective although pain provocation tests are more reliable than palpation tests.
Modified Tests[edit | edit source]
Some tests cannot be performed as per usual given the patient's growing abdomen therefore the following modifications are needed.[24]
Hip Flexor Length: To modify the test position of the ‘Thomas Test’ the patient will have to sit on the edge of a table or mat, and extend the test leg as much as possible, while maintaining slight knee flexion. The pelvis should be kept in a neutral alignment. A patient with non-impaired flexibility should be able to extend her hip perpendicular to the floor.
SI Joint Examination: If the patient is unable to stand, instruct the patient to lie in supine and perform a pelvic bridge. The bridge will place the pelvis in neutral - the ASIS’ can be palpated for symmetry.
Figure B: Walk B. Texas State University's Evidence-based Practice project.
Medical Management[edit | edit source]
It is important to encourage the patient to receive regular checkups by her obstetrician. During the therapy session, continually check on pain levels and any aches radiating from the low back or stomach. Some patients tolerate pain and discomfort better than others and will therefore mask their distress – Use a chart for Rate of Perceived Exertion to determine the patient's true status and take note of any changes that occur between the begging and end of the session.
Although there are numerous interventions promoted for low back pain during pregnancy, the most common and widely used is a specific exercise program designed by a physical/physiotherapist (see below)[25] [26]. Another intervention that is getting tractions and shows prominent research is acupuncture. Recent studies show that a week of continuous acupuncture at specific auricular points can decrease pain and increase the capacity for some physical activity which can help diminish the need for drugs.[27]
Other Interventions[edit | edit source]
- Side lying while sleeping or resting using a wedge shaped pillow to support stomach
- Use of pillow between the legs while side lying (squeeze the pillow/legs together while rolling)
- Compression socks to promote venous return and decrease edema
- Support belt (The Love Comfort support belt is covered by Medicaid) [17]
- Soft tissue massage
- Acetaminophen as prescribed by physician
- Yoga
- Aquatherapy[28]
- Intra-articular sacroiliac joint injections (under imaging guidance) for ankylosing spondylitis can be recommended. There are indications that acupuncture during pregnancy may reduce pain, but high quality studies are required for sacroiliac joint therapeutic injection therapy. [18] [10]
- Most therapeutic strategies encourage preventive measures among pregnant women and those who are planning to become pregnant. It has been shown that women who participate in prophylactic education and strengthening programs during early pregnancy can avoid problems from low back pain.
Physical Therapy Management[edit | edit source]
Studies have found that pregnant women with low back pain, who participate in both education and physical therapy, have less pain and disability, higher quality of life, and improvement on physical tests. Physical therapy encompasses several factors such as postural modifications, back strengthening, stretching, and self-mobilization techniques. Functional stability can be maintained throughout pregnancy by strengthening the muscles around the lumbar spine through various back exercises. [10] [29]
Treatment depends on the diagnosis and timing of pregnancy (before or after childbirth). The patient should understand her own symptoms and be motivated to remain active.
Red Flags[edit | edit source]
The following are crucial to identify during treatments:[3]
- Vaginal bleeding
- Dizziness/feeling faint
- Shortness of breath
- Chest pain
- Headache
- Muscles weakness
- Calf pain or swelling
- Uterine contractions
- Decreased fetal movement
- Vaginal fluid leakage
- Neurological symptoms
Physical Therapy Goals[edit | edit source]
The focus of physiotherapy is to:
- Restore biomechanics during daily activities
- Improve lumbo-pelvic stabilization
- Educate and prevent[25]
Physical therapy should be focused on the following strategies[30]
1) Patient Instructions
It’s important to communicate with the patient and provide information about the relevant anatomy, ergonomics, back education (to prevent unnecessary mechanical stress on the back), and how to manage ADL activities (walking, standing, sitting, lying, and work position, learning how to control pain). Research shows that when the symptoms are explained, patients can feel more at ease and their anxiety may decrease.
- Using a small pillow between the legs while sitting and rolling in order to stabilize the back.
- Postural correction by standing upright with a neutral posture, avoiding hyperlordosis
- Do not sit or stand for a long time, alternate it with walking or stretching
- Taking breaks and resting in a comfortable position, with the back supported to relieve tired muscles
- Sleeping lying on one side with the top leg on a pillow
- “Use of a small footstool for one foot in sitting or standing, alternate feet”[30]
- Avoiding spine twisting while lifting
2) Active Back Exercises
Even though most pregnant patients will be advised to exercises within their safe and pain free range, studies show that less than 50% will actually do so. [31]. Furthermore it has also been proven that training the rectus abdominus muscles will be useless due to his weakness during the pregnancy.
Stability, coordination and functional preservation should be trained with active back exercises – endurance training for back muscles stabilization. Pelvic tilts, knee pull, straight leg raising, curl up, lateral straight leg raising and water aerobics are recommended because these exercises could relieves lumbar pain in pregnancy. Relaxation exercises while paying close attention to proper respiration also show to be beneficial.
Management includes specific interventions to address pain, weakness, and mobility in the low back region. The Ottawa Panel also recommends massage therapy in order to treat subacute and chronic low back pain.
3) Manual Therapy Techniques
| Posterior/Anterior mobilizations in side lying position | Addresses pain and mobility (Grades 1-4). |
Figure C: Walk B. Texas State University's Evidence-based Practice |
| Muscle Energy Technique by resisting hip flexion in side laying while stabilizing the sacrum | Corrects anterior innominate rotation. |
Figure D: Walk B. Texas State University's Evidence-based Practice |
| Spinal manipulation(Level of evidence:2A) | Are used to relax soft tissues |
| Strengthening Gluteus Mediu |
Position the patient in a side lying and place an elastic around both legs above the knees. Ask the patient to perform an external rotation of her leg in order to strengthen the Gluteus Medius. Perform this exercise on both sides. Feet need to be kept together during the whole exercise. Also, prevent the pelvis from externally rotating. |
Figure E: Walk B. Texas State University's Evidence-based Practice |
| Abdominal Drawing in Maneuver with Physioball (ADIM). |
Ask the patient to sit on a physioball and simulate a walk movement with the lower extremities. This will encourage the back muscle memory to stabilize back during ADL's.
|
Figure F: Walk B. Texas State University's Evidence-based Practice |
| Latissimus dorsi pull-downs |
The patient will be positioned on a physioball, which will force the pelvic, abdomen and back muscles to stay active in order to find a balanced sitting position. This part of the exercise will provoke a contraction of the glutei to increase the strength of the posterior oblique sling muscles which compress the SIJ. Keep the back straight during the whole exercise. |
Figure G: Walk B. Texas State University's Evidence-based Practice |
| Angry Cat (Level of evidence:5) | Starting from the hands-and knees-position the patient will move her back up and down. During this exercise it is important to keep the arms stretched out with the hands positioned right under the shoulders and to keep the stomach muscles tight throughout the entire exercise. |
Figure H: [32](Level of evidence:5) |
| Pelvic Tilt (Level of evidence:5) | Lay down with flexed knees and move the pelvic in an anterior and posterior position. |
Figure I: Women health clinic. Post Natal Exercises. Available at: http://www.pregnancyandchildcare. info/pregnancy_articles/ postnatalexer.html |
4) TENS
There is no strong evidence on the benefits of Tens on Low back pain in pregnancy but it can be used as a supplementary therapy. It’s important to use a low intensity and avoid the acupuncture points which may induce throes. Precautions and contra-indications must be respected.[15][33]
Patients should take caution when using ultrasound and electrical stimulation and avoid placing those modalities anywhere near the stomach or low back.
5) Yoga
Yoga can effectively decrease low back pain intensity. [34](Level of evidence:1B)
6) Stretching
1. Lower Back Stretch: it is plausible that stretching lower back and hip extensor muscles can lead to increased lower back and pelvic flexibility.
Figure J + K: [32]Stahmann Dilfer C.; Your Baby, Your Body (Fitness during pregnancy); Crown publishers, inc., New York, 1977'
Instructions:
- Clasp your fingers around your right knee.
- Gently pull your knee as close to your chest as possible. Relax your lower back and try to let your glutes (butt) roll of the floor as you pull.
- Hold for a slow count of 3.
- Release.
- Repeat steps 1-4, 12-15 times.
- Now, grasp your left knee, put the right foot flat on the floor and repeat steps 1-5
- Finally, grasp both knees with your hands, and pull both knees close to your chest (or outside your stomach)
- Repeat steps 2-5.
2. Combined squat stretch, back and hamstrings stretch: strengthens thighs (upper legs) and gluts, stretches hamstrings, inner thighs, pelvic floor muscles and back.[32](Level of evidence:5)
Figure L + M: [32](Level of evidence:5) Stahmann Dilfer C.; Your Baby, Your Body (Fitness during pregnancy); Crown publishers, inc., New York, 1977
Instructions:[32](Level of evidence:5)
- Squat down on your feet, feet pointing at a 45° angle to the sides, heels on the floor
- Open your knees wide using thigh muscles and push them apart until they are directly over your feet
- Keep your knees back over your feet, and slowly raise your gluts – keep on extending your knees – until your legs are as straight as possible (do not lock out your knees)
- Relax your head, neck and shoulders
- Hold position for 10 counts/seconds
- Try to keep your knees over your feet and slowly lower your gluts until you return to starting position.
7) Aerobic Exercises
Walking, swimming (Level of evidence: 1B),Tai chi, recumbent bicycle (or nu-step), are plausible to be beneficial at a low to moderate intensity. The stress on the back should be minimal.[35](Level of evidence:2A)
8) Home Exercises
The exercises explained above could also be performed at home if both the patient and therapist feel confident that the exercises will be performed correctly without supervision.
Back tuck arch [32]Lean with the back against the wall and alternate between anterior and posterior pelvic tilt.
Figure N: Hughston clinic. Excercising during pregnancy. Available at : http://www.hughston.com/a-11-3-4.aspx
Prognosis[edit | edit source]
Patients recover from LBP in pregnancy within a few weeks or a few months after childbirth, but symptoms may return during a future pregnancy. Between 8% and 10% of women will continue to experience pain for up to 2 years post-delivery.[15](Level of evidence:3A)
Key Research[edit | edit source]
Low back pain pregnancy/pregnant, LBP pregnancy, pregnancy back pain, maternal low back pain, gestation low back pain, pregnancy exercise(s), low back pain causes, low back pain physical therapy.
Resources[edit | edit source]
Clinical Bottom Line[edit | edit source]
The majority of pregnant women experience low back pain. Appropriate examination, interventions and follow up, can help in managing the pain. There are many physiotherapy treatments for pregnant woman with low back pain. Our research suggested a combination of instructions, manual therapy, active exercises, aerobic exercises and stretching. Key questions must be asked and special modifications must be made for more complex patient experiencing pregnancy related back pain. As patient centered practitioners, it is our job to research and implement evidence based practice to increase outcomes with minimal number of treatments.
We concluded there is a dearth in good quality research. Future studies should more concentrate on the specific low back pain of pregnant woman.
Presentations[edit | edit source]
 |
Pelvic Physiotherapy - to Kegel or Not?
This presentation was created by Carolyn Vandyken, a physiotherapist who specializes in the treatment of male and female pelvic dysfunction. She also provides education and mentorship to physiotherapists who are similarly interested in treating these dysfunctions. In the presentation, Carolyn reviews pelvic anatomy, the history of Kegel exercises and what the evidence tells us about when Kegels are and aren't appropriate for our patients. |
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Weis CA, Barrett J, Tavares P, Draper C, Ngo K, Leung J, Huynh T, Landsman V. Prevalence of low back pain, pelvic girdle pain, and combination pain in a pregnant Ontario population. Journal of Obstetrics and Gynaecology Canada. 2018 Aug 1;40(8):1038-43.
- ↑ 2.0 2.1 Robey JH, Boyle K. The role of prism glass and postural restoration in managing a collegiate baseball player with bilateral sacroiliac joint dysfunction: A case report. International Journal of Sports Physical Therapy. 2013 Oct;8(5):716.
- ↑ 3.0 3.1 Perkins J, Hammer RL, Loubert PV. Identification and management of pregnancy-related low back pain. Journal of nurse-midwifery. 1998 Sep 1;43(5):331-40.
- ↑ Ansari NN, Hasson S, Naghdi S, Keyhani S, Jalaie S. Low back pain during pregnancy in Iranian women: Prevalence and risk factors. Physiotherapy theory and practice. 2010 Jan 1;26(1):40-8.
- ↑ 5.0 5.1 Bekkering GE, Hendriks HJ, Koes BW, Oostendorp RA, Ostelo RW, Thomassen JM, Van Tulder MW. Dutch physiotherapy guidelines for low back pain. Physiotherapy. 2003 Feb 1;89(2):82-96.
- ↑ 6.0 6.1 6.2 6.3 Glinkowski WM, Tomasik P, Walesiak K, Głuszak M, Krawczak K, Michoński J, Czyżewska A, Żukowska A, Sitnik R, Wielgoś M. Posture and low back pain during pregnancy—3D study. Ginekologia Polska. 2016;87(8):575-80.[1]
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 Katonis P, Kampouroglou A, Aggelopoulos A, Kakavelakis K, Lykoudis S, Makrigiannakis A, Alpantaki K. Pregnancy-related low back pain. Hippokratia. 2011 Jul;15(3):205.
- ↑ 8.0 8.1 8.2 8.3 8.4 Chang HY, Lai YH, Jensen MP, Shun SC, Hsiao FH, Lee CN, Yang YL. Factors associated with low back pain changes during the third trimester of pregnancy. Journal of advanced nursing. 2014 May;70(5):1054-64.
- ↑ 9.0 9.1 To WW, Wong MW. Factors associated with back pain symptoms in pregnancy and the persistence of pain 2 years after pregnancy. Acta obstetricia et gynecologica Scandinavica. 2003 Jan 1;82(12):1086-91.
- ↑ 10.0 10.1 10.2 10.3 Shah S, Banh ET, Koury K, Bhatia G, Nandi R, Gulur P. Pain management in pregnancy: multimodal approaches. Pain research and treatment. 2015;2015.
- ↑ Verstraete EH, Vanderstraeten G, Parewijck W. Pelvic Girdle Pain during or after Pregnancy: a review of recent evidence and a clinical care path proposal. Facts, views & vision in ObGyn. 2013;5(1):33.
- ↑ Wu WH, Meijer OG, Uegaki K, Mens JM, Van Dieen JH, Wuisman PI, Östgaard HC. https://link.springer.com/article/10.1007/s00586-003-0615-y. European Spine Journal. 2004 Nov;13:575-89.
- ↑ Gutke A, Östgaard HC, Öberg B. Pelvic girdle pain and lumbar pain in pregnancy: a cohort study of the consequences in terms of health and functioning. Spine. 2006 Mar 1;31(5):E149-55.
- ↑ Mens JM, Huis YH, Pool-Goudzwaard A. Severity of signs and symptoms in lumbopelvic pain during pregnancy. Manual therapy. 2012 Apr 1;17(2):175-9.
- ↑ 15.0 15.1 15.2 15.3 Vermani E, Mittal R, Weeks A. Pelvic girdle pain and low back pain in pregnancy: a review. Pain Practice. 2010 Jan;10(1):60-71.
- ↑ Östgaard HC, Roos-Hansson E, Zetherström G. Regression of back and posterior pelvic pain after pregnancy. Spine. 1996 Dec 1;21(23):2777-80.
- ↑ 17.0 17.1 17.2 17.3 17.4 17.5 17.6 Östgaard HC, Roos-Hansson E, Zetherström G. Regression of back and posterior pelvic pain after pregnancy. Spine. 1996 Dec 1;21(23):2777-80.
- ↑ 18.0 18.1 18.2 18.3 Vleeming A, Albert H, Ostgaard HC, Stuge B, Sturesson B. European guidelines on the diagnosis and treatment of pelvic girdle pain [European Commission Research Directorate General Web site]. 2005. Available online at: www. backpain europe. org, accessed April. 2008.
- ↑ Mens JM, Vleeming A, Snijders CJ, Ronchetti I, Ginai AZ, Stam HJ. Responsiveness of outcome measurements in rehabilitation of patients with posterior pelvic pain since pregnancy. Spine. 2002 May 15;27(10):1110-5.
- ↑ Van De Pol, G., et al. The Pregnancy Mobility Index: a mobility scale during and after pregnancy. Acta obstetricia et gynecologica Scandinavica 85.7 (2006): 786-791. (Evidence level: 2B)
- ↑ de Groot M, Pool-Goudzwaard AL, Spoor CW, Snijders CJ. The active straight leg raising test (ASLR) in pregnant women: differences in muscle activity and force between patients and healthy subjects. Manual Therapy. 2008 Feb 1;13(1):68-74.
- ↑ 22.0 22.1 Roussel NA, Nijs J, Truijen S, Smeuninx L, Stassijns G. Low back pain: clinimetric properties of the Trendelenburg test, active straight leg raise test, and breathing pattern during active straight leg raising. Journal of manipulative and physiological therapeutics. 2007 May 1;30(4):270-8.
- ↑ Mens JM, Huis YH, Pool-Goudzwaard A. The Active Straight Leg Raise test in lumbopelvic pain during pregnancy. Manual therapy. 2012 Aug 1;17(4):364-8.
- ↑ Cullaty M. Suspected sacroiliac joint dysfunction: modifying examination and intervention during pregnancy. Journal of Women’s Health Physical Therapy. 2006 Jul 1;30(2):18-24.
- ↑ 25.0 25.1 Stuge B, Hilde G, Vøllestad N. Physical therapy for pregnancy-related low back and pelvic pain: a systematic review. Acta obstetricia et gynecologica Scandinavica. 2003 Jan 1;82(11):983-90.
- ↑ Mens JM, Snijders CJ, Stam HJ. Diagonal trunk muscle exercises in peripartum pelvic pain: a randomized clinical trial. Physical therapy. 2000 Dec 1;80(12):1164-73.
- ↑ Wang SM, DeZinno P, Lin EC, Lin H, Yue JJ, Berman MR, Braveman F, Kain ZN. Auricular acupuncture as a treatment for pregnant women who have low back and posterior pelvic pain: a pilot study. American journal of obstetrics and gynecology. 2009 Sep 1;201(3):271-e1.
- ↑ Granath AB, Hellgren MS, Gunnarsson RK, Water aerobics reduces sick leave due to low back pain during pregnancy. J Obstet Gynecol Neonatal Nurs. 2006 Jul-Aug;35(4):465-71 (Evidence level: 1B)
- ↑ 29.0 29.1 Borg-Stein J, Dugan SA. Musculoskeletal disorders of pregnancy, delivery and postpartum. Physical medicine and rehabilitation clinics of North America. 2007 Aug 1;18(3):459-76.
- ↑ 30.0 30.1 Beales DJ, O'Sullivan PB, Briffa NK. The effects of manual pelvic compression on trunk motor control during an active straight leg raise in chronic pelvic girdle pain subjects. Manual therapy. 2010 Apr 1;15(2):190-9.
- ↑ George JW, Skaggs CD, Thompson PA, Nelson DM, Gavard JA, Gross GA. A randomized controlled trial comparing a multimodal intervention and standard obstetrics care for low back and pelvic pain in pregnancy. American journal of obstetrics and gynecology. 2013 Apr 1;208(4):295-e1.
- ↑ 32.0 32.1 32.2 32.3 32.4 32.5 Stahmann Dilfer C. Your Baby, Your Body (Fitness during pregnancy) New York: Crown publishers, inc. 1977 (Evidence level: 5)
- ↑ Khadilkar A, Odebiyi DO, Brosseau L, Wells GA. Transcutaneous electrical nerve stimulation (TENS) versus placebo for chronic low‐back pain. Cochrane Database of Systematic Reviews. 2008(4).
- ↑ Martins, Roseny Flávia, and João Luiz Pinto e Silva. Treatment of pregnancy-related lumbar and pelvic girdle pain by the yoga method: a randomized controlled study. The Journal of Alternative and Complementary Medicine 20.1 (2014): 24-31. (Evidence level: 1B)
- ↑ Field T., Prenatal exercise research, Infant Behavior & Development 35 (2012) 397– 407 (Evidence level: 2A)