Foot and Ankle Assessment-Investigations and Tests: Difference between revisions
No edit summary |
No edit summary |
||
| (46 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor''' - [[User: | '''Original Editor''' - [[User:Ewa Jaraczewska|Ewa Jaraczewska]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
Taking a patient's history and completing an objective assessment is | Taking a patient's history and completing an objective assessment is the gold standard for the foot and ankle assessment. The purpose of using special investigations and tests is to confirm the clinical diagnosis. <blockquote>"We can't treat the patient just on x-rays or just on MRI findings. These things have to come together (with the objective assessment)". ''Helene Simpson'' </blockquote> | ||
== Investigations == | |||
=== | === X-Rays === | ||
An X-ray can help to investigate bone | [[File:Lisfranc.jpg|thumb|Lisfranc joint complex]] | ||
* Assists with the diagnosis of the '''Achilles tendon rupture''' based on the presence of five radiological X-ray signs<ref name=":0">Bowen L, Evans R, Bodger O, Howard J, Anne-Marie H. [https://pdfs.semanticscholar.org/ebf8/385215a158a6c5a2ea5b63554eba5dfa2d42.pdf Investigating the Validity of Soft Tissue Signs on Lateral Ankle X-Ray to Aid Diagnosis of Achilles Tendon Rupture in the Emergency Department]. Int J Foot Ankle. 2019;3:033.</ref> | [[File:Sesamoid Bone.png|thumb|Sesamoid Bone in the distal end of the first metatarsal ]] | ||
* May not be sufficient to identify '''malleolar fractures.''' <ref name=":1">Szymański T, Zdanowicz U. [https://reader.elsevier.com/reader/sd/pii/S1268773121000783?token=20BAABA2656F575E4601ED8303F1B6E4B0582F1FC9F97CE00713DCEF03C1EECA7C36EA352B30679E107BB48D397AC0AB&originRegion=eu-west-1&originCreation=20220108195539 Comparison of routine computed tomography and plain X-ray imaging for malleolar fractures—How much do we miss]?. Foot and Ankle Surgery. 2021 Apr 1.</ref> | An [[X-Rays|X-ray]] can help to investigate bone and soft tissue: | ||
* '''Syndesmosis injury''' is often overlooked on X- | * Assists with the diagnosis of the '''[[Achilles Rupture|Achilles tendon rupture]]''' based on the presence of five radiological X-ray signs.<ref name=":0">Bowen L, Evans R, Bodger O, Howard J, Anne-Marie H. [https://pdfs.semanticscholar.org/ebf8/385215a158a6c5a2ea5b63554eba5dfa2d42.pdf Investigating the Validity of Soft Tissue Signs on Lateral Ankle X-Ray to Aid Diagnosis of Achilles Tendon Rupture in the Emergency Department]. Int J Foot Ankle. 2019;3:033.</ref> A lateral ankle X-ray is reliable to support the diagnosis of the Achilles tendon rupture.<ref name=":0" /> | ||
* Assists with a diagnosis of | * May not be sufficient to identify '''malleolar fractures.'''<ref name=":1">Szymański T, Zdanowicz U. [https://reader.elsevier.com/reader/sd/pii/S1268773121000783?token=20BAABA2656F575E4601ED8303F1B6E4B0582F1FC9F97CE00713DCEF03C1EECA7C36EA352B30679E107BB48D397AC0AB&originRegion=eu-west-1&originCreation=20220108195539 Comparison of routine computed tomography and plain X-ray imaging for malleolar fractures—How much do we miss]?. Foot and Ankle Surgery. 2021 Apr 1.</ref> | ||
* Malalignment of the second tarsometatarsal joint is a common feature in | * '''[[Syndesmotic Ankle Sprains|Syndesmosis injury]]''' is often overlooked on X-rays.<ref name=":1" /> | ||
* '''Hindfoot malalignment''' causes foot and ankle disability | * Assists with a diagnosis of an '''[[Diagnostic Imaging of the Foot and Ankle for Physical Therapists|ankle fracture]]'''. AP, lateral and mortise views are recommended. Mortise view refers to the AP view with 15° internal rotation. If possible, the X-ray should be done with the patient in a standing position. The patient is advised to stand even with little weight (even 99 % on the un-injured foot). There are exceptions when there is an obvious dislocation / open fracture. When ankle fracture is ruled out, but there is no progress in patient's rehabilitation and the patient continues to complain of pain, an X-ray should be repeated within 6 weeks to rule out [[Ankle Osteochondral Lesions|osteochondral lesion]] or hairline fracture. | ||
* The '''fracture of the sesamoid bone''' is shown on | * Malalignment of the second tarsometatarsal joint is a common feature in '''[[Lisfranc Injuries|Lisfranc fracture-dislocations]].''' The X-ray's AP view shows lateral displacement of the second metatarsal base and diastasis over 2 mm between the first and second metatarsal bases. It is recommended that an X-ray is taken of each foot in a weight-bearing position, so that the injured side can be compared to the contralateral side.<ref>Stavlas P, Roberts CS, Xypnitos FN, Giannoudis PV. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2989076/pdf/264_2010_Article_1101.pdf The role of reduction and internal fixation of Lisfranc fracture-dislocations: a systematic review of the literature]. Int Orthop. 2010 Dec;34(8):1083-91. </ref> | ||
* | * '''Hindfoot malalignment''' causes foot and ankle disability. The assessment of X-ray results of hindfoot alignment is important. The recommendation for a clinical and research purpose is to use the long axial hindfoot view in a bilateral stance. <ref>ML Reilingh, L Beimers, GJM Tuijthof, SAS Stufkens, M Maas, et al. [https://www.researchgate.net/publication/40900666_Measuring_hindfoot_alignment_radiographically_The_long_axial_view_is_more_reliable_than_the_hindfoot_alignment_view Measuring hindfoot alignment radiographically: the long axial view is more reliable than the hindfoot alignment view.] Skeletal radiology 2010;39 (11): 1103-1108.</ref> | ||
* The '''fracture of the [[Sesamoid|sesamoid bone]]''' is shown on X-ray as a rough space between the bone pieces. A smooth separation of two bones visible on X-ray is a normal sign in about 10 % of the population. | |||
* '''[[Ligament Sprain|Ligament injuries]]''' were confirmed on a first diagnostic X-ray in only 50% of patients. This number increased to 66% of patients during the second X-ray when the diagnosis was confirmed.<ref name=":3">Qi H, Feng Y. [https://ieeexplore.ieee.org/stamp/stamp.jsp?tp=&arnumber=9050426 Analysis of the clinical value of weight-bearing magnetic resonance diagnosis of ankle ligament sports injury.] IEEE Access. 2020 Mar 30;8:62725-37.</ref> | |||
=== | === Diagnostic Ultrasound === | ||
Diagnostic ultrasound allows for dynamic examination of | [[File:Mortons-neuroma-1.gif|thumb|Mortons neuroma US between 3rd & 4th MT heads ]] | ||
Diagnostic [[Ultrasound Scans|ultrasound]] allows for dynamic examination of foot and ankle pathology. It is a non-invasive, economical and readily available tool that is recommended as a first-line diagnostic modality to rule out torn [[Ligament|ligaments]], [[Tendon Pathophysiology|tendonitis]], tenosynovitis, [[Plantar Fasciitis|plantar fascia]], soft tissue masses or [[Morton's Neuroma|Morton's neuroma]]. <ref>Khoury V, Guillin R, Dhanju J, Cardinal É. Ultrasound of ankle and foot: overuse and sports injuries. Seminars in musculoskeletal radiology 2007 Jun; 11(02): 149-161.</ref> <ref>Rawool NM, Nazarian LN. Ultrasound of the ankle and foot. In: Seminars in Ultrasound, CT and MRI 2000 Jun; 21(3): 275-284. </ref> | |||
Diagnostic ultrasound was found to be an effective diagnostic tool for the | Diagnostic ultrasound was found to be an effective diagnostic tool for the following foot and ankle injuries: | ||
* '''Fifth metatarsal, lateral and medial malleolus fractures''' in patients with foot and/or ankle sprains. Note: sensitivity for navicular fractures is low.<ref>Atilla OD, Yesilaras M, Kilic TY, Tur FC, Reisoglu A, Sever M, Aksay E. [https://onlinelibrary.wiley.com/doi/epdf/10.1111/acem.12467 The accuracy of bedside ultrasonography as a diagnostic tool for fractures in the ankle and foot.] Academic Emergency Medicine. 2014 Sep;21(9):1058-61.</ref> | * '''Fifth [[Metatarsal Fractures|metatarsal]], lateral and medial malleolus fractures''' in patients with foot and/or ankle sprains. Note: sensitivity for [[navicular]] fractures is low.<ref>Atilla OD, Yesilaras M, Kilic TY, Tur FC, Reisoglu A, Sever M, Aksay E. [https://onlinelibrary.wiley.com/doi/epdf/10.1111/acem.12467 The accuracy of bedside ultrasonography as a diagnostic tool for fractures in the ankle and foot.] Academic Emergency Medicine. 2014 Sep;21(9):1058-61.</ref> | ||
* To rule out '''torn vs sprained anterior talofibular ligament and calcaneofibular ligament'''.<ref>Hosseinian SH, Aminzadeh B, Rezaeian A, Jarahi L, Naeini AK, Jangjui P. Diagnostic Value of Ultrasound in Ankle Sprain. The Journal of Foot and Ankle Surgery. 2021 Aug 20.</ref><ref>Esmailian M, Ataie M, Ahmadi O, Rastegar S, Adibi A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8106407/pdf/JRMS-26-14.pdf Sensitivity and specificity of ultrasound in the diagnosis of a traumatic ankle injury.] Journal of Research in Medical Sciences: The Official Journal of Isfahan University of Medical Sciences. 2021;26.</ref><ref>Gribble PA. [https://meridian.allenpress.com/jat/article/54/6/617/420891/Evaluating-and-Differentiating-Ankle-Instability Evaluating and differentiating ankle instability]. Journal of athletic training. 2019 Jun;54(6):617-27.</ref> | * To rule out '''torn vs sprained anterior talofibular ligament and calcaneofibular ligament'''.<ref>Hosseinian SH, Aminzadeh B, Rezaeian A, Jarahi L, Naeini AK, Jangjui P. Diagnostic Value of Ultrasound in Ankle Sprain. The Journal of Foot and Ankle Surgery. 2021 Aug 20.</ref><ref>Esmailian M, Ataie M, Ahmadi O, Rastegar S, Adibi A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8106407/pdf/JRMS-26-14.pdf Sensitivity and specificity of ultrasound in the diagnosis of a traumatic ankle injury.] Journal of Research in Medical Sciences: The Official Journal of Isfahan University of Medical Sciences. 2021;26.</ref><ref>Gribble PA. [https://meridian.allenpress.com/jat/article/54/6/617/420891/Evaluating-and-Differentiating-Ankle-Instability Evaluating and differentiating ankle instability]. Journal of athletic training. 2019 Jun;54(6):617-27.</ref> | ||
* Ankle pain related to lateral ligament pathologies, '''tendinous pathologies, and joint effusion'''. Note: limited use in a suspected posterior talofibular ligament injury.<ref>Singh K, Thukral CL, Gupta K, Singh A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6444321/pdf/jou-18-316.pdf Comparison of high-resolution ultrasonography with clinical findings in patients with ankle pain]. J Ultrason. 2018;18:316–24.</ref> | * Ankle pain related to lateral ligament pathologies, '''tendinous pathologies, and joint effusion'''. Note: limited use in a suspected posterior talofibular ligament injury.<ref>Singh K, Thukral CL, Gupta K, Singh A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6444321/pdf/jou-18-316.pdf Comparison of high-resolution ultrasonography with clinical findings in patients with ankle pain]. J Ultrason. 2018;18:316–24.</ref> | ||
* '''Achilles tendon injuries'''.<ref>Lee SH, Yun SJ. The feasibility of point-of-care ankle ultrasound examination in patients with a recurrent ankle sprain and chronic ankle instability: Comparison with magnetic resonance imaging. Injury. 2017;48:2323–8.</ref> | * '''Achilles tendon injuries'''.<ref>Lee SH, Yun SJ. The feasibility of point-of-care ankle ultrasound examination in patients with a recurrent ankle sprain and chronic ankle instability: Comparison with magnetic resonance imaging. Injury. 2017;48:2323–8.</ref> | ||
* Statistically significant for diagnosing a ''' syndesmosis injury''' at ≥6.0 mm of tibiofibular clear space widening. <ref>Fisher CL, Rabbani T, Johnson K, Reeves R, Wood A. [https://link.springer.com/content/pdf/10.1186/s12891-019-2899-z.pdf Diagnostic capability of dynamic ultrasound evaluation of supination-external rotation ankle injuries: a cadaveric study]. BMC musculoskeletal disorders. 2019 Dec;20(1):1-7.</ref> | * Statistically significant for diagnosing a''' syndesmosis injury''' at ≥6.0 mm of tibiofibular clear space widening.<ref>Fisher CL, Rabbani T, Johnson K, Reeves R, Wood A. [https://link.springer.com/content/pdf/10.1186/s12891-019-2899-z.pdf Diagnostic capability of dynamic ultrasound evaluation of supination-external rotation ankle injuries: a cadaveric study]. BMC musculoskeletal disorders. 2019 Dec;20(1):1-7.</ref> | ||
* | * Should be considered as a primary modality for '''foot and ankle fractures'''. <ref>Wu J, Wang Y, Wang Z. [https://medultrason.ro/medultrason/index.php/medultrason/article/view/2659/1656 The diagnostic accuracy of ultrasound in the detection of foot and ankle fractures: a systematic review and meta-analysis.] Medical Ultrasonography. 2021 May 20;23(2):203-12.</ref> | ||
=== | === MRI === | ||
MRI is the investigation of choice in chronic foot pain. Based on the available research MRI is a modality used in various foot and ankle soft tissue disorders due to its high resolution and contrast, but the interpretation of the results is key in proper diagnosis. MRI is: | [[File:MRI Ankle Sprain.jpg|thumb|254x254px|MRI Ankle Sprain]] | ||
[[MRI Scans|MRI]] is the investigation of choice in chronic foot pain. Based on the available research MRI is a modality used in various foot and ankle soft tissue disorders due to its high resolution and contrast, but the interpretation of the results is key in proper diagnosis. MRI modality is expensive and not always easily accessible in many countries and it should be the orthopaedic surgeon who requests this particular investigation. <blockquote>"It's fantastic to have a look at your soft tissue. If we're looking for [[cartilage]] injuries, it's sensitive, but it might overestimate the extent of the injury". ''Helene Simpson''</blockquote>MRI is: | |||
* A gold standard for the diagnosis of '''Achilles tendon rupture.'''<ref name=":0" /> | * A gold standard for the diagnosis of '''Achilles tendon rupture.'''<ref name=":0" /> | ||
* Recommended in patients with ongoing pain at rest following ankle sprains as the clinical examination is insufficient when '''syndesmotic injury''' is suspected.<ref>Grossterlinden LG, Hartel M, Yamamura J, Schoennagel B, Burger N, Krause M, et al. Isolated syndesmotic injuries in acute ankle sprains: diagnostic significance of clinical examination and MRI. Knee Surg Sports Traumatol Arthrosc. 2016;24(4):1180–6.</ref> | * Recommended in patients with ongoing pain at rest following ankle sprains as the clinical examination is insufficient when a ''' syndesmotic injury''' is suspected.<ref>Grossterlinden LG, Hartel M, Yamamura J, Schoennagel B, Burger N, Krause M, et al. Isolated syndesmotic injuries in acute ankle sprains: diagnostic significance of clinical examination and MRI. Knee Surg Sports Traumatol Arthrosc. 2016;24(4):1180–6.</ref> | ||
* A preoperative decisional tool for ''' | * A preoperative decisional tool for the '''anterior talofibular ligament repair''' in case of '''chronic lateral ankle instability'''.<ref>Morvan A, Klouche S, Thes A, Hardy P, Bauer T. Reliability and validity of preoperative MRI for surgical decision making in chronic lateral ankle instability. European Journal of Orthopaedic Surgery & Traumatology. 2018 May;28(4):713-9.</ref><ref>Cao S, Wang C, Ma X, Wang X, Huang J, Zhang C, Wang K. [https://josr-online.biomedcentral.com/track/pdf/10.1186/s13018-019-1102-4.pdf Reliability and validity of different ankle MRI scanning planes for the anterior talofibular ligament injury diagnosis: a cadaveric study]. Journal of orthopaedic surgery and research. 2019 Dec;14(1):1-8.</ref> | ||
* A routine inspection method of the ankle ligament in the case of the '''ankle ligament injury'''. A weight-bearing MRI is recommended because the transverse position and the coronal position can show the full length of the ligament.<ref name=":3" /> | * A routine inspection method of the ankle ligament in the case of the '''ankle ligament injury'''. A weight-bearing MRI is recommended because the transverse position and the coronal position can show the full length of the ligament.<ref name=":3" /> | ||
* A valuable tool in the diagnosis of | * A valuable tool in the diagnosis of '''post-traumatic ankle pain''' as it has 96% accuracy in detecting tendon injury.<ref name=":2">Elgohary MM, Abdul Rahim SA, Ibrahim TA. [https://journals.ekb.eg/article_11782_9027f455004fbdf2c244f7188ed35c66.pdf Role of MRI in Evaluation of Traumatic Ankle Injuries]. The Egyptian Journal of Hospital Medicine. 2017 Oct 1;69(3):2016-24.</ref> | ||
* Advantageous for assessing tendons, ligaments, nerves, and fascia and for recognising '''occult bone injuries'''. <ref name=":2" /> | * Advantageous for assessing tendons, ligaments, nerves, and fascia and for recognising '''occult bone injuries'''.<ref name=":2" /> | ||
* An investigation of choice for '''metatarsalgia''' due to its high resolution demonstrating sesamoid anatomy, plantar glenosesamoid apparatus, and the adjoining flexor, abductor, and adductor tendons. <ref>Batta NS, Gupta A, Batra V. [https://mss-ijmsr.com/imaging-findings-of-bilateral-medial-hallucal-sesamoid-insufficiency-in-a-marathon-runner/ Imaging Findings of Bilateral Medial Hallucal Sesamoid Insufficiency in a Marathon Runner]. Indian J Musculoskelet Radiol 2019;1(1):57-60.</ref> | * An investigation of choice for '''[[metatarsalgia]]''' due to its high resolution demonstrating sesamoid anatomy, plantar glenosesamoid apparatus, and the adjoining flexor, abductor, and adductor tendons.<ref>Batta NS, Gupta A, Batra V. [https://mss-ijmsr.com/imaging-findings-of-bilateral-medial-hallucal-sesamoid-insufficiency-in-a-marathon-runner/ Imaging Findings of Bilateral Medial Hallucal Sesamoid Insufficiency in a Marathon Runner]. Indian J Musculoskelet Radiol 2019;1(1):57-60.</ref> | ||
=== | === CT Scan === | ||
In the foot and ankle injury, the use of CT scan is a | [[File:Triplane fracture CT.png|thumb|233x233px|Triplane fracture CT]] | ||
In the foot and ankle injury, the use of [[CT Scans|CT scan]] is proposed as a modality to assess the passive subsystem. It is a quick tool and it can be used during surgery. A weight-bearing computed tomography (WBCT) allows for the measurement and analysis of foot and ankle bone position and its deformities.<ref>Rojas EO, Barbachan Mansur NS, Dibbern K, Lalevee M, Auch E, Schmidt E, Vivtcharenko V, Li S, Phisitkul P, Femino J, de Cesar Netto C. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8259196/ Weightbearing Computed Tomography for Assessment of Foot and Ankle Deformities: The Iowa Experience.] Iowa Orthop J. 2021;41(1):111-119. </ref> The recommendations for using a CT scan and WBCT are: | |||
* To assess '''fractures in the ankle''' joint area. <ref name=":1" /> | * To assess '''fractures in the ankle''' joint area.<ref name=":1" /> | ||
* To evaluate a '''syndesmotic reduction'''. A weight-bearing CT (WBCT) scan is proven to be more reliable.<ref>Abdelaziz ME, Hagemeijer N, Guss D, El-Hawary A, El-Mowafi H, DiGiovanni CW. Evaluation of syndesmosis reduction on CT scan. Foot & ankle international. 2019 Sep;40(9):1087-93.</ref> | * To evaluate a '''syndesmotic reduction'''. A weight-bearing CT (WBCT) scan is proven to be more reliable.<ref>Abdelaziz ME, Hagemeijer N, Guss D, El-Hawary A, El-Mowafi H, DiGiovanni CW. Evaluation of syndesmosis reduction on CT scan. Foot & ankle international. 2019 Sep;40(9):1087-93.</ref> | ||
* To predict '''syndesmotic injuries''' in ankle fractures.<ref>Lee SW, Lee KJ, Park CH, Kwon HJ, Kim BS. [https://www.mdpi.com/2075-4418/10/10/812/htm The Valid Diagnostic Parameters in Bilateral CT Scan to Predict Unstable Syndesmotic Injury with Ankle Fracture]. Diagnostics. 2020 Oct;10(10):812.</ref> | * To predict '''syndesmotic injuries''' in ankle fractures.<ref>Lee SW, Lee KJ, Park CH, Kwon HJ, Kim BS. [https://www.mdpi.com/2075-4418/10/10/812/htm The Valid Diagnostic Parameters in Bilateral CT Scan to Predict Unstable Syndesmotic Injury with Ankle Fracture]. Diagnostics. 2020 Oct;10(10):812.</ref> | ||
* To characterise '''hindfoot alignment''' in order to determine the amount of translation needed for a neutral alignment during a calcaneal osteotomy.<ref>Burssens A, Peeters J, Buedts K, Victor J, Vandeputte G. Measuring hindfoot alignment in weight-bearing CT: A novel clinical relevant measurement method. Foot Ankle Surg. 2016 Dec;22(4):233-238.</ref> | * To characterise '''hindfoot alignment''' in order to determine the amount of translation needed for a neutral alignment during a calcaneal osteotomy.<ref>Burssens A, Peeters J, Buedts K, Victor J, Vandeputte G. Measuring hindfoot alignment in weight-bearing CT: A novel clinical relevant measurement method. Foot Ankle Surg. 2016 Dec;22(4):233-238.</ref> | ||
* To diagnose subtle '''Lisfranc instability'''.<ref>Bhimani R, Sornsakrin P, Ashkani‐Esfahani S, Lubberts B, Guss D, De Cesar Netto C, Waryasz GR, Kerkhoffs GM, DiGiovanni CW. Using area and volume measurement via weight-bearing CT to detect Lisfranc instability. Journal of Orthopaedic Research®. 2021 Jan 6.</ref> | * To diagnose subtle '''Lisfranc instability'''.<ref>Bhimani R, Sornsakrin P, Ashkani‐Esfahani S, Lubberts B, Guss D, De Cesar Netto C, Waryasz GR, Kerkhoffs GM, DiGiovanni CW. Using area and volume measurement via weight-bearing CT to detect Lisfranc instability. Journal of Orthopaedic Research®. 2021 Jan 6.</ref> | ||
== Special Tests == | |||
=== | === Ottawa Foot and Ankle Rules === | ||
Ottawa Ankle Rule is | Ottawa Ankle Rule determine the need for radiographs in acute ankle sprains. It is an accurate instrument for excluding fractures of the ankle and mid-foot, but the test has some limitations: | ||
* High accuracy is true for the first 10 days post-injury | * High accuracy is true for the first 10 days post-injury | ||
* High sensitivity is detected for patients younger than 55- years- old | * High sensitivity is detected for patients younger than 55- years- old | ||
Detailed information can be found on [[Ottawa Ankle Rules|Ottawa Ankle Rule]] page. | Detailed information can be found on the [[Ottawa Ankle Rules|Ottawa Ankle Rule]] page. | ||
=== Knee To Wall Test === | |||
=== | [[File: Helene Simpson Knee-to-Wall Test.jpg|thumb|Knee-To-Wall Test]]Should always be performed when assessing ankle and foot injury: | ||
* Provides a means of assessing dorsiflexion range of motion at the ankle joint | |||
* Recommended when conditions such as foot overpronation or plantar fasciitis are being examined | |||
* Starting position for testing: toes against the wall and gradually moving away. The distance between the toes and the wall is measured with the ruler and is recorded for comparison and future reassessment. | |||
{{#ev:youtube|v=wV9tITMsbDs|300}}<ref>The Weight Bearing Lunge Test. 2017. Available from: https://www.youtube.com/watch?v=wV9tITMsbDs [last accessed 12/01/2022]</ref> | |||
Detailed information can be found on the [[Knee to Wall Test|Knee To Wall Test]] page. | |||
=== | === Anterior Drawer Test === | ||
* Always performed in ankle and foot injury | * Always performed in when assessing an ankle and foot injury | ||
* Always compare with normal side | * Always compare with the "normal" side | ||
* During the test remember to "hug" the calcaneus, because it moves the talus | * During the test remember to "hug" the calcaneus, because it moves the talus. | ||
* See more here [[Anterior Drawer of the Ankle]] | |||
=== Squeeze Test === | |||
=== | |||
* Performed to detect syndesmotic injury | * Performed to detect syndesmotic injury | ||
* Attempting to reproduce pain symptoms | * Attempting to reproduce pain symptoms | ||
Detailed information can be found on [[Squeeze Test]] page. | Detailed information can be found on the [[Squeeze Test]] page. | ||
=== | === External Rotation Test === | ||
* Performed to detect syndesmotic injury | * Performed to detect a syndesmotic injury | ||
* Attempting to reproduce a mechanism of the injury | * Attempting to reproduce a mechanism of the injury | ||
{{#ev:youtube|v= | {{#ev:youtube|v=LnB1fta_rQA|300}}<ref>Kleiger's Test or External Rotation Test. 2013 Available from: https://www.youtube.com/watch?v=LnB1fta_rQA [last accessed 12/01/2022]</ref> | ||
Detailed information can be found on the [[Kleiger's Test|External Rotation Test]] page. | |||
=== Cotton Test === | |||
* Performed to detect syndesmotic instability | |||
* It is a manual stress test | |||
* It identifies the amount of the lateral translation of the talus within the ankle mortise | |||
{{#ev:youtube|v=qX68KET3dls|300}}<ref> UWECATEP. Cotton Test. 2013. Available from: https://www.youtube.com/watch?v=qX68KET3dls [last accessed 12/01/2022]</ref> | |||
=== Coleman Block Test === | |||
* Performed to evaluate hindfoot flexibility and pronation of forefoot | |||
* Completed by supporting the lateral forefoot on a woodblock that is 2.5-4 cm thick | |||
* Determines if an inverted heel is due to a forefoot issue | |||
{{#ev:youtube|v=TCp25F0l7hc |300}}<ref>Assessing Foot Flexibility: Part 05 (Modified Coleman Block Test). Available from: https://www.youtube.com/watch?v=TCp25F0l7hc [last accessed 6/6/2009]</ref> | |||
=== | === Other Tests === | ||
Other special tests include: | Other special tests include: | ||
| Line 110: | Line 125: | ||
*[[Impingement sign ankle]] | *[[Impingement sign ankle]] | ||
*[[Navicular Drop Test|Navicular drop test]] | *[[Navicular Drop Test|Navicular drop test]] | ||
For detailed information on these tests, please refer to the relevant pages with links provided. | |||
=== Balance | === Balance Tests === | ||
==== | ==== BESS Test ==== | ||
* Assessment tool for postural stability | |||
* Requires two testing surfaces, stopwatch and scoring sheet | |||
Detailed information can be found on the [[Balance Error Scoring System]] page. | |||
==== Star Excursion Balance Test (SEBT) ==== | ==== Star Excursion Balance Test (SEBT) ==== | ||
* Assesses anterior movements | |||
* Record the movements and compare results | |||
* Used to show progress | |||
* [[Y Balance Test|Y balance test]] is a short version of the Star test | |||
* see more here [[Star Excursion Balance Test]] | |||
{{#ev:youtube|v=GBT9V78d6E0|300}}<ref>Star Excursion Balance Test (SEBT).2017. Available from: https://www.youtube.com/watch?v=GBT9V78d6E0[last accessed 12/01/2022]</ref> | |||
=== Return to Sports Tests === | |||
The purpose of administering a return to sport test is to determine an individual's readiness to participate in high-level activities. | |||
Return to Sports Tests: | |||
* Help to determine the timing for a return to unrestricted activity. | |||
* Aim to decrease the risk of re-injury. | |||
* They test an athlete's ability to return to sport. They should mimic the athlete's activity. Example: '''single-leg hop''' or '''double-leg jump''' test for a long jumper with a history of a sprained ankle. Other examples include '''a jump to stability test''' or '''shuttle run.''' | |||
* They are not standardised. No data is available to support the use of one test versus a series of testing. | |||
* It is important to utilise a wide range of assessments: patient self-report questionnaires and assessment of psychological factors as examples. <ref>Manske R, Reiman M. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3658404/#bibr11-1941738113479925 Functional performance testing for power and return to sports]. Sports Health. 2013 May;5(3):244-50.</ref> | |||
* See also [[Return to Play in Sports]] | |||
=== Outcome Measures === | |||
Foot and ankle injuries are fairly common and the patient's progress and satisfaction with outcomes are the focus of all physiotherapy providers. Outcome measures used in different stages of rehabilitation help to monitor improvement in function and determine if there are further limitations preventing the patient from returning to sports or activities of daily living. The most commonly used self-reported outcome measures for foot and ankle injuries are as follows:<ref>Shultz S, Olszewski A, Ramsey O, Schmitz M, Wyatt V, Cook C. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3867077/ A systematic review of outcome tools used to measure lower leg conditions]. Int J Sports Phys Ther. 2013 Dec;8(6):838-48. </ref> | |||
*[[Foot and Ankle Ability Measure]] (FAAM) | |||
* Oxford Ankle Foot Questionnaire | |||
*[[Foot and Ankle Disability Index]] (FADI) | |||
* Lower‐Limb Tasks Questionnaire (LLTQ) | |||
* [[Foot Function Index (FFI)|Foot Function Index]] (FFI) | |||
* American Academy of Orthopaedic Surgeons (AAOS) Lower Limb Core Score/Foot and Ankle Module | |||
* Ankle Joint Functional Assessment Tool (AJFAT) | |||
* [[VISA-A scale|VISA-A Scale]] | |||
== Conclusion == | |||
Please watch the following video demonstrating the application and interpretation of special tests for the foot and ankle assessment:{{#ev: youtube|l6gkHR02rIM|400}}<ref>Kris Porter DPT. Movement Screen of the Lower Quarter. Available from: https://www.youtube.com/watch?v=l6gkHR02rIM [last accessed 30/6/2021]</ref> | |||
| Line 152: | Line 187: | ||
[[Category:Athlete Assessment]] | [[Category:Athlete Assessment]] | ||
[[Category:Sports Medicine]] | [[Category:Sports Medicine]] | ||
Latest revision as of 15:38, 22 October 2023
Original Editor - Ewa Jaraczewska
Top Contributors - Ewa Jaraczewska, Admin, Kim Jackson, Lucinda hampton, Samuel Adedigba, Nikhil Benhur Abburi, Jess Bell, Shejza Mino, Khloud Shreif, Rachael Lowe, Kai A. Sigel, Simisola Ajeyalemi, Rucha Gadgil, Wanda van Niekerk, Pinar Kisacik and Evan Thomas
Introduction[edit | edit source]
Taking a patient's history and completing an objective assessment is the gold standard for the foot and ankle assessment. The purpose of using special investigations and tests is to confirm the clinical diagnosis.
"We can't treat the patient just on x-rays or just on MRI findings. These things have to come together (with the objective assessment)". Helene Simpson
Investigations[edit | edit source]
X-Rays[edit | edit source]
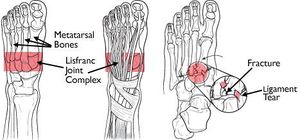
An X-ray can help to investigate bone and soft tissue:
- Assists with the diagnosis of the Achilles tendon rupture based on the presence of five radiological X-ray signs.[1] A lateral ankle X-ray is reliable to support the diagnosis of the Achilles tendon rupture.[1]
- May not be sufficient to identify malleolar fractures.[2]
- Syndesmosis injury is often overlooked on X-rays.[2]
- Assists with a diagnosis of an ankle fracture. AP, lateral and mortise views are recommended. Mortise view refers to the AP view with 15° internal rotation. If possible, the X-ray should be done with the patient in a standing position. The patient is advised to stand even with little weight (even 99 % on the un-injured foot). There are exceptions when there is an obvious dislocation / open fracture. When ankle fracture is ruled out, but there is no progress in patient's rehabilitation and the patient continues to complain of pain, an X-ray should be repeated within 6 weeks to rule out osteochondral lesion or hairline fracture.
- Malalignment of the second tarsometatarsal joint is a common feature in Lisfranc fracture-dislocations. The X-ray's AP view shows lateral displacement of the second metatarsal base and diastasis over 2 mm between the first and second metatarsal bases. It is recommended that an X-ray is taken of each foot in a weight-bearing position, so that the injured side can be compared to the contralateral side.[3]
- Hindfoot malalignment causes foot and ankle disability. The assessment of X-ray results of hindfoot alignment is important. The recommendation for a clinical and research purpose is to use the long axial hindfoot view in a bilateral stance. [4]
- The fracture of the sesamoid bone is shown on X-ray as a rough space between the bone pieces. A smooth separation of two bones visible on X-ray is a normal sign in about 10 % of the population.
- Ligament injuries were confirmed on a first diagnostic X-ray in only 50% of patients. This number increased to 66% of patients during the second X-ray when the diagnosis was confirmed.[5]
Diagnostic Ultrasound[edit | edit source]
Diagnostic ultrasound allows for dynamic examination of foot and ankle pathology. It is a non-invasive, economical and readily available tool that is recommended as a first-line diagnostic modality to rule out torn ligaments, tendonitis, tenosynovitis, plantar fascia, soft tissue masses or Morton's neuroma. [6] [7]
Diagnostic ultrasound was found to be an effective diagnostic tool for the following foot and ankle injuries:
- Fifth metatarsal, lateral and medial malleolus fractures in patients with foot and/or ankle sprains. Note: sensitivity for navicular fractures is low.[8]
- To rule out torn vs sprained anterior talofibular ligament and calcaneofibular ligament.[9][10][11]
- Ankle pain related to lateral ligament pathologies, tendinous pathologies, and joint effusion. Note: limited use in a suspected posterior talofibular ligament injury.[12]
- Achilles tendon injuries.[13]
- Statistically significant for diagnosing a syndesmosis injury at ≥6.0 mm of tibiofibular clear space widening.[14]
- Should be considered as a primary modality for foot and ankle fractures. [15]
MRI[edit | edit source]
MRI is the investigation of choice in chronic foot pain. Based on the available research MRI is a modality used in various foot and ankle soft tissue disorders due to its high resolution and contrast, but the interpretation of the results is key in proper diagnosis. MRI modality is expensive and not always easily accessible in many countries and it should be the orthopaedic surgeon who requests this particular investigation.
"It's fantastic to have a look at your soft tissue. If we're looking for cartilage injuries, it's sensitive, but it might overestimate the extent of the injury". Helene Simpson
MRI is:
- A gold standard for the diagnosis of Achilles tendon rupture.[1]
- Recommended in patients with ongoing pain at rest following ankle sprains as the clinical examination is insufficient when a syndesmotic injury is suspected.[16]
- A preoperative decisional tool for the anterior talofibular ligament repair in case of chronic lateral ankle instability.[17][18]
- A routine inspection method of the ankle ligament in the case of the ankle ligament injury. A weight-bearing MRI is recommended because the transverse position and the coronal position can show the full length of the ligament.[5]
- A valuable tool in the diagnosis of post-traumatic ankle pain as it has 96% accuracy in detecting tendon injury.[19]
- Advantageous for assessing tendons, ligaments, nerves, and fascia and for recognising occult bone injuries.[19]
- An investigation of choice for metatarsalgia due to its high resolution demonstrating sesamoid anatomy, plantar glenosesamoid apparatus, and the adjoining flexor, abductor, and adductor tendons.[20]
CT Scan[edit | edit source]
In the foot and ankle injury, the use of CT scan is proposed as a modality to assess the passive subsystem. It is a quick tool and it can be used during surgery. A weight-bearing computed tomography (WBCT) allows for the measurement and analysis of foot and ankle bone position and its deformities.[21] The recommendations for using a CT scan and WBCT are:
- To assess fractures in the ankle joint area.[2]
- To evaluate a syndesmotic reduction. A weight-bearing CT (WBCT) scan is proven to be more reliable.[22]
- To predict syndesmotic injuries in ankle fractures.[23]
- To characterise hindfoot alignment in order to determine the amount of translation needed for a neutral alignment during a calcaneal osteotomy.[24]
- To diagnose subtle Lisfranc instability.[25]
Special Tests[edit | edit source]
Ottawa Foot and Ankle Rules[edit | edit source]
Ottawa Ankle Rule determine the need for radiographs in acute ankle sprains. It is an accurate instrument for excluding fractures of the ankle and mid-foot, but the test has some limitations:
- High accuracy is true for the first 10 days post-injury
- High sensitivity is detected for patients younger than 55- years- old
Detailed information can be found on the Ottawa Ankle Rule page.
Knee To Wall Test[edit | edit source]
Should always be performed when assessing ankle and foot injury:
- Provides a means of assessing dorsiflexion range of motion at the ankle joint
- Recommended when conditions such as foot overpronation or plantar fasciitis are being examined
- Starting position for testing: toes against the wall and gradually moving away. The distance between the toes and the wall is measured with the ruler and is recorded for comparison and future reassessment.
Detailed information can be found on the Knee To Wall Test page.
Anterior Drawer Test[edit | edit source]
- Always performed in when assessing an ankle and foot injury
- Always compare with the "normal" side
- During the test remember to "hug" the calcaneus, because it moves the talus.
- See more here Anterior Drawer of the Ankle
Squeeze Test[edit | edit source]
- Performed to detect syndesmotic injury
- Attempting to reproduce pain symptoms
Detailed information can be found on the Squeeze Test page.
External Rotation Test[edit | edit source]
- Performed to detect a syndesmotic injury
- Attempting to reproduce a mechanism of the injury
Detailed information can be found on the External Rotation Test page.
Cotton Test[edit | edit source]
- Performed to detect syndesmotic instability
- It is a manual stress test
- It identifies the amount of the lateral translation of the talus within the ankle mortise
Coleman Block Test[edit | edit source]
- Performed to evaluate hindfoot flexibility and pronation of forefoot
- Completed by supporting the lateral forefoot on a woodblock that is 2.5-4 cm thick
- Determines if an inverted heel is due to a forefoot issue
Other Tests[edit | edit source]
Other special tests include:
- Ankle ligament stress tests
- Talar tilt test
- Eversion stress test
- Silfverskiöld test
- Windlass test
- Impingement sign ankle
- Navicular drop test
For detailed information on these tests, please refer to the relevant pages with links provided.
Balance Tests[edit | edit source]
BESS Test[edit | edit source]
- Assessment tool for postural stability
- Requires two testing surfaces, stopwatch and scoring sheet
Detailed information can be found on the Balance Error Scoring System page.
Star Excursion Balance Test (SEBT)[edit | edit source]
- Assesses anterior movements
- Record the movements and compare results
- Used to show progress
- Y balance test is a short version of the Star test
- see more here Star Excursion Balance Test
Return to Sports Tests[edit | edit source]
The purpose of administering a return to sport test is to determine an individual's readiness to participate in high-level activities.
Return to Sports Tests:
- Help to determine the timing for a return to unrestricted activity.
- Aim to decrease the risk of re-injury.
- They test an athlete's ability to return to sport. They should mimic the athlete's activity. Example: single-leg hop or double-leg jump test for a long jumper with a history of a sprained ankle. Other examples include a jump to stability test or shuttle run.
- They are not standardised. No data is available to support the use of one test versus a series of testing.
- It is important to utilise a wide range of assessments: patient self-report questionnaires and assessment of psychological factors as examples. [31]
- See also Return to Play in Sports
Outcome Measures[edit | edit source]
Foot and ankle injuries are fairly common and the patient's progress and satisfaction with outcomes are the focus of all physiotherapy providers. Outcome measures used in different stages of rehabilitation help to monitor improvement in function and determine if there are further limitations preventing the patient from returning to sports or activities of daily living. The most commonly used self-reported outcome measures for foot and ankle injuries are as follows:[32]
- Foot and Ankle Ability Measure (FAAM)
- Oxford Ankle Foot Questionnaire
- Foot and Ankle Disability Index (FADI)
- Lower‐Limb Tasks Questionnaire (LLTQ)
- Foot Function Index (FFI)
- American Academy of Orthopaedic Surgeons (AAOS) Lower Limb Core Score/Foot and Ankle Module
- Ankle Joint Functional Assessment Tool (AJFAT)
- VISA-A Scale
Conclusion[edit | edit source]
Please watch the following video demonstrating the application and interpretation of special tests for the foot and ankle assessment:
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Bowen L, Evans R, Bodger O, Howard J, Anne-Marie H. Investigating the Validity of Soft Tissue Signs on Lateral Ankle X-Ray to Aid Diagnosis of Achilles Tendon Rupture in the Emergency Department. Int J Foot Ankle. 2019;3:033.
- ↑ 2.0 2.1 2.2 Szymański T, Zdanowicz U. Comparison of routine computed tomography and plain X-ray imaging for malleolar fractures—How much do we miss?. Foot and Ankle Surgery. 2021 Apr 1.
- ↑ Stavlas P, Roberts CS, Xypnitos FN, Giannoudis PV. The role of reduction and internal fixation of Lisfranc fracture-dislocations: a systematic review of the literature. Int Orthop. 2010 Dec;34(8):1083-91.
- ↑ ML Reilingh, L Beimers, GJM Tuijthof, SAS Stufkens, M Maas, et al. Measuring hindfoot alignment radiographically: the long axial view is more reliable than the hindfoot alignment view. Skeletal radiology 2010;39 (11): 1103-1108.
- ↑ 5.0 5.1 Qi H, Feng Y. Analysis of the clinical value of weight-bearing magnetic resonance diagnosis of ankle ligament sports injury. IEEE Access. 2020 Mar 30;8:62725-37.
- ↑ Khoury V, Guillin R, Dhanju J, Cardinal É. Ultrasound of ankle and foot: overuse and sports injuries. Seminars in musculoskeletal radiology 2007 Jun; 11(02): 149-161.
- ↑ Rawool NM, Nazarian LN. Ultrasound of the ankle and foot. In: Seminars in Ultrasound, CT and MRI 2000 Jun; 21(3): 275-284.
- ↑ Atilla OD, Yesilaras M, Kilic TY, Tur FC, Reisoglu A, Sever M, Aksay E. The accuracy of bedside ultrasonography as a diagnostic tool for fractures in the ankle and foot. Academic Emergency Medicine. 2014 Sep;21(9):1058-61.
- ↑ Hosseinian SH, Aminzadeh B, Rezaeian A, Jarahi L, Naeini AK, Jangjui P. Diagnostic Value of Ultrasound in Ankle Sprain. The Journal of Foot and Ankle Surgery. 2021 Aug 20.
- ↑ Esmailian M, Ataie M, Ahmadi O, Rastegar S, Adibi A. Sensitivity and specificity of ultrasound in the diagnosis of a traumatic ankle injury. Journal of Research in Medical Sciences: The Official Journal of Isfahan University of Medical Sciences. 2021;26.
- ↑ Gribble PA. Evaluating and differentiating ankle instability. Journal of athletic training. 2019 Jun;54(6):617-27.
- ↑ Singh K, Thukral CL, Gupta K, Singh A. Comparison of high-resolution ultrasonography with clinical findings in patients with ankle pain. J Ultrason. 2018;18:316–24.
- ↑ Lee SH, Yun SJ. The feasibility of point-of-care ankle ultrasound examination in patients with a recurrent ankle sprain and chronic ankle instability: Comparison with magnetic resonance imaging. Injury. 2017;48:2323–8.
- ↑ Fisher CL, Rabbani T, Johnson K, Reeves R, Wood A. Diagnostic capability of dynamic ultrasound evaluation of supination-external rotation ankle injuries: a cadaveric study. BMC musculoskeletal disorders. 2019 Dec;20(1):1-7.
- ↑ Wu J, Wang Y, Wang Z. The diagnostic accuracy of ultrasound in the detection of foot and ankle fractures: a systematic review and meta-analysis. Medical Ultrasonography. 2021 May 20;23(2):203-12.
- ↑ Grossterlinden LG, Hartel M, Yamamura J, Schoennagel B, Burger N, Krause M, et al. Isolated syndesmotic injuries in acute ankle sprains: diagnostic significance of clinical examination and MRI. Knee Surg Sports Traumatol Arthrosc. 2016;24(4):1180–6.
- ↑ Morvan A, Klouche S, Thes A, Hardy P, Bauer T. Reliability and validity of preoperative MRI for surgical decision making in chronic lateral ankle instability. European Journal of Orthopaedic Surgery & Traumatology. 2018 May;28(4):713-9.
- ↑ Cao S, Wang C, Ma X, Wang X, Huang J, Zhang C, Wang K. Reliability and validity of different ankle MRI scanning planes for the anterior talofibular ligament injury diagnosis: a cadaveric study. Journal of orthopaedic surgery and research. 2019 Dec;14(1):1-8.
- ↑ 19.0 19.1 Elgohary MM, Abdul Rahim SA, Ibrahim TA. Role of MRI in Evaluation of Traumatic Ankle Injuries. The Egyptian Journal of Hospital Medicine. 2017 Oct 1;69(3):2016-24.
- ↑ Batta NS, Gupta A, Batra V. Imaging Findings of Bilateral Medial Hallucal Sesamoid Insufficiency in a Marathon Runner. Indian J Musculoskelet Radiol 2019;1(1):57-60.
- ↑ Rojas EO, Barbachan Mansur NS, Dibbern K, Lalevee M, Auch E, Schmidt E, Vivtcharenko V, Li S, Phisitkul P, Femino J, de Cesar Netto C. Weightbearing Computed Tomography for Assessment of Foot and Ankle Deformities: The Iowa Experience. Iowa Orthop J. 2021;41(1):111-119.
- ↑ Abdelaziz ME, Hagemeijer N, Guss D, El-Hawary A, El-Mowafi H, DiGiovanni CW. Evaluation of syndesmosis reduction on CT scan. Foot & ankle international. 2019 Sep;40(9):1087-93.
- ↑ Lee SW, Lee KJ, Park CH, Kwon HJ, Kim BS. The Valid Diagnostic Parameters in Bilateral CT Scan to Predict Unstable Syndesmotic Injury with Ankle Fracture. Diagnostics. 2020 Oct;10(10):812.
- ↑ Burssens A, Peeters J, Buedts K, Victor J, Vandeputte G. Measuring hindfoot alignment in weight-bearing CT: A novel clinical relevant measurement method. Foot Ankle Surg. 2016 Dec;22(4):233-238.
- ↑ Bhimani R, Sornsakrin P, Ashkani‐Esfahani S, Lubberts B, Guss D, De Cesar Netto C, Waryasz GR, Kerkhoffs GM, DiGiovanni CW. Using area and volume measurement via weight-bearing CT to detect Lisfranc instability. Journal of Orthopaedic Research®. 2021 Jan 6.
- ↑ The Weight Bearing Lunge Test. 2017. Available from: https://www.youtube.com/watch?v=wV9tITMsbDs [last accessed 12/01/2022]
- ↑ Kleiger's Test or External Rotation Test. 2013 Available from: https://www.youtube.com/watch?v=LnB1fta_rQA [last accessed 12/01/2022]
- ↑ UWECATEP. Cotton Test. 2013. Available from: https://www.youtube.com/watch?v=qX68KET3dls [last accessed 12/01/2022]
- ↑ Assessing Foot Flexibility: Part 05 (Modified Coleman Block Test). Available from: https://www.youtube.com/watch?v=TCp25F0l7hc [last accessed 6/6/2009]
- ↑ Star Excursion Balance Test (SEBT).2017. Available from: https://www.youtube.com/watch?v=GBT9V78d6E0[last accessed 12/01/2022]
- ↑ Manske R, Reiman M. Functional performance testing for power and return to sports. Sports Health. 2013 May;5(3):244-50.
- ↑ Shultz S, Olszewski A, Ramsey O, Schmitz M, Wyatt V, Cook C. A systematic review of outcome tools used to measure lower leg conditions. Int J Sports Phys Ther. 2013 Dec;8(6):838-48.
- ↑ Kris Porter DPT. Movement Screen of the Lower Quarter. Available from: https://www.youtube.com/watch?v=l6gkHR02rIM [last accessed 30/6/2021]