Chondromalacia Patellae: Difference between revisions
No edit summary |
No edit summary |
||
| (37 intermediate revisions by 9 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox">'''Original Editors '''- [[User:Francky Petit|Francky Petit]] as part of the [[Vrije Universiteit Brussel Evidence-based Practice Project|Vrije Universiteit Brussel's Evidence-based Practice project]] | ||
'''Original Editors '''- [[User:Francky Petit|Francky Petit]] | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Definition/Description == | == Definition/Description == | ||
Chondromalacia patellae (CMP) is referred as anterior knee pain due to the physical and biomechanical changes <ref name="Lee Herrington et al."> | Chondromalacia patellae (CMP) is referred to as anterior knee pain due to the physical and biomechanical changes <ref name="Lee Herrington et al.">Herrington L, Al-Sherhi A. [https://pubmed.ncbi.nlm.nih.gov/17469667/ A controlled trial of weight-bearing versus non-weight-bearing exercises for patellofemoral pain]. J Orthop Sports Phys Ther. 2007 Apr;37(4):155-60. doi: 10.2519/jospt.2007.2433. </ref>. The articular cartilage of the posterior surface of the patella is going though degenerative changes <ref name="radiography">http://www.e-radiography.net/radpath/c/chondromalaciap.htm</ref> which manifest as a softening, swelling, fraying, and erosion of the hyaline cartilage underlying the patella and sclerosis of the underlying bone. <ref name="gagliardi">Gagliardi JA, Chung EM, Chandnani VP, Kesling KL, Christensen KP, Null RN, et al. [https://www.ajronline.org/doi/10.2214/ajr.163.3.8079858 Detection and staging of chondromalacia patellae: relative efficacies of conventional MR imaging, MR arthrography, and CT arthrography]. AJR Am J Roentgenol. 1994 Sep;163(3):629-36. doi: 10.2214/ajr.163.3.8079858. </ref> | ||
Chondromalacia patellae is one of the most frequently encountered causes of anterior knee pain among young people. It’s the number one cause in the United States with an incidence as high as one in four people.< | Chondromalacia patellae is one of the most frequently encountered causes of anterior knee pain among young people. It’s the number one cause in the United States with an incidence as high as one in four people.<ref name=":7">Laprade J, Culham E, Brouwer B. [https://pubmed.ncbi.nlm.nih.gov/9513865/ Comparison of five isometric exercises in the recruitment of the vastus medialis oblique in persons with and without patellofemoral pain syndrome]. J Orthop Sports Phys Ther. 1998; 27: 197–204 | ||
</ref> The word chondromalacia is derived from the Greek words - chrondros, meaning cartilage, and malakia, meaning softening. Hence chondromalacia patellae is a softening of the articular cartilage on the posterior surface of the patella which may eventually lead to fibrillation, fissuring, and erosion.<ref name=":6">Gordon HM. [https://www.sciencedirect.com/science/article/pii/S000495141461028X?via%3Dihub Chondromalacia patellae]. Aust J Physiother. 1977 Sep;23(3):103-6. doi: 10.1016/S0004-9514(14)61028-X.</ref> | |||
The differential diagnosis of chondromalacia includes [[Patellofemoral Pain Syndrome|patellofemoral pain syndrome]] and [[patellar tendinopathy|patellar tendinopathy]]. Chondromalacia patella is not considered to be under the umbrella term of PFPS.<ref name=":4">Wiles P, Andrews PS, Devas MB. [https://boneandjoint.org.uk/Article/10.1302/0301-620X.38B1.95 Chondromalacia of the patella]. Bone & Joint Journal. 1956 Feb 1;38(1):95-113.</ref><ref>Blazer K. Diagnosis and treatment of patellofemoral pain syndrome in the female adolescent. Physician Assistant. 2003 Sep 1;27(9):23-30.</ref><ref name=":5">Fernández-Cuadros ME, Albaladejo-Florín MJ, Algarra-López R, Pérez-Moro OS. [https://www.imbiodent.com/articulos/imagenes/articulos/pdfs/116/50.-efficiency-of-plateletrich-plasma-prp-comparedto-ozone-infiltrations-on-patellofemoral-painsyndrome-and-chondromalacia-_-1-.pdf Efficiency of Platelet-rich Plasma (PRP) Compared to Ozone Infiltrations on Patellofemoral Pain Syndrome and Chondromalacia: A Non-Randomized Parallel Controlled Trial]. Diversity & Equality in Health and Care. 2017 Aug 4;14(4):203-211</ref> The pathophysiology is different and therefore there is an alternative treatment.<ref name=":4" /><ref name=":5" />Chondromalacia patella can be present in patellofemoral pain but not everyone with patellofemoral pain syndrome will have chondromalacia patella.<ref>Willy RW, Hoglund LT, Barton CJ, Bolgla LA, Scalzitti DA, Logerstedt DS, Lynch AD, Snyder-Mackler L, McDonough CM. [https://www.jospt.org/doi/10.2519/jospt.2019.0302?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed Patellofemoral Pain]. J Orthop Sports Phys Ther. 2019 Sep;49(9):CPG1-CPG95. doi: 10.2519/jospt.2019.0302. </ref> | |||
== Clinically Relevant Anatomy [[Image:Vastus.png|thumb|right]] | == Clinically Relevant Anatomy == | ||
[[Image:Vastus.png|thumb|right]] | |||
The knee comprises 4 major bones: the femur, tibia, fibula and the patella. The patella articulates with the femur at the trochlear groove. <ref>http://emedicine.medscape.com/article/1898986-overview#aw2aab6b3 fckLR</ref> Articular cartilage on the underside of the patella allows the patella to glide over the femoral groove, necessary for efficient motion at the knee joint. <ref name="Anderson">Anderson MK. Fundamentals of Sports Injury Management, second edition, Lippincott Williams & Wilkins, 2003, p. 208</ref> Excess and persistent turning forces on the lateral side of the knee can harm the nutrition of the articular cartilage and more specifically in the medial and central area of the patella, where degenerative change will occur more readily. <ref name="Beeton">Beeton KS. Manual Therapy Masterclasses: The Peripheral Joints, Churchill Livingstone, 2003, p.50-51</ref> | |||
The | The quadriceps insert into the patella via the quadriceps tendon and are divided into four separate muscles: rectus femoris (RF), vastus lateralis (VL), vastus intermedius (VI) and vastus medialis (VM). The VM has oblique fibres which are referred to as the vastus medialis obliques (VMO)<ref name="spieren">Kendall FP, Hulsman P, Zuidgeest A. Spieren: tests en functies, Nederland:Bohn Stafleu van Loghum, 469p (383)</ref> | ||
These muscles are active stabilisers during knee extension, especially the VL (on the lateral side) and the VMO (on the medial side). The VMO is active during knee extension but does not extend the knee. Its function is to keep the patella centred in the trochlea. This muscle is the only active stabiliser on the medial aspect, so its functional timing and amount of activity are critical to patellofemoral movement, the smallest change having significant effects on the position of the patella. [[Image:Femoral groove.png|thumb|right]]Not only do the quadriceps influence the patella position, but also the passive structures of the knee. These passive structures are more extensive and stronger on the lateral side than the medial side, with most of the lateral retinaculum arising from the iliotibial band (ITB). If the ITB is under excessive tension, excessive lateral tracking and/or lateral patellar tilt can occur. This is because the tensor fasciae lata is tight, as the ITB itself is a non-contractile structure.<ref name="Beeton" />.<br> | |||
These muscles are active stabilisers during knee extension, especially the VL (on the lateral side) and the VMO (on the medial side). The VMO is active during knee extension | |||
Other significant anatomical structures: [[Image:Q angle.png|thumb|right]] | Other significant anatomical structures: [[Image:Q angle.png|thumb|right]] | ||
*Femoral anteversion <ref name="Nyland"> | *Femoral anteversion <ref name="Nyland">Nyland J, Kuzemchek S, Parks M, Caborn DN. [https://www.sciencedirect.com/science/article/abs/pii/S1050641103000786?via%3Dihub Femoral anteversion influences vastus medialis and gluteus medius EMG amplitude: composite hip abductor EMG amplitude ratios during isometric combined hip abduction-external rotation]. J Electromyogr Kinesiol. 2004 Apr;14(2):255-61. doi: 10.1016/S1050-6411(03)00078-6. </ref> or medial torsion of the femur is a condition that changes the alignment of the bones at the knee. This may lead to overuse injuries of the knee due to malalignment of the femur to the patella and tibia. <ref name="Milner">Milner CE. Functional Anatomy For Sport And Exercise: Quick Reference, Routledge, 2008, p58-60 </ref> | ||
*The [[Q Angle|Q-angle]]: or quadriceps angle is the geometric relationship between the pelvis, the tibia, the patella and the femur<ref name="Milner" /><ref name="Singh">Singh V. Clinical And Surgical Anatomy, second edition, Elsevier, 2007, p228- 230. </ref> and is defined as the angle between the first line from the anterior superior iliac spine to the centre of the patella and the second line from the centre of the patella to the tibial tuberosity <ref>Asseln M, Eschweiler J, Zimmermann F, Radermacher K. [https://www.degruyter.com/document/doi/10.1515/bmt-2013-4115/html The Q-Angle and its Effect on Active Knee Joint Kinematics - a Simulation Study]. Biomed Tech (Berl). 2013 Aug;58 Suppl 1:/j/bmte.2013.58.issue-s1-D/bmt-2013-4115/bmt-2013-4115.xml. doi: 10.1515/bmt-2013-4115. </ref>. | |||
*The [[ | |||
If there is | If there is increased adduction and/or internal rotation of the hip, the Q-angle will increase, which increases the relative valgus of the lower extremity. This higher Q-angle and valgus will increase the contact pressure on the lateral side of the patellofemoral joint (which is also increased by external rotation of the tibia) <ref name=":0">Meira EP, Brumitt J. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3445210/ Influence of the hip on patients with patellofemoral pain syndrome: a systematic review]. Sports Health. 2011 Sep;3(5):455-65. doi: 10.1177/1941738111415006. </ref> | ||
== Epidemiology /Etiology == | == Epidemiology /Etiology == | ||
The | The aetiology of CMP is poorly understood, although it is believed that the causes of chondromalacia are injury, generalised constitutional disturbance and patellofemoral contact <ref name="iraj salehi">Salehi I, Khazaeli S, Hatami P, Malekpour M. [https://link.springer.com/article/10.1007/s00296-009-1149-3 Bone density in patients with chondromalacia patella]. Rheumatol Int. 2010 Jun;30(8):1137-8. doi: 10.1007/s00296-009-1149-3.</ref>, or as a result of trauma to the chondrocytes in the articular cartilage (leading to proteolytic enzymatic digestion of the superficial matrix). It may also be caused by instability or maltracking of the patella which softens the articular cartilage. <ref name="Macmull">Macmull S, Jaiswal PK, Bentley G, Skinner JA, Carrington RW, Briggs TW. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3385894/ The role of autologous chondrocyte implantation in the treatment of symptomatic chondromalacia patellae]. Int Orthop. 2012 Jul;36(7):1371-7. doi: 10.1007/s00264-011-1465-6. </ref> Chondromalacia patella is usually described as an overload injury, caused by malalignment of the femur to the patella and the tibia. <ref>Bartlett R. Encyclopedia of International Sports Studies, Routledge, 2010, p90.</ref> | ||
Hamstrings: during running tight hamstrings increase knee flexion | Main reasons for patellar malalignment; | ||
* Q-angle: An abnormality of the Q-angle is one of the most significant factors of patellar malalignment. A normal Q-angle is 14° for men and 17° for women. An increase can result in an increased lateral pull on the patella. | |||
* Muscular tightness of: | |||
** Rectus femoris: affects patellar movement during flexion of the knee. | |||
** Tensa Fascia late; affects the influence of the ITB | |||
** Hamstrings: during running, tight hamstrings increase knee flexion resulting to increased ankle dorsiflexion. This causes compensatory pronation in the talocrural joint. | |||
** Gastrocnemius: tightness will result in compensatory pronation in the subtalar joint. | |||
* Excessive pronation: prolonged pronation of the subtalar joint is caused by internal rotation of the leg. This internal rotation will result in malalignment of the patella. | * Excessive pronation: prolonged pronation of the subtalar joint is caused by internal rotation of the leg. This internal rotation will result in malalignment of the patella. | ||
* Patella alta: this is a condition where the patella is positioned in an abnormally superior position. | * Patella alta: this is a condition where the patella is positioned in an abnormally superior position. It is present when the length of the patellar tendon is 20% greater than the height of the patella. | ||
* Vastus medialis insufficiency: the function of the vastus medialis is to realign the patella during knee extension. If the strength of VM is insufficient this will cause a lateral drift of the patella.<ref> | * Vastus medialis insufficiency: the function of the vastus medialis is to realign the patella during knee extension. If the strength of VM is insufficient this will cause a lateral drift of the patella.<ref>McConnell J. The management of chondromalacia patellae: a long term solution. Australian Journal of Physiotherapy; 1986, 32(4): 215-223</ref> | ||
A muscular balance between the VL and VM is important. Where VM is weaker the patella is pulled too far laterally which can cause increased contact with the condylus lateralis, leading to degenerative disease.<ref name="aafp">http://www.aafp.org/afp/991101ap/2012.htm</ref> | |||
Degenerative changes of the articular cartilage can be caused by <ref name="Logan"> | Degenerative changes of the articular cartilage can be caused by <ref name="Logan">Logan AL. The Knee Clinical Applications. Aspen Publishers, 1994, p131.</ref>: | ||
*Trauma: instability caused by | *Trauma: instability caused by previous trauma or overuse during recovery | ||
*Repetitive microtrauma and inflammatory conditions | |||
*Repetitive | *Postural distortion: causes malposition or dislocation of the patella in the trochlear groove | ||
Hip positioning and strength are linked to the prevalence of patellofemoral pain syndrome. Therefore, hip strengthening and stability exercises may be useful in the treatment program of patellofemoral pain syndrome.<ref name=":0" /> | |||
Some authors use the term “patellar pain syndrome” instead of “chondromalacia” to describe “anterior knee pain”. <ref name="Manske">Manske RC. Postsurgical Orthopedic Sports Rehabilitation: Knee & Shoulder, 2006, Mosby:Elsevier, p446-451.</ref> | |||
== Stages of the Disease == | |||
In the early stages, chondromalacia shows areas of high sensitivity to fluid sequences. This can be associated with the increased thickness of the cartilage and may also cause oedema. In the latter stages, there will be a more irregular surface with focal thinning that can expand to and expose the subchondral bone. <ref name="Wessely">Wessely M, Young M. Essential Musculoskeletal MRI: A Primer for the Clinician. Churchill Livingstone Elsevier, 2011, p115.</ref> | |||
Chondromalacia patella is graded based on arthroscopic findings, the depth of cartilage thinning and associated subchondral bone changes. Moderate to severe stages can be seen on [[MRI Scans|MRI]]. <ref name="Munk">Munk PL, Ryan AG. Teaching Atlas of Musculoskeletal Imaging. Thieme, 2008, p68-70.</ref> | |||
*Stage 1: softening and swelling of the articular cartilage due to broken vertical collagenous fibres. The cartilage is spongy on arthroscopy. | *Stage 1: softening and swelling of the articular cartilage due to broken vertical collagenous fibres. The cartilage is spongy on arthroscopy. | ||
*Stage 2: blister formation in the articular cartilage due to the separation of the superficial from the deep cartilaginous layers. Cartilaginous fissures affecting less than 1,3 cm² in area with no extension to the subchondral bone. | |||
*Stage 2: blister formation in the articular cartilage due to the separation of the superficial from the deep cartilaginous layers. Cartilaginous fissures affecting less than 1,3 | |||
*Stage 3: fissures ulceration, fragmentation, and fibrillation of cartilage extending to the subchondral bone but affecting less than 50% of the patellar articular surface. | *Stage 3: fissures ulceration, fragmentation, and fibrillation of cartilage extending to the subchondral bone but affecting less than 50% of the patellar articular surface. | ||
*Stage 4: crater formation and eburnation of the exposed subchondral bone more than 50% of the patellar articular surface exposed, with sclerosis and erosions of the subchondral bone. Osteophyte formation also occurs at this stage. | *Stage 4: crater formation and eburnation of the exposed subchondral bone more than 50% of the patellar articular surface exposed, with sclerosis and erosions of the subchondral bone. Osteophyte formation also occurs at this stage. | ||
Articular cartilage does not have any nerve endings, so CMP should not be considered as a true source of anterior knee pain, rather, it is a pathological or surgical finding that represents areas of articular cartilage trauma or divergent loading. <ref name="Anderson" /> ''Kok et al'' showed that there is a significant association between subcutaneous knee fat thickness with the presence and severity of chondromalacia patellae. This could explain why women suffer more from the condition of chondromalacia than men.<ref>Kok HK, Donnellan J, Ryan D, Torreggiani WC. [https://www.sciencedirect.com/science/article/pii/S0846537112000423?via%3Dihub Correlation between subcutaneous knee fat thickness and chondromalacia patellae on magnetic resonance imaging of the knee]. Can Assoc Radiol J. 2013 Aug;64(3):182-6. doi: 10.1016/j.carj.2012.04.003. </ref> | |||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
There are important distinguishing features between chondromalacia patellae and [[Knee Osteoarthritis|Osteoarthritis]]. CMP affects just one side of the joint, the convex patellar side, <ref> | There are important distinguishing features between chondromalacia patellae and [[Knee Osteoarthritis|Osteoarthritis]]. CMP affects just one side of the joint, the convex patellar side, <ref>Ellis H, French H, Kinirons MT. French’s Index of differential diagnosis. 14th edition, Hodder Arnold Publishers, 2005. </ref> with excised patellas show localised softening and degeneration of the articular cartilage. <ref>Anderson JR. Muir’s Textbook of Pathology. 12th edition, Lippincott Williams Wilkins, 1988</ref> The main symptom of chondromalacia patellae is anterior knee pain,<ref name="iraj salehi" /> which is exacerbated by common daily activities that load the patellofemoral joint, such as running, stair climbing, squatting, kneeling <ref name="Lee Herrington et al." />, or changing from a sitting to a standing position <ref>Moeckel E, Noori M. Textbook of Pediatric Osteopathy. Elsevier Health Sciences, 2008, p338.</ref>. The pain often causes disability affecting the short-term participation of daily and physical activities.<ref name="Bill Vicenzino">Vicenzino B, Collins N, Crossley K, Beller E, Darnell R, McPoil T. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2279129/ Foot orthoses and physiotherapy in the treatment of patellofemoral pain syndrome: a randomised clinical trial]. BMC Musculoskelet Disord. 2008 Feb 27;9:27. doi: 10.1186/1471-2474-9-27. PMID: 18304317; PMCID: PMC2279129.</ref> Other symptoms are tenderness on palpating under the medial or lateral border of the patella, <ref name="Shultz">Shultz SJ, Houglum PA, Perrin DH. Examination of Musculoskeletal injuries. 3rd edition. Human Kinetics, 2010, p453.</ref> crepitation (felt with motion), <ref name=":1">DeGowin RL, DeGowin EL. DeGowin & DeGowin’s Diagnostic Examination. 6th edition. McGraw Hill, 1994, p735. </ref>; minor swelling, <ref name="Shultz" /> a weak vastus medialis muscle and a high Q-angle. <ref>Ebnezar J, Textbook of Orthopedics. 4th edition. India:JP Medical Ltd, 2010, p426-427. </ref> Vastus medialis is functionally divided into two components: the vastus medialis longus (VML) and the vastus medialis obliquus (VMO). The VML extends the knee, with the rest of the quadriceps muscle. The VMO does not extend the knee but is active throughout the knee extension. This component assists in keeping the patella centred in the femoral trochlea. <ref name="Beeton" /> | ||
This condition can cause a deficit in quadriceps strength, therefore, building and/or maintaining quadriceps strength is essential.<ref name="Lee Herrington et al." /> A significant number of individuals are asymptomatic, but crepitation in flexion or extension is often present. <ref name="Murray">Murray RO, Jacobson HG. The Radiology of Skeletal Disorders: exercises in diagnosis. 2nd edition. Churchill Livingstone, 1990, p306-307.</ref>Chondromalacia is common in adolescents and females with idiopathic chondromalacia usually seen in young children and adolescents and the degenerative condition is most common in the middle-aged and older population. <ref name="Wessely" /> | |||
== Differential Diagnosis == | == Differential Diagnosis == | ||
| Line 89: | Line 80: | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
Since its first description by Budinger in 1906, chondromalacia patella has been of significant clinical interest because diagnosis is often difficult. The chief reason for this is that the aetiology is often unknown and the correlation between the articular cartilage changes and the clinical system is poor. Patients affected by chondromalacia patella are young, between 15 and 35 years old, and many are highly active and are often considerably disabled by the symptoms of aching behind the patella, recurrent effusion of the knee, knee instability | Since its first description by Budinger in 1906, chondromalacia patella has been of significant clinical interest because diagnosis is often difficult. The chief reason for this is that the aetiology is often unknown and the correlation between the articular cartilage changes and the clinical system is poor. Patients affected by chondromalacia patella are young, between 15 and 35 years old, and many are highly active and are often considerably disabled by the symptoms of aching behind the patella, recurrent effusion of the knee, knee instability and crepitus.<ref>Bentley G, Lesly IJ, Fischer D. Effect of aspirin treatment on chondromalacia patella. Annals of the rheumatic diseases, 1981; 40:37-41.</ref> | ||
The primary diagnostic approach for chondromalacia patellae is radiography with added arthrography. | The primary diagnostic approach for chondromalacia patellae is radiography with added arthrography. Pinhole scintigraphy, part of arthrography, is also used to diagnose the condition. <ref>Bahk YW, Park YH, Chung SK, Kim SH, Shinn KS. Pinhole scintigraphic sign of chondromalacia patellae in older subjects: a prospective assessment with differential diagnosis. J Nucl Med. 1994;35:855–862.</ref> MRI is an effective, non-invasive method with the ability to increase the sensitivity and specificity of the diagnosis.<ref>Kim HJ, Lee SH, Kang CH, Ryu JA, Shin MJ, Cho KJ, et al. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3017887/ Evaluation of the chondromalacia patella using a microscopy coil: comparison of the two-dimensional fast spin echo techniques and the three-dimensional fast field echo techniques]. Korean J Radiol. 2011 Jan-Feb;12(1):78-88. doi: 10.3348/kjr.2011.12.1.78. </ref> | ||
== Outcome Measures == | == Outcome Measures == | ||
There are | There are various measures: <ref>Crossley KM, Bennell KL, Cowan SM, Green S. Analysis of outcome measures for persons with patellofemoral pain: which are reliable and valid? Arch Phys Med Rehabil. 2004 May;85(5):815-22. doi: 10.1016/s0003-9993(03)00613-0. </ref><ref name=":3">Petersen W, Ellermann A, Rembitzki IV, Scheffler S, Herbort M, Brüggemann GP, et al. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4908172/ Evaluating the potential synergistic benefit of a realignment brace on patients receiving exercise therapy for patellofemoral pain syndrome: a randomized clinical trial]. Arch Orthop Trauma Surg. 2016 Jul;136(7):975-82. doi: 10.1007/s00402-016-2464-2. </ref> | ||
* Anterior Knee Pain Scale: a 13 item questionnaire with categories related to various levels of current knee function. | * Anterior Knee Pain Scale: a 13-item questionnaire with categories related to various levels of current knee function. | ||
* Visual analog scale | * Visual analog scale | ||
*The five KOOS subscales: a scale about | *The five KOOS subscales: a scale about patients' experience over time with knee conditions. It consists of five subscales: Pain, other Symptoms, Function in daily living, Function in sport and recreation and knee-related Quality of life. | ||
== <br> | == Examination == | ||
Examination of the knee is 4 fold: observation, mobility, feel, X-ray.<ref name=":6" /> | |||
* '''Observation''': joint appearance is usually normal, but there may be a slight effusion. | |||
* '''Mobility''': passive movements are usually full and painless, but repeated extension of the knee from flexion will produce pain and a grating feeling underneath the patella, especially if the articular surfaces are compressed together. | |||
* '''Feel''': Pain and crepitus will be felt if the patella is compressed against the femur, either vertically or horizontally, with the knee in full extension. By displacing the patella medially or laterally, the patellar margins and their articular surfaces may be felt. Tenderness of one or other margin may be elicited and more frequently felt medially. Resisting a static quadriceps contraction will generally produce a sharp pain under the patella. This may be apparent in both knees, but more severe on the affected side. | |||
* '''X-ray:''' an AP view of the patellofemoral joint is needed to detect any radiological change. In all but the most advanced cases, there is no convincing radiological change. In the latter stages, patellofemoral joint space narrows and osteoarthritic changes begin to appear.<br> | |||
=== Tests === | |||
The patient's posture can be an initial clue as well as any observed asymmetries, such as; limb alignment in standing, internal femoral rotation, anterior or posterior pelvic tilt, hyperextended or ‘locked back’ knees, genu varum or valgum and abnormal pronation of the foot. Gait patterns may also be affected. <ref name="spieren" /> | |||
Mobility and range of motion (ROM) of the joint are tested, which can be limited. if bursitis is present, passive flexion or active extension will be painful. Loss of power in the affected leg may also be present on isometric testing. There are specific tests for anterior knee pain syndrome: <ref name=":1" /> | |||
*[http://www.physio-pedia.com/Patellar_Grind_Test Patellar | *[http://www.physio-pedia.com/Patellar_Grind_Test Patellar grind test] or Clarke’s sign: This test detects the presence of patellofemoral joint disorder. A positive sign on this test is a pain in the patellofemoral joint. | ||
*Compression test | *Compression test | ||
*[http://www.physio-pedia.com/Knee_Extension_Resistance_Test Extension-resistance test] | *[http://www.physio-pedia.com/Knee_Extension_Resistance_Test Extension-resistance test]: This test is used to perform a maximal provocation on the muscle-tendon mechanism of the extensor muscles and is positive when the affected knee demonstrates less power when trying to maintain the pressure. | ||
*The critical test: This | *The critical test: This is done with the patient in high sitting and performing isometric quadriceps contractions at 5 different angles (0°, 30°, 60°, 90° and 120°) while the femur is externally rotated, sustaining the contractions for 10 seconds. If pain is produced then the leg is positioned in full extension. In this position, the patella and femur have no more contact. The lower leg of the patient is supported by the therapist so the quadriceps can be fully relaxed. When the quadriceps is relaxed, the therapist can glide the patella medially. This glide is maintained while the isometric contractions are again performed. If this reduces the pain and the pain is patellofemoral in origin, there is a high chance of a favourable outcome.<ref name=":7" /> | ||
It is possible to diagnose incorrectly and these tests may aid in determining chondromalacia, but other possible conditions also need to be excluded. | |||
== Medical Management | == Medical Management == | ||
Exercise and education are two | Exercise and education are two important aspects of a treatment programme. Education helps the patient to understand the condition and how they should deal with it for optimal recovery. Exercise focus is on stretching and strengthening appropriate structures, such as the hamstring, quadriceps and gastrocnemius length and strength of the gluteal muscles.<ref name=":2">Clark DI, Downing N, Mitchell J, Coulson L, Syzpryt EP, Doherty M. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1753277/ Physiotherapy for anterior knee pain: a randomised controlled trial]. Ann Rheum Dis. 2000 Sep;59(9):700-4. doi: 10.1136/ard.59.9.700.</ref> Fire needling and acupuncture may also relieve clinical symptoms of chondromalacia patellae and recover the biodynamical structure of the patellae. <ref>Huang J, Li L, Lou BD, Tan CJ, Liu Z, Ye Y, et al. [[https://pubmed.ncbi.nlm.nih.gov/25112086/ Efficacy observation on chrondromalacia patellae treated with fire needling technique at high stress points]]. Zhongguo Zhen Jiu. 2014 Jun;34(6):551-4. </ref> | ||
If conservative measures fail | If conservative measures fail, there are several possible surgical procedures. <ref name="Munk" /> | ||
* '''Chondrectomy''': also known as shaving. This treatment includes shaving down the damaged cartilage to the non-damaged cartilage underneath. The success of this treatment depends on the severity of the cartilage damage. | |||
* '''Drilling''' is also a method that is frequently used to heal damaged cartilage. However, this procedure has not so far been proven to be effective. More localised degeneration might respond better to drilling small holes through the damaged cartilage. This facilitates the growth of healthy tissue through the holes from the layers underneath. | |||
* '''Full patellectomy''': This is the most severe surgical treatment. This method is only used when no other procedures are helpful, but a significant consequence is that the quadriceps will become weak. | |||
Two other treatments that may be successful: <ref name="Logan" /> | |||
*'''Replacement of the damaged cartilage:''' The damaged cartilage is replaced by a polyethylene cap prosthesis. Early results have been good, but the eventual wearing of the opposing articular surface is inevitable. | |||
*'''Autologous chondrocyte transplantation''' under a tibial periosteal patch. <ref name="Logan" /> | |||
Simply removing the cartilage is not a cure for chondromalacia patellae. The biomechanical deficits need addressing and there are various procedures to aid in managing this. | |||
* Tightening of the medial capsule (MC): If the MC is lax, it can be tightened by pulling the patella back into its correct alignment. | |||
* Lateral release: A very tight lateral capsule will pull the patella laterally. Release of the lateral patellar retinaculum allows the patella to track correctly into the femoral groove. | |||
* Medial shift of the tibial tubercle: Moving the insertion of the quadriceps tendon medially at the tibial tubercle, allows the quadriceps to pull the patella more directly. It also decreases the amount of wear on the underside of the patellar. | |||
* Partial removal of the patella | |||
Although there is no overall agreement for the treatment of chondromalacia, the consensus is that the best treatment is a non-surgical one.<ref name="r.van linschoten">van Linschoten R, van Middelkoop M, Berger MY, Heintjes EM, Verhaar JA, Willemsen SP, et al. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2764849/ Supervised exercise therapy versus usual care for patellofemoral pain syndrome: an open-label randomised controlled trial]. BMJ. 2009 Oct 20;339:b4074. doi: 10.1136/bmj.b4074. </ref> | |||
== Physical Therapy Management == | |||
=== Exercise Program === | |||
Conservative treatment of chondromalacia patellae is both physical and highly advised. Short-wave diathermy can help to relieve pain and to increase the blood supply to the area, improving the nutrition supply to the articular cartilage. Care must be taken when planning an exercise programme.<ref name=":2" /> Conservative therapeutic interventions include the following:<ref name=":8" /> | |||
*Isometric quadriceps strengthening and stretching exercises<ref name="Lee Herrington et al." /> Restoration of adequate quadriceps strength and function is an essential factor in achieving good recovery. The most effective exercises are isometric and isotonic in the inner range. Isotonic exercises through a full range of motion will only lead to increased pain and even joint effusion.<ref name=":2" /> Stretching of the vastus lateralis and strengthening of the vastus medialis is often recommended, but they are difficult to isolate due to shared innervation and insertion.<ref name="spieren" /><ref name="aafp" />It has shown that closed kinematic chain exercises can improve patellofemoral joint performance by increasing quadriceps muscle strength and patellar alignment correction.<ref>Bakhtiary AH, Fatemi E. [https://bjsm.bmj.com/content/42/2/99.long Open versus closed kinetic chain exercises for patellar chondromalacia]. Br J Sports Med. 2008 Feb;42(2):99-102; discussion 102. doi: 10.1136/bjsm.2007.038109. </ref> | |||
== | |||
Conservative treatment of chondromalacia patellae is both physical and | |||
*Hamstring stretching exercises | *Hamstring stretching exercises | ||
*Temporary modification of activity | *Temporary modification of activity | ||
*Patellar taping | *Patellar taping | ||
*Foot orthoses | *Foot orthoses | ||
* | *NSAIDs | ||
*Hip strength and stability training, as hip positioning and strength have a significant influence on anterior knee pain. | |||
*Hip abductor strengthening as an increased hip adduction angle is associated with weakened hip abductors.<ref name="Bleakley C" /> | |||
*Patellar realignment brace<ref name=":3" /> | |||
''<u></u>'' | |||
* | |||
< | Not only is strengthening important, but stretching should also be part of the programme. <ref name="Anderson" /> It has been shown that patients with patellofemoral pain syndrome have shorter and less flexible hamstrings than asymptomatic individuals.. Although stretching can improve flexibility and knee function, it doesn’t necessarily directly improve pain.<ref>Harvie D, O'Leary T, Kumar S. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3215347/ A systematic review of randomized controlled trials on exercise parameters in the treatment of patellofemoral pain: what works?] J Multidiscip Healthc. 2011;4:383-92. doi: 10.2147/JMDH.S24595.</ref> | ||
< | Another form of therapy is warm needling. In combination with rehabilitation exercises, it has a prolonged pain-relieving effect than in warm needling in combination with medication<ref>Qiu L, Zhang M, Zhang J, Gao LN, Chen DW, Liu J, et al. [https://www.sciencedirect.com/science/article/pii/S025462720960039X Chondromalacia patellae treated by warming needle and rehabilitation training]. J Tradit Chin Med. 2009 Jun;29(2):90-4. doi: 10.1016/s0254-6272(09)60039-x.</ref> | ||
=== Ice Medication === | |||
< | Ice may be useful for reducing pain in an acute flare-up, but not as a long-term treatment protocol.<ref name="Bleakley C">Bleakley C, McDonough S, MacAuley D. [https://journals.sagepub.com/doi/10.1177/0363546503260757?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed The use of ice in the treatment of acute soft-tissue injury: a systematic review of randomized controlled trials]. Am J Sports Med. 2004 Jan-Feb;32(1):251-61. doi: 10.1177/0363546503260757. </ref> NSAIDs may also be of benefit in the short term to relieve pain so that knee function and mobility are normalised and an exercise programme can begin. | ||
=== Taping and Braces === | |||
Taping the patella to influence its movement may provide some short-term relief, but the evidence is varied. A commonly used technique is ‘[[Taping|McConnell taping]] or kinesiotaping. <ref name="derasari a.">Derasari A, Brindle TJ, Alter KE, Sheehan FT. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2836141/ McConnell taping shifts the patella inferiorly in patients with patellofemoral pain: a dynamic magnetic resonance imaging study]. Phys Ther. 2010 Mar;90(3):411-9. doi: 10.2522/ptj.20080365.</ref><ref name="naoko aminaka">Aminaka N, Gribble PA. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1323297/ A systematic review of the effects of therapeutic taping on patellofemoral pain syndrome]. J Athl Train. 2005 Oct-Dec;40(4):341-51. </ref> | |||
Supporting the patella and knee joint by bracing is a further way to reduce pain and symptoms, but it will also alter patella tracking and reduce the active function of the quadriceps. Bracing may be useful in the short term to offer patients some support and pain relief to help them avoid antalgic movements and normalise gait as much as possible. Bracing can also be used for patients pre- and postoperatively, but a brace should allow variation in medial pull on the patellar and pressure.<ref name="Manske" /> Wearing a patellar realignment brace and following physical therapy has a synergistic effect on patients with chondromalacia patellae.<ref name=":3" /> | |||
=== Foot Orthoses === | |||
Foot orthoses are another option for pain relief, but only in cases where lower limb mechanics are deemed to be contributing to the knee pain, which may be due to: | |||
* Poor pronation control, | |||
* Excessive lower limb internal rotation during weight-bearing | |||
* An increased Q-angle.<ref name="Bill Vicenzino" /> <ref name="Manske" /> | |||
< | === Foam Roller === | ||
Using a foam roller cab be useful for relieving tight musculature and reducing pressure over the patella.<ref name=":8">Macdonald GZ, Button DC, Drinkwater EJ, Behm DG. [https://journals.lww.com/acsm-msse/fulltext/2014/01000/foam_rolling_as_a_recovery_tool_after_an_intense.19.aspx Foam rolling as a recovery tool after an intense bout of physical activity]. Med Sci Sports Exerc. 2014 Jan;46(1):131-42. doi: 10.1249/MSS.0b013e3182a123db. </ref> | |||
== References == | == References == | ||
<references /> | |||
<br> | |||
[[Category:Vrije_Universiteit_Brussel_Project]] | |||
[[Category:Knee]] [[Category: | [[Category:Knee]] | ||
[[Category:Conditions]] | |||
[[Category:Knee - Conditions]] | |||
[[Category:Musculoskeletal/Orthopaedics]] | |||
[[Category:Sports Medicine]] | |||
Latest revision as of 16:16, 25 March 2024
Top Contributors - Francky Petit, Gianni Delmoitie, Scott Cornish, Admin, Kim Jackson, Ine Van de Weghe, Uchechukwu Chukwuemeka, Scott Buxton, George Prudden, Robbe Luyckx, Sem Bras, Tessa Fransis, 127.0.0.1, Nupur Smit Shah, Evan Thomas, WikiSysop, Wanda van Niekerk and Naomi O'Reilly
Definition/Description[edit | edit source]
Chondromalacia patellae (CMP) is referred to as anterior knee pain due to the physical and biomechanical changes [1]. The articular cartilage of the posterior surface of the patella is going though degenerative changes [2] which manifest as a softening, swelling, fraying, and erosion of the hyaline cartilage underlying the patella and sclerosis of the underlying bone. [3]
Chondromalacia patellae is one of the most frequently encountered causes of anterior knee pain among young people. It’s the number one cause in the United States with an incidence as high as one in four people.[4] The word chondromalacia is derived from the Greek words - chrondros, meaning cartilage, and malakia, meaning softening. Hence chondromalacia patellae is a softening of the articular cartilage on the posterior surface of the patella which may eventually lead to fibrillation, fissuring, and erosion.[5]
The differential diagnosis of chondromalacia includes patellofemoral pain syndrome and patellar tendinopathy. Chondromalacia patella is not considered to be under the umbrella term of PFPS.[6][7][8] The pathophysiology is different and therefore there is an alternative treatment.[6][8]Chondromalacia patella can be present in patellofemoral pain but not everyone with patellofemoral pain syndrome will have chondromalacia patella.[9]
Clinically Relevant Anatomy[edit | edit source]
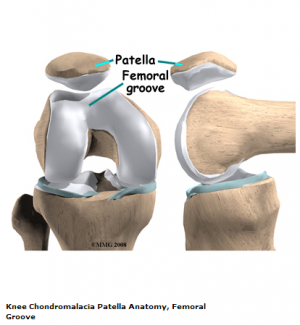
The knee comprises 4 major bones: the femur, tibia, fibula and the patella. The patella articulates with the femur at the trochlear groove. [10] Articular cartilage on the underside of the patella allows the patella to glide over the femoral groove, necessary for efficient motion at the knee joint. [11] Excess and persistent turning forces on the lateral side of the knee can harm the nutrition of the articular cartilage and more specifically in the medial and central area of the patella, where degenerative change will occur more readily. [12]
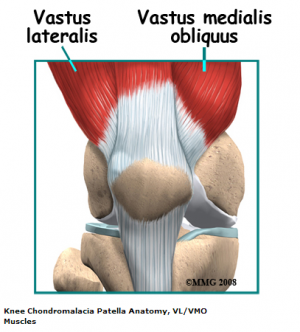
The quadriceps insert into the patella via the quadriceps tendon and are divided into four separate muscles: rectus femoris (RF), vastus lateralis (VL), vastus intermedius (VI) and vastus medialis (VM). The VM has oblique fibres which are referred to as the vastus medialis obliques (VMO)[13]
These muscles are active stabilisers during knee extension, especially the VL (on the lateral side) and the VMO (on the medial side). The VMO is active during knee extension but does not extend the knee. Its function is to keep the patella centred in the trochlea. This muscle is the only active stabiliser on the medial aspect, so its functional timing and amount of activity are critical to patellofemoral movement, the smallest change having significant effects on the position of the patella.
Not only do the quadriceps influence the patella position, but also the passive structures of the knee. These passive structures are more extensive and stronger on the lateral side than the medial side, with most of the lateral retinaculum arising from the iliotibial band (ITB). If the ITB is under excessive tension, excessive lateral tracking and/or lateral patellar tilt can occur. This is because the tensor fasciae lata is tight, as the ITB itself is a non-contractile structure.[12].
Other significant anatomical structures:
- Femoral anteversion [14] or medial torsion of the femur is a condition that changes the alignment of the bones at the knee. This may lead to overuse injuries of the knee due to malalignment of the femur to the patella and tibia. [15]
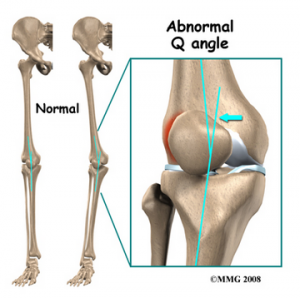
- The Q-angle: or quadriceps angle is the geometric relationship between the pelvis, the tibia, the patella and the femur[15][16] and is defined as the angle between the first line from the anterior superior iliac spine to the centre of the patella and the second line from the centre of the patella to the tibial tuberosity [17].
If there is increased adduction and/or internal rotation of the hip, the Q-angle will increase, which increases the relative valgus of the lower extremity. This higher Q-angle and valgus will increase the contact pressure on the lateral side of the patellofemoral joint (which is also increased by external rotation of the tibia) [18]
Epidemiology /Etiology[edit | edit source]
The aetiology of CMP is poorly understood, although it is believed that the causes of chondromalacia are injury, generalised constitutional disturbance and patellofemoral contact [19], or as a result of trauma to the chondrocytes in the articular cartilage (leading to proteolytic enzymatic digestion of the superficial matrix). It may also be caused by instability or maltracking of the patella which softens the articular cartilage. [20] Chondromalacia patella is usually described as an overload injury, caused by malalignment of the femur to the patella and the tibia. [21]
Main reasons for patellar malalignment;
- Q-angle: An abnormality of the Q-angle is one of the most significant factors of patellar malalignment. A normal Q-angle is 14° for men and 17° for women. An increase can result in an increased lateral pull on the patella.
- Muscular tightness of:
- Rectus femoris: affects patellar movement during flexion of the knee.
- Tensa Fascia late; affects the influence of the ITB
- Hamstrings: during running, tight hamstrings increase knee flexion resulting to increased ankle dorsiflexion. This causes compensatory pronation in the talocrural joint.
- Gastrocnemius: tightness will result in compensatory pronation in the subtalar joint.
- Excessive pronation: prolonged pronation of the subtalar joint is caused by internal rotation of the leg. This internal rotation will result in malalignment of the patella.
- Patella alta: this is a condition where the patella is positioned in an abnormally superior position. It is present when the length of the patellar tendon is 20% greater than the height of the patella.
- Vastus medialis insufficiency: the function of the vastus medialis is to realign the patella during knee extension. If the strength of VM is insufficient this will cause a lateral drift of the patella.[22]
A muscular balance between the VL and VM is important. Where VM is weaker the patella is pulled too far laterally which can cause increased contact with the condylus lateralis, leading to degenerative disease.[23]
Degenerative changes of the articular cartilage can be caused by [24]:
- Trauma: instability caused by previous trauma or overuse during recovery
- Repetitive microtrauma and inflammatory conditions
- Postural distortion: causes malposition or dislocation of the patella in the trochlear groove
Hip positioning and strength are linked to the prevalence of patellofemoral pain syndrome. Therefore, hip strengthening and stability exercises may be useful in the treatment program of patellofemoral pain syndrome.[18]
Some authors use the term “patellar pain syndrome” instead of “chondromalacia” to describe “anterior knee pain”. [25]
Stages of the Disease[edit | edit source]
In the early stages, chondromalacia shows areas of high sensitivity to fluid sequences. This can be associated with the increased thickness of the cartilage and may also cause oedema. In the latter stages, there will be a more irregular surface with focal thinning that can expand to and expose the subchondral bone. [26]
Chondromalacia patella is graded based on arthroscopic findings, the depth of cartilage thinning and associated subchondral bone changes. Moderate to severe stages can be seen on MRI. [27]
- Stage 1: softening and swelling of the articular cartilage due to broken vertical collagenous fibres. The cartilage is spongy on arthroscopy.
- Stage 2: blister formation in the articular cartilage due to the separation of the superficial from the deep cartilaginous layers. Cartilaginous fissures affecting less than 1,3 cm² in area with no extension to the subchondral bone.
- Stage 3: fissures ulceration, fragmentation, and fibrillation of cartilage extending to the subchondral bone but affecting less than 50% of the patellar articular surface.
- Stage 4: crater formation and eburnation of the exposed subchondral bone more than 50% of the patellar articular surface exposed, with sclerosis and erosions of the subchondral bone. Osteophyte formation also occurs at this stage.
Articular cartilage does not have any nerve endings, so CMP should not be considered as a true source of anterior knee pain, rather, it is a pathological or surgical finding that represents areas of articular cartilage trauma or divergent loading. [11] Kok et al showed that there is a significant association between subcutaneous knee fat thickness with the presence and severity of chondromalacia patellae. This could explain why women suffer more from the condition of chondromalacia than men.[28]
Characteristics/Clinical Presentation[edit | edit source]
There are important distinguishing features between chondromalacia patellae and Osteoarthritis. CMP affects just one side of the joint, the convex patellar side, [29] with excised patellas show localised softening and degeneration of the articular cartilage. [30] The main symptom of chondromalacia patellae is anterior knee pain,[19] which is exacerbated by common daily activities that load the patellofemoral joint, such as running, stair climbing, squatting, kneeling [1], or changing from a sitting to a standing position [31]. The pain often causes disability affecting the short-term participation of daily and physical activities.[32] Other symptoms are tenderness on palpating under the medial or lateral border of the patella, [33] crepitation (felt with motion), [34]; minor swelling, [33] a weak vastus medialis muscle and a high Q-angle. [35] Vastus medialis is functionally divided into two components: the vastus medialis longus (VML) and the vastus medialis obliquus (VMO). The VML extends the knee, with the rest of the quadriceps muscle. The VMO does not extend the knee but is active throughout the knee extension. This component assists in keeping the patella centred in the femoral trochlea. [12]
This condition can cause a deficit in quadriceps strength, therefore, building and/or maintaining quadriceps strength is essential.[1] A significant number of individuals are asymptomatic, but crepitation in flexion or extension is often present. [36]Chondromalacia is common in adolescents and females with idiopathic chondromalacia usually seen in young children and adolescents and the degenerative condition is most common in the middle-aged and older population. [26]
Differential Diagnosis[edit | edit source]
- Patellar subluxation
- Osteoarthritis
- Rheumatoid arthritis
- Anterior knee pain
- Patellofemoral pain syndrome
Diagnostic Procedures[edit | edit source]
Since its first description by Budinger in 1906, chondromalacia patella has been of significant clinical interest because diagnosis is often difficult. The chief reason for this is that the aetiology is often unknown and the correlation between the articular cartilage changes and the clinical system is poor. Patients affected by chondromalacia patella are young, between 15 and 35 years old, and many are highly active and are often considerably disabled by the symptoms of aching behind the patella, recurrent effusion of the knee, knee instability and crepitus.[37]
The primary diagnostic approach for chondromalacia patellae is radiography with added arthrography. Pinhole scintigraphy, part of arthrography, is also used to diagnose the condition. [38] MRI is an effective, non-invasive method with the ability to increase the sensitivity and specificity of the diagnosis.[39]
Outcome Measures[edit | edit source]
There are various measures: [40][41]
- Anterior Knee Pain Scale: a 13-item questionnaire with categories related to various levels of current knee function.
- Visual analog scale
- The five KOOS subscales: a scale about patients' experience over time with knee conditions. It consists of five subscales: Pain, other Symptoms, Function in daily living, Function in sport and recreation and knee-related Quality of life.
Examination[edit | edit source]
Examination of the knee is 4 fold: observation, mobility, feel, X-ray.[5]
- Observation: joint appearance is usually normal, but there may be a slight effusion.
- Mobility: passive movements are usually full and painless, but repeated extension of the knee from flexion will produce pain and a grating feeling underneath the patella, especially if the articular surfaces are compressed together.
- Feel: Pain and crepitus will be felt if the patella is compressed against the femur, either vertically or horizontally, with the knee in full extension. By displacing the patella medially or laterally, the patellar margins and their articular surfaces may be felt. Tenderness of one or other margin may be elicited and more frequently felt medially. Resisting a static quadriceps contraction will generally produce a sharp pain under the patella. This may be apparent in both knees, but more severe on the affected side.
- X-ray: an AP view of the patellofemoral joint is needed to detect any radiological change. In all but the most advanced cases, there is no convincing radiological change. In the latter stages, patellofemoral joint space narrows and osteoarthritic changes begin to appear.
Tests[edit | edit source]
The patient's posture can be an initial clue as well as any observed asymmetries, such as; limb alignment in standing, internal femoral rotation, anterior or posterior pelvic tilt, hyperextended or ‘locked back’ knees, genu varum or valgum and abnormal pronation of the foot. Gait patterns may also be affected. [13]
Mobility and range of motion (ROM) of the joint are tested, which can be limited. if bursitis is present, passive flexion or active extension will be painful. Loss of power in the affected leg may also be present on isometric testing. There are specific tests for anterior knee pain syndrome: [34]
- Patellar grind test or Clarke’s sign: This test detects the presence of patellofemoral joint disorder. A positive sign on this test is a pain in the patellofemoral joint.
- Compression test
- Extension-resistance test: This test is used to perform a maximal provocation on the muscle-tendon mechanism of the extensor muscles and is positive when the affected knee demonstrates less power when trying to maintain the pressure.
- The critical test: This is done with the patient in high sitting and performing isometric quadriceps contractions at 5 different angles (0°, 30°, 60°, 90° and 120°) while the femur is externally rotated, sustaining the contractions for 10 seconds. If pain is produced then the leg is positioned in full extension. In this position, the patella and femur have no more contact. The lower leg of the patient is supported by the therapist so the quadriceps can be fully relaxed. When the quadriceps is relaxed, the therapist can glide the patella medially. This glide is maintained while the isometric contractions are again performed. If this reduces the pain and the pain is patellofemoral in origin, there is a high chance of a favourable outcome.[4]
It is possible to diagnose incorrectly and these tests may aid in determining chondromalacia, but other possible conditions also need to be excluded.
Medical Management[edit | edit source]
Exercise and education are two important aspects of a treatment programme. Education helps the patient to understand the condition and how they should deal with it for optimal recovery. Exercise focus is on stretching and strengthening appropriate structures, such as the hamstring, quadriceps and gastrocnemius length and strength of the gluteal muscles.[42] Fire needling and acupuncture may also relieve clinical symptoms of chondromalacia patellae and recover the biodynamical structure of the patellae. [43]
If conservative measures fail, there are several possible surgical procedures. [27]
- Chondrectomy: also known as shaving. This treatment includes shaving down the damaged cartilage to the non-damaged cartilage underneath. The success of this treatment depends on the severity of the cartilage damage.
- Drilling is also a method that is frequently used to heal damaged cartilage. However, this procedure has not so far been proven to be effective. More localised degeneration might respond better to drilling small holes through the damaged cartilage. This facilitates the growth of healthy tissue through the holes from the layers underneath.
- Full patellectomy: This is the most severe surgical treatment. This method is only used when no other procedures are helpful, but a significant consequence is that the quadriceps will become weak.
Two other treatments that may be successful: [24]
- Replacement of the damaged cartilage: The damaged cartilage is replaced by a polyethylene cap prosthesis. Early results have been good, but the eventual wearing of the opposing articular surface is inevitable.
- Autologous chondrocyte transplantation under a tibial periosteal patch. [24]
Simply removing the cartilage is not a cure for chondromalacia patellae. The biomechanical deficits need addressing and there are various procedures to aid in managing this.
- Tightening of the medial capsule (MC): If the MC is lax, it can be tightened by pulling the patella back into its correct alignment.
- Lateral release: A very tight lateral capsule will pull the patella laterally. Release of the lateral patellar retinaculum allows the patella to track correctly into the femoral groove.
- Medial shift of the tibial tubercle: Moving the insertion of the quadriceps tendon medially at the tibial tubercle, allows the quadriceps to pull the patella more directly. It also decreases the amount of wear on the underside of the patellar.
- Partial removal of the patella
Although there is no overall agreement for the treatment of chondromalacia, the consensus is that the best treatment is a non-surgical one.[44]
Physical Therapy Management[edit | edit source]
Exercise Program[edit | edit source]
Conservative treatment of chondromalacia patellae is both physical and highly advised. Short-wave diathermy can help to relieve pain and to increase the blood supply to the area, improving the nutrition supply to the articular cartilage. Care must be taken when planning an exercise programme.[42] Conservative therapeutic interventions include the following:[45]
- Isometric quadriceps strengthening and stretching exercises[1] Restoration of adequate quadriceps strength and function is an essential factor in achieving good recovery. The most effective exercises are isometric and isotonic in the inner range. Isotonic exercises through a full range of motion will only lead to increased pain and even joint effusion.[42] Stretching of the vastus lateralis and strengthening of the vastus medialis is often recommended, but they are difficult to isolate due to shared innervation and insertion.[13][23]It has shown that closed kinematic chain exercises can improve patellofemoral joint performance by increasing quadriceps muscle strength and patellar alignment correction.[46]
- Hamstring stretching exercises
- Temporary modification of activity
- Patellar taping
- Foot orthoses
- NSAIDs
- Hip strength and stability training, as hip positioning and strength have a significant influence on anterior knee pain.
- Hip abductor strengthening as an increased hip adduction angle is associated with weakened hip abductors.[47]
- Patellar realignment brace[41]
Not only is strengthening important, but stretching should also be part of the programme. [11] It has been shown that patients with patellofemoral pain syndrome have shorter and less flexible hamstrings than asymptomatic individuals.. Although stretching can improve flexibility and knee function, it doesn’t necessarily directly improve pain.[48]
Another form of therapy is warm needling. In combination with rehabilitation exercises, it has a prolonged pain-relieving effect than in warm needling in combination with medication[49]
Ice Medication[edit | edit source]
Ice may be useful for reducing pain in an acute flare-up, but not as a long-term treatment protocol.[47] NSAIDs may also be of benefit in the short term to relieve pain so that knee function and mobility are normalised and an exercise programme can begin.
Taping and Braces[edit | edit source]
Taping the patella to influence its movement may provide some short-term relief, but the evidence is varied. A commonly used technique is ‘McConnell taping or kinesiotaping. [50][51]
Supporting the patella and knee joint by bracing is a further way to reduce pain and symptoms, but it will also alter patella tracking and reduce the active function of the quadriceps. Bracing may be useful in the short term to offer patients some support and pain relief to help them avoid antalgic movements and normalise gait as much as possible. Bracing can also be used for patients pre- and postoperatively, but a brace should allow variation in medial pull on the patellar and pressure.[25] Wearing a patellar realignment brace and following physical therapy has a synergistic effect on patients with chondromalacia patellae.[41]
Foot Orthoses[edit | edit source]
Foot orthoses are another option for pain relief, but only in cases where lower limb mechanics are deemed to be contributing to the knee pain, which may be due to:
- Poor pronation control,
- Excessive lower limb internal rotation during weight-bearing
- An increased Q-angle.[32] [25]
Foam Roller[edit | edit source]
Using a foam roller cab be useful for relieving tight musculature and reducing pressure over the patella.[45]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Herrington L, Al-Sherhi A. A controlled trial of weight-bearing versus non-weight-bearing exercises for patellofemoral pain. J Orthop Sports Phys Ther. 2007 Apr;37(4):155-60. doi: 10.2519/jospt.2007.2433.
- ↑ http://www.e-radiography.net/radpath/c/chondromalaciap.htm
- ↑ Gagliardi JA, Chung EM, Chandnani VP, Kesling KL, Christensen KP, Null RN, et al. Detection and staging of chondromalacia patellae: relative efficacies of conventional MR imaging, MR arthrography, and CT arthrography. AJR Am J Roentgenol. 1994 Sep;163(3):629-36. doi: 10.2214/ajr.163.3.8079858.
- ↑ 4.0 4.1 Laprade J, Culham E, Brouwer B. Comparison of five isometric exercises in the recruitment of the vastus medialis oblique in persons with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 1998; 27: 197–204
- ↑ 5.0 5.1 Gordon HM. Chondromalacia patellae. Aust J Physiother. 1977 Sep;23(3):103-6. doi: 10.1016/S0004-9514(14)61028-X.
- ↑ 6.0 6.1 Wiles P, Andrews PS, Devas MB. Chondromalacia of the patella. Bone & Joint Journal. 1956 Feb 1;38(1):95-113.
- ↑ Blazer K. Diagnosis and treatment of patellofemoral pain syndrome in the female adolescent. Physician Assistant. 2003 Sep 1;27(9):23-30.
- ↑ 8.0 8.1 Fernández-Cuadros ME, Albaladejo-Florín MJ, Algarra-López R, Pérez-Moro OS. Efficiency of Platelet-rich Plasma (PRP) Compared to Ozone Infiltrations on Patellofemoral Pain Syndrome and Chondromalacia: A Non-Randomized Parallel Controlled Trial. Diversity & Equality in Health and Care. 2017 Aug 4;14(4):203-211
- ↑ Willy RW, Hoglund LT, Barton CJ, Bolgla LA, Scalzitti DA, Logerstedt DS, Lynch AD, Snyder-Mackler L, McDonough CM. Patellofemoral Pain. J Orthop Sports Phys Ther. 2019 Sep;49(9):CPG1-CPG95. doi: 10.2519/jospt.2019.0302.
- ↑ http://emedicine.medscape.com/article/1898986-overview#aw2aab6b3 fckLR
- ↑ 11.0 11.1 11.2 Anderson MK. Fundamentals of Sports Injury Management, second edition, Lippincott Williams & Wilkins, 2003, p. 208
- ↑ 12.0 12.1 12.2 Beeton KS. Manual Therapy Masterclasses: The Peripheral Joints, Churchill Livingstone, 2003, p.50-51
- ↑ 13.0 13.1 13.2 Kendall FP, Hulsman P, Zuidgeest A. Spieren: tests en functies, Nederland:Bohn Stafleu van Loghum, 469p (383)
- ↑ Nyland J, Kuzemchek S, Parks M, Caborn DN. Femoral anteversion influences vastus medialis and gluteus medius EMG amplitude: composite hip abductor EMG amplitude ratios during isometric combined hip abduction-external rotation. J Electromyogr Kinesiol. 2004 Apr;14(2):255-61. doi: 10.1016/S1050-6411(03)00078-6.
- ↑ 15.0 15.1 Milner CE. Functional Anatomy For Sport And Exercise: Quick Reference, Routledge, 2008, p58-60
- ↑ Singh V. Clinical And Surgical Anatomy, second edition, Elsevier, 2007, p228- 230.
- ↑ Asseln M, Eschweiler J, Zimmermann F, Radermacher K. The Q-Angle and its Effect on Active Knee Joint Kinematics - a Simulation Study. Biomed Tech (Berl). 2013 Aug;58 Suppl 1:/j/bmte.2013.58.issue-s1-D/bmt-2013-4115/bmt-2013-4115.xml. doi: 10.1515/bmt-2013-4115.
- ↑ 18.0 18.1 Meira EP, Brumitt J. Influence of the hip on patients with patellofemoral pain syndrome: a systematic review. Sports Health. 2011 Sep;3(5):455-65. doi: 10.1177/1941738111415006.
- ↑ 19.0 19.1 Salehi I, Khazaeli S, Hatami P, Malekpour M. Bone density in patients with chondromalacia patella. Rheumatol Int. 2010 Jun;30(8):1137-8. doi: 10.1007/s00296-009-1149-3.
- ↑ Macmull S, Jaiswal PK, Bentley G, Skinner JA, Carrington RW, Briggs TW. The role of autologous chondrocyte implantation in the treatment of symptomatic chondromalacia patellae. Int Orthop. 2012 Jul;36(7):1371-7. doi: 10.1007/s00264-011-1465-6.
- ↑ Bartlett R. Encyclopedia of International Sports Studies, Routledge, 2010, p90.
- ↑ McConnell J. The management of chondromalacia patellae: a long term solution. Australian Journal of Physiotherapy; 1986, 32(4): 215-223
- ↑ 23.0 23.1 http://www.aafp.org/afp/991101ap/2012.htm
- ↑ 24.0 24.1 24.2 Logan AL. The Knee Clinical Applications. Aspen Publishers, 1994, p131.
- ↑ 25.0 25.1 25.2 Manske RC. Postsurgical Orthopedic Sports Rehabilitation: Knee & Shoulder, 2006, Mosby:Elsevier, p446-451.
- ↑ 26.0 26.1 Wessely M, Young M. Essential Musculoskeletal MRI: A Primer for the Clinician. Churchill Livingstone Elsevier, 2011, p115.
- ↑ 27.0 27.1 Munk PL, Ryan AG. Teaching Atlas of Musculoskeletal Imaging. Thieme, 2008, p68-70.
- ↑ Kok HK, Donnellan J, Ryan D, Torreggiani WC. Correlation between subcutaneous knee fat thickness and chondromalacia patellae on magnetic resonance imaging of the knee. Can Assoc Radiol J. 2013 Aug;64(3):182-6. doi: 10.1016/j.carj.2012.04.003.
- ↑ Ellis H, French H, Kinirons MT. French’s Index of differential diagnosis. 14th edition, Hodder Arnold Publishers, 2005.
- ↑ Anderson JR. Muir’s Textbook of Pathology. 12th edition, Lippincott Williams Wilkins, 1988
- ↑ Moeckel E, Noori M. Textbook of Pediatric Osteopathy. Elsevier Health Sciences, 2008, p338.
- ↑ 32.0 32.1 Vicenzino B, Collins N, Crossley K, Beller E, Darnell R, McPoil T. Foot orthoses and physiotherapy in the treatment of patellofemoral pain syndrome: a randomised clinical trial. BMC Musculoskelet Disord. 2008 Feb 27;9:27. doi: 10.1186/1471-2474-9-27. PMID: 18304317; PMCID: PMC2279129.
- ↑ 33.0 33.1 Shultz SJ, Houglum PA, Perrin DH. Examination of Musculoskeletal injuries. 3rd edition. Human Kinetics, 2010, p453.
- ↑ 34.0 34.1 DeGowin RL, DeGowin EL. DeGowin & DeGowin’s Diagnostic Examination. 6th edition. McGraw Hill, 1994, p735.
- ↑ Ebnezar J, Textbook of Orthopedics. 4th edition. India:JP Medical Ltd, 2010, p426-427.
- ↑ Murray RO, Jacobson HG. The Radiology of Skeletal Disorders: exercises in diagnosis. 2nd edition. Churchill Livingstone, 1990, p306-307.
- ↑ Bentley G, Lesly IJ, Fischer D. Effect of aspirin treatment on chondromalacia patella. Annals of the rheumatic diseases, 1981; 40:37-41.
- ↑ Bahk YW, Park YH, Chung SK, Kim SH, Shinn KS. Pinhole scintigraphic sign of chondromalacia patellae in older subjects: a prospective assessment with differential diagnosis. J Nucl Med. 1994;35:855–862.
- ↑ Kim HJ, Lee SH, Kang CH, Ryu JA, Shin MJ, Cho KJ, et al. Evaluation of the chondromalacia patella using a microscopy coil: comparison of the two-dimensional fast spin echo techniques and the three-dimensional fast field echo techniques. Korean J Radiol. 2011 Jan-Feb;12(1):78-88. doi: 10.3348/kjr.2011.12.1.78.
- ↑ Crossley KM, Bennell KL, Cowan SM, Green S. Analysis of outcome measures for persons with patellofemoral pain: which are reliable and valid? Arch Phys Med Rehabil. 2004 May;85(5):815-22. doi: 10.1016/s0003-9993(03)00613-0.
- ↑ 41.0 41.1 41.2 Petersen W, Ellermann A, Rembitzki IV, Scheffler S, Herbort M, Brüggemann GP, et al. Evaluating the potential synergistic benefit of a realignment brace on patients receiving exercise therapy for patellofemoral pain syndrome: a randomized clinical trial. Arch Orthop Trauma Surg. 2016 Jul;136(7):975-82. doi: 10.1007/s00402-016-2464-2.
- ↑ 42.0 42.1 42.2 Clark DI, Downing N, Mitchell J, Coulson L, Syzpryt EP, Doherty M. Physiotherapy for anterior knee pain: a randomised controlled trial. Ann Rheum Dis. 2000 Sep;59(9):700-4. doi: 10.1136/ard.59.9.700.
- ↑ Huang J, Li L, Lou BD, Tan CJ, Liu Z, Ye Y, et al. [Efficacy observation on chrondromalacia patellae treated with fire needling technique at high stress points]. Zhongguo Zhen Jiu. 2014 Jun;34(6):551-4.
- ↑ van Linschoten R, van Middelkoop M, Berger MY, Heintjes EM, Verhaar JA, Willemsen SP, et al. Supervised exercise therapy versus usual care for patellofemoral pain syndrome: an open-label randomised controlled trial. BMJ. 2009 Oct 20;339:b4074. doi: 10.1136/bmj.b4074.
- ↑ 45.0 45.1 Macdonald GZ, Button DC, Drinkwater EJ, Behm DG. Foam rolling as a recovery tool after an intense bout of physical activity. Med Sci Sports Exerc. 2014 Jan;46(1):131-42. doi: 10.1249/MSS.0b013e3182a123db.
- ↑ Bakhtiary AH, Fatemi E. Open versus closed kinetic chain exercises for patellar chondromalacia. Br J Sports Med. 2008 Feb;42(2):99-102; discussion 102. doi: 10.1136/bjsm.2007.038109.
- ↑ 47.0 47.1 Bleakley C, McDonough S, MacAuley D. The use of ice in the treatment of acute soft-tissue injury: a systematic review of randomized controlled trials. Am J Sports Med. 2004 Jan-Feb;32(1):251-61. doi: 10.1177/0363546503260757.
- ↑ Harvie D, O'Leary T, Kumar S. A systematic review of randomized controlled trials on exercise parameters in the treatment of patellofemoral pain: what works? J Multidiscip Healthc. 2011;4:383-92. doi: 10.2147/JMDH.S24595.
- ↑ Qiu L, Zhang M, Zhang J, Gao LN, Chen DW, Liu J, et al. Chondromalacia patellae treated by warming needle and rehabilitation training. J Tradit Chin Med. 2009 Jun;29(2):90-4. doi: 10.1016/s0254-6272(09)60039-x.
- ↑ Derasari A, Brindle TJ, Alter KE, Sheehan FT. McConnell taping shifts the patella inferiorly in patients with patellofemoral pain: a dynamic magnetic resonance imaging study. Phys Ther. 2010 Mar;90(3):411-9. doi: 10.2522/ptj.20080365.
- ↑ Aminaka N, Gribble PA. A systematic review of the effects of therapeutic taping on patellofemoral pain syndrome. J Athl Train. 2005 Oct-Dec;40(4):341-51.