Brachial Plexus: Difference between revisions
Kim Jackson (talk | contribs) m (Text replacement - "== '''" to "==") |
No edit summary |
||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- [[User:Matt Anderson|Matt Anderson]] | '''Original Editor '''- [[User:Matt Anderson|Matt Anderson]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
The Brachial Plexus is a network of nerve fibers that run from the spine, | The Brachial Plexus is a network of nerve fibers that run from the spine, passing through the cervico-axillary canal to reach axilla. It is formed by the ventral rami of the lower four cervical and first thoracic nerve roots (C5-C8, T1).<ref name="Teach">TeachMeAnatomy. TeachMeSeries, Educational Health Care Resource. http://teachmeanatomy.info/upper-limb/nerves/brachial-plexus/. (accessed 9 Apr 2017).</ref> | ||
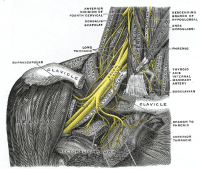
[[Image:Brachial-Plexus.png|thumb|left|200px|The right brachial plexus with its short branches, viewed from in front.]][[Image:Brachial plexus anterior view nerves.JPG|thumb|center]] | |||
[[Image:Brachial-Plexus.png|thumb|left|200px|The right brachial plexus with its short branches, viewed from in front.]][[Image:Brachial plexus anterior view nerves.JPG|thumb|center]] | |||
== Function == | == Function == | ||
The brachial plexus is responsible for cutaneous and muscular innervation of the entire upper limb, with two exceptions: the [[Trapezius|trapezius muscle]] innervated by the spinal accessory nerve (CN XI) and an area of skin near the axilla innervated by the intercostobrachial nerve.<ref name="Stanley">Hoppenfeld S. Physical Examination of the Spine and Extremities. CTI Reviews 2014.</ref> | The brachial plexus is responsible for cutaneous and muscular innervation of the entire upper limb, with two exceptions: the [[Trapezius|trapezius muscle]] innervated by the spinal accessory nerve (CN XI) and an area of skin near the axilla innervated by the intercostobrachial nerve.<ref name="Stanley">Hoppenfeld S. Physical Examination of the Spine and Extremities. CTI Reviews 2014.</ref> | ||
== Description == | == Description == | ||
=== Path | === Path<ref name="Dutton">Dutton M. Orthopaedic Examination, Evaluation and Intervention. 2nd Ed. New York: McGraw-Hill, 2008.</ref><ref name="Slide">SlideShare, LinkedIn Corporation. Brachial Plexus:Anatomy and localisation of lesion. www.slideshare.net/anjupaed/brachial-plexus (accessed 9 Apr 2017)</ref> === | ||
The brachial plexus is divided into Roots, Trunks, Divisions, Cords, and Branches. There are five "terminal" branches and numerous other "pre-terminal" or "collateral" branches that leave the plexus at various points along its length. | The brachial plexus is divided into Roots, Trunks, Divisions, Cords, and Branches. There are five "terminal" branches and numerous other "pre-terminal" or "collateral" branches that leave the plexus at various points along its length. | ||
*The five '''Roots''' are the five anterior rami | *The five '''Roots''' are the five anterior rami of the lower four cervical and first thoracic nerve roots (C5-C8, T1) after they have given off their segmental supply to the muscles of the neck. These Roots merge to form three Trunks: | ||
**Upper Trunk (C5-C6) | **Upper Trunk (C5-C6) | ||
**Middle Trunk (C7) | **Middle Trunk (C7) | ||
**Lower Trunk (C8, T1) | **Lower Trunk (C8, T1) | ||
*Each '''Trunk''' then splits into anterior and posterior divisions, to form six Divisions. | *Each '''Trunk''' then splits into anterior and posterior divisions, to form six Divisions. The anterior/ posterior divisions innervate flexor groups versus extensor groups: | ||
**anterior divisions of the upper, middle, and lower trunks | **anterior divisions of the upper, middle, and lower trunks | ||
**posterior divisions of the upper, middle, and lower trunks | **posterior divisions of the upper, middle, and lower trunks | ||
*These six '''Divisions '''will regroup to become the three Cords. The Cords are named by their position | *These six '''Divisions '''will regroup to become the three Cords. The Cords are named by their position to the axillary artery. | ||
**The Posterior Cord is formed from the three posterior divisions of the trunks (C5-C8,T1) | **The Posterior Cord is formed from the three posterior divisions of the trunks (C5-C8, T1) | ||
**The Lateral Cord is the anterior divisions from the upper and middle trunks (C5-C7) | **The Lateral Cord is the anterior divisions from the upper and middle trunks (C5-C7) | ||
**The Medial Cord is simply a continuation of the anterior division of the lower trunk (C8,T1) | **The Medial Cord is simply a continuation of the anterior division of the lower trunk (C8, T1) | ||
[[Image:Brachial-plexus-2.png|thumb|center|600px|Anatomical illustration of the brachial plexus with areas of roots, trunks, divisions and cords marked.]] | [[Image:Brachial-plexus-2.png|thumb|center|600px|Anatomical illustration of the brachial plexus with areas of roots, trunks, divisions, and cords marked.]] | ||
=== Specific Branches | === Specific Branches<ref name="Teach" /><ref name="Dutton" /><span style="background-color: initial; font-size: 17.5296px;"></span> === | ||
The branches are listed below. | The branches are listed below. They mostly branch from the cords, but some originate from earlier structures (indicated in italics). | ||
'''Bold''' indicates primary spinal root component of nerve. ''Italics'' indicate spinal roots that frequently, but not always, contribute to the nerve. | '''Bold''' indicates primary spinal root component of the nerve. ''Italics'' indicate spinal roots that frequently, but not always, contribute to the nerve. | ||
{| width="100%" border="1" cellpadding="1" cellspacing="1" align="center" | {| width="100%" border="1" cellpadding="1" cellspacing="1" align="center" | ||
|- | |- | ||
| From | | From | ||
| Nerve | | Nerve | ||
| Roots | | Roots | ||
| Muscles | | Muscles | ||
| Cutaneous | | Cutaneous | ||
|- style="background:#ffcccc" | |- style="background:#ffcccc" | ||
| roots | | roots | ||
| Dorsal scapular nerve | | Dorsal scapular nerve | ||
| ''C4'', '''C5''' | | ''C4'', '''C5''' | ||
| [[Rhomboids|Rhomboid muscles]] and [[Levator Scapulae|Levator scapulae]] | | [[Rhomboids|Rhomboid muscles]] and [[Levator Scapulae|Levator scapulae]] | ||
| - | | - | ||
|- style="background:#ffcccc" | |- style="background:#ffcccc" | ||
| roots | | roots | ||
| Long thoracic nerve | | Long thoracic nerve | ||
| '''C5''', '''C6''', C7 | | '''C5''', '''C6''', C7 | ||
| [[Serratus Anterior|Serratus anterior]] | | [[Serratus Anterior|Serratus anterior]] | ||
| - | | - | ||
|- style="background:#ccffcc" | |- style="background:#ccffcc" | ||
| upper trunk | | upper trunk | ||
| Nerve to the subclavius | | Nerve to the subclavius | ||
| ''C5'', '''C6''' | | ''C5'', '''C6''' | ||
| Subclavius muscle | | Subclavius muscle | ||
| - | | - | ||
|- style="background:#ccffcc" | |- style="background:#ccffcc" | ||
| upper trunk | | upper trunk | ||
| Suprascapular nerve | | Suprascapular nerve | ||
| '''C5''', C6 | | '''C5''', C6 | ||
| [[Supraspinatus]] and [[Infraspinatus]] | | [[Supraspinatus]] and [[Infraspinatus]] | ||
| - | | - | ||
|- style="background:#aaccff" | |- style="background:#aaccff" | ||
| lateral cord | | lateral cord | ||
| Lateral pectoral nerve | | Lateral pectoral nerve | ||
| C5, '''C6''', C7 | | C5, '''C6''', C7 | ||
| [[Pectoralis major]] and [[Pectoralis Minor|Pectoralis minor]] (by communicating with the Medial pectoral nerve) | | [[Pectoralis major]] and [[Pectoralis Minor|Pectoralis minor]] (by communicating with the Medial pectoral nerve) | ||
| - | | - | ||
|- style="background:#aaccff" | |- style="background:#aaccff" | ||
| lateral cord | | lateral cord | ||
| Musculocutaneous nerve | | Musculocutaneous nerve | ||
| C5, C6, C7 | | C5, C6, C7 | ||
| [[Coracobrachialis Muscle|Coracobrachialis]], [[Brachialis]] and [[Biceps brachii]] | | [[Coracobrachialis Muscle|Coracobrachialis]], [[Brachialis]] and [[Biceps brachii]] | ||
| becomes the Lateral cutaneous nerve of the forearm | | becomes the Lateral cutaneous nerve of the forearm | ||
|- style="background:#aaccff" | |- style="background:#aaccff" | ||
| lateral cord | | lateral cord | ||
| lateral root of the [[Median nerve]] | | lateral root of the [[Median nerve]] | ||
| C6, C7 | | C6, C7 | ||
| fibres to the median nerve | | fibres to the median nerve | ||
| - | | - | ||
|- style="background:#ffffcc" | |- style="background:#ffffcc" | ||
| posterior cord | | posterior cord | ||
| Upper subscapular nerve | | Upper subscapular nerve | ||
| C5, C6 | | C5, C6 | ||
| [[Subscapularis]] (upper part) | | [[Subscapularis]] (upper part) | ||
| - | | - | ||
|- style="background:#ffffcc" | |- style="background:#ffffcc" | ||
| posterior cord | | posterior cord | ||
| Thoracodorsal nerve (middle subscapular nerve) | | Thoracodorsal nerve (middle subscapular nerve) | ||
| C6, '''C7''', C8 | | C6, '''C7''', C8 | ||
| [[Latissimus Dorsi Muscle|Latissimus dorsi]] | | [[Latissimus Dorsi Muscle|Latissimus dorsi]] | ||
| - | | - | ||
|- style="background:#ffffcc" | |- style="background:#ffffcc" | ||
| posterior cord | | posterior cord | ||
| Lower subscapular nerve | | Lower subscapular nerve | ||
| C5, C6 | | C5, C6 | ||
| subscapularis (lower part ) and [[Teres Major|Teres major]] | | subscapularis (lower part ) and [[Teres Major|Teres major]] | ||
| - | | - | ||
|- style="background:#ffffcc" | |- style="background:#ffffcc" | ||
| posterior cord | | posterior cord | ||
| [[Axillary Nerve Injury|Axillary nerve]] | | [[Axillary Nerve Injury|Axillary nerve]] | ||
| '''C5''', C6 | | '''C5''', C6 | ||
| anterior branch: [[deltoid]] and a small area of overlying skin | | anterior branch: [[deltoid]] and a small area of overlying skin posterior branch: [[Teres Minor|Teres minor]] and deltoid muscles | ||
| posterior branch becomes Upper lateral cutaneous nerve of the arm | | posterior branch becomes Upper lateral cutaneous nerve of the arm | ||
|- style="background:#ffffcc" | |- style="background:#ffffcc" | ||
| posterior cord | | posterior cord | ||
| [[Radial nerve]] | | [[Radial nerve]] | ||
| C5, C6, C7, C8, T1 | | C5, C6, C7, C8, T1 | ||
| [[Triceps brachii|Triceps]] brachii, [[Supinator]], Anconeus, the [[Quadriceps Muscle Strain|extensor]] muscles of the Forearm, and [[Brachioradialis]] | | [[Triceps brachii|Triceps]] brachii, [[Supinator]], Anconeus, the [[Quadriceps Muscle Strain|extensor]] muscles of the Forearm, and [[Brachioradialis]] | ||
| skin of the posterior arm as the Posterior cutaneous nerve of the arm | | skin of the posterior arm as the Posterior cutaneous nerve of the arm | ||
|- style="background:#dddddd" | |- style="background:#dddddd" | ||
| medial cord | | medial cord | ||
| Medial pectoral nerve | | Medial pectoral nerve | ||
| C8, T1 | | C8, T1 | ||
| [[Pectoralis major]] and [[Pectoralis Minor|Pectoralis minor]] | | [[Pectoralis major]] and [[Pectoralis Minor|Pectoralis minor]] | ||
| - | | - | ||
|- style="background:#dddddd" | |- style="background:#dddddd" | ||
| medial cord | | medial cord | ||
| medial root of the [[Median nerve]] | | medial root of the [[Median nerve]] | ||
| C8, T1 | | C8, T1 | ||
| fibres to the median nerve | | fibres to the median nerve | ||
| portions of hand not served by ulnar or radial | | portions of hand not served by ulnar or radial | ||
|- style="background:#dddddd" | |- style="background:#dddddd" | ||
| medial cord | | medial cord | ||
| Medial cutaneous nerve of the arm | | Medial cutaneous nerve of the arm | ||
| C8, T1 | | C8, T1 | ||
| - | | - | ||
| front and medial skin of the Arm | | front and medial skin of the Arm | ||
|- style="background:#dddddd" | |- style="background:#dddddd" | ||
| medial cord | | medial cord | ||
| Medial cutaneous nerve of the forearm | | Medial cutaneous nerve of the forearm | ||
| C8, T1 | | C8, T1 | ||
| - | | - | ||
| medial skin of the forearm | | medial skin of the forearm | ||
|- style="background:#dddddd" | |- style="background:#dddddd" | ||
| medial cord | | medial cord | ||
| [[Ulnar Nerve|Ulnar nerve]] | | [[Ulnar Nerve|Ulnar nerve]] | ||
| C8, T1 | | C8, T1 | ||
| Flexor carpi ulnaris, the medial two bellies of Flexor digitorum profundus, the intrinsic hand muscles except the Thenar muscles and the two most lateral lumbricals | | Flexor carpi ulnaris, the medial two bellies of Flexor digitorum profundus, the intrinsic hand muscles except the Thenar muscles and the two most lateral lumbricals | ||
| the skin of the medial side of the hand and medial one and a half fingers on the palmar side and medial two and a half fingers on the dorsal side | | the skin of the medial side of the hand and medial one and a half fingers on the palmar side and medial two and a half fingers on the dorsal side | ||
|} | |} | ||
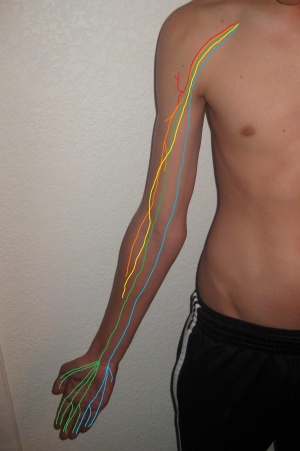
Specific branches can be visualised on the diagram below: | Specific branches can be visualised on the diagram below: | ||
[[Image:Brachplx.gif|center]] | [[Image:Brachplx.gif|center]] | ||
== Injuries == | == Injuries == | ||
Injury to the brachial plexus can be very problematic because the nerves branching off of the plexus provide innervation to the upper extremity. Clinical signs and symptoms vary with which area of the plexus is involved, and generally result in paralysis or anesthesia.<ref name="Dutton" /> | Injury to the brachial plexus can be very problematic because the nerves branching off of the plexus provide innervation to the upper extremity. Clinical signs and symptoms vary with which area of the plexus is involved, and generally result in paralysis or anesthesia.<ref name="Dutton" /> | ||
Symptoms can range from transient nerve dysfunction to complete upper extremity weakness. | Symptoms can range from transient nerve dysfunction to complete upper extremity weakness. Because of the anatomical variants<ref name="Orebaugh">Orebaugh SL, Williams BA. Brachial Plexus Anatomy: Normal and Variant. The Scientific World Journal. 2009;9:300-312.</ref> of the brachial plexus these injuries can be a challenge to diagnose. | ||
== Mechanism of Injury == | == Mechanism of Injury == | ||
The main causes of brachial plexus palsies are traction, due to extreme movements, and heavy impact. <ref name="Coene">Coene LN. Mechanisms of brachial plexus lesions. Clinical Neurology and Neurosurgery. 1993;95:24-29.</ref> | The main causes of brachial plexus palsies are traction, due to extreme movements, and heavy impact. <ref name="Coene">Coene LN. Mechanisms of brachial plexus lesions. Clinical Neurology and Neurosurgery. 1993;95:24-29.</ref> | ||
Brachial plexus injury can occur in a variety of ways and can occur as | Brachial plexus injury can occur in a variety of ways and can occur as a result of shoulder trauma, tumours, or inflammation. The rare [[Parsonage-Turner Syndrome|Parsonage-Turner Syndrome]]causes brachial plexus inflammation without obvious injury, but with nevertheless disabling symptoms. But in general, brachial plexus lesions can be classified as either traumatic or obstetric. | ||
*'''Obstetric injuries''' may occur from mechanical injury involving shoulder dystocia during difficult childbirth. | *'''Obstetric injuries''' may occur from a mechanical injury involving shoulder dystocia during a difficult childbirth. During birth, excessive stretching of the neck or pulling the upper extremity can result in an upper brachial plexus injury or inferior trunk, respectively. The incidence of brachial plexus injury is approximately 1 in 1,000 live births.<ref name="Benny">Joyner B, Soto MA, Henry M. Adam. Brachial Plexus Injury. Pediatrics in Review. 2006;27:238</ref> | ||
*'''Traumatic injury''' may arise from penetrating or sports related injuries, falls, work related injuries, radiation therapy and iatrogenic causes (i.e. first rib resection, shoulder surgery, brachial plexus block). | *'''Traumatic injury''' may arise from penetrating or sports-related injuries, falls, work-related injuries, radiation therapy and iatrogenic causes (i.e. first rib resection, shoulder surgery, brachial plexus block). However, the most common mechanism of injury is a traction injury due to the forceful separation of the neck from the shoulder. | ||
Common associated injuries can include fractures of the proximal humerus, clavicle, scapula, cervical spine and upper limb vascular injuries. <ref name="Coene" /> | Common associated injuries can include fractures of the proximal humerus, clavicle, scapula, cervical spine and upper limb vascular injuries. <ref name="Coene" />Management of these injuries may complicate the picture when diagnosing brachial plexus injury but can also guide in determining the mechanism of injury. | ||
{{#ev:youtube|JfsjQwCL0xU}} | {{#ev:youtube|JfsjQwCL0xU}} | ||
=== Classification of Injury === | === Classification of Injury === | ||
There are many classification systems for brachial plexus injuries, they can be divided into three types: | There are many classification systems for brachial plexus injuries, they can be divided into three types: | ||
#An '''upper brachial plexus lesion''', which occurs from excessive lateral neck flexion away from the shoulder. Most commonly, forceps delivery or falling on the neck at an angle causes upper plexus lesions leading to [[Erb's Palsy]]. | #An '''upper brachial plexus lesion''', which occurs from excessive lateral neck flexion away from the shoulder. Most commonly, forceps delivery or falling on the neck at an angle causes upper plexus lesions leading to [[Erb's Palsy]]. This type of injury produces a very characteristic sign called ''Waiter's tip deformity'' due to loss of the lateral rotators of the shoulder, arm flexors, and hand extensor muscles.<ref name="Teach" /> | ||
#Less frequently, the '''whole brachial plexus lesion''' occurs. | #Less frequently, the '''whole brachial plexus lesion''' occurs. | ||
#Most infrequently, sudden upward pulling on an abducted arm (as when someone breaks a fall by grasping a tree branch) produces a '''lower brachial plexus lesion''', in which the eighth cervical (C8) and first thoracic (T1) nerves are injured either before or after they have joined to form the lower trunk. The subsequent paralysis affects | #Most infrequently, sudden upward pulling on an abducted arm (as when someone breaks a fall by grasping a tree branch) produces a '''lower brachial plexus lesion''', in which the eighth cervical (C8) and first thoracic (T1) nerves are injured either before or after they have joined to form the lower trunk. The subsequent paralysis affects the intrinsic muscles of the hand and the flexors of the wrist and fingers.This results in a form of paralysis known as [[Klumpke's Paralysis]].<ref name="Teach" /> | ||
However a commonly used one is '''Leffert's classification system''' which is based on | However, a commonly used one is '''Leffert's classification system''' which is based on etiology and level of injury: | ||
*I Open (usually from stabbing) | *I Open (usually from stabbing) | ||
*II Closed (usually from motorcycle accident) | *II Closed (usually from a motorcycle accident) | ||
*IIa Supraclavicular (preganglionic or | *IIa Supraclavicular (preganglionic or postganglionic) | ||
*IIb Infraclavicular | *IIb Infraclavicular | ||
*IIc Combined | *IIc Combined | ||
*III Radiation induced | *III Radiation-induced | ||
*IV Obstetric | *IV Obstetric | ||
*IVa Erb's (upper root) | *IVa Erb's (upper root) | ||
*IVb Klumpke (lower root) | *IVb Klumpke (lower root) | ||
*IVc Mixed | *IVc Mixed | ||
=== Signs and Symptoms === | === Signs and Symptoms === | ||
Nerve damage causes a multifaceted clinical picture consisting of sensorimotor disturbances (pain, muscle atrophy, muscle weakness, secondary deformities) as well as | Nerve damage causes a multifaceted clinical picture consisting of sensorimotor disturbances (pain, muscle atrophy, muscle weakness, secondary deformities) as well as the reorganisation of the Central Nervous System that may be associated with upper limb underuse.<ref name="Smania">Smania N, Berto G, La Marchina E, Melotti C, Midiri A, Roncari L et al. Rehabilitation of brachial plexus injuries in adults and children. European Journal of Physical and Rehabilitation Medicine 2012; 48:483-506</ref> | ||
*'''Pain''' is most common, in particular those | *'''Pain''' is most common, in particular, those affecting the preganglionic fibres<ref name="Tabitha">Tabitha A. Washington, Khalilah M. Brown, Gilbert J. Fanciullo. Pain. Oxford University Press, 2012</ref>. Often described as crushing with intermittent severe attacks shooting down the arm. | ||
*'''Paralysis''' and '''anaesthesia''' | *'''Paralysis''' and '''anaesthesia'''in affected extremity. | ||
*Bizarre sensations, | *Bizarre sensations, hyperalgesia, dysesthesia, and allodynia. | ||
*Myoclonic jerks in the affected extremity. | *Myoclonic jerks in the affected extremity. | ||
*Ipsilateral [[Horner's Syndrome|Horners Syndrome]] | *Ipsilateral [[Horner's Syndrome|Horners Syndrome]]with T1 injury. | ||
=== Investigations | === Investigations<ref name="Slide" /> === | ||
*'''Xray''' of shoulder area and cervical spine to determine if any boney abnormalities are causing the lesion. | *'''Xray''' of the shoulder area and cervical spine to determine if any boney abnormalities are causing the lesion. | ||
*'''MRI''' will help to visualise causative pathology such as tumors, neuritis, radiation injury. | *'''MRI''' will help to visualise causative pathology such as tumors, neuritis, radiation injury. | ||
*'''EMG and NCS''' help to confirm diagnosis, localise lesion and determine degree of axonal loss. | *'''EMG and NCS''' help to confirm a diagnosis, localise the lesion and determine the degree of axonal loss. These tests are the most useful tests to determine localisation of the plexopathy, especially, the sensory nerve conduction studies (SCSs) because sensory nerve action potential amplitude will decrease in plexopathies due to [https://www.sciencedirect.com/topics/neuroscience/wallerian-degeneration Wallerian degeneration] of the postganglionic sensory fibers<ref name="Higashihara">Higashihara M, Sonoo M. Electrodiagnosis in plexopathies; an update. Rinsho Shinkeigaku. 2012;52(11):1243-5.</ref>. | ||
*'''Histamine test''' to differentiate between pre and postganglionic lesion<ref name="Tabitha" />. | *'''Histamine test''' to differentiate between pre and postganglionic lesion<ref name="Tabitha" />. | ||
=== Management === | === Management === | ||
brachial plexus injury may result in severe and chronic impairments in both adults and children, thus requiring | brachial plexus injury may result in severe and chronic impairments in both adults and children, thus requiring early and long-lasting treatment. <ref name="Smania" /> | ||
==== Medical Management ==== | ==== Medical Management ==== | ||
*The main aspect of medical management is pain control. | *The main aspect of medical management is pain control. Often treated in a similar way to neuropathic pain with NSAID, tricyclic antidepressants, anticonvulsants, and oral or transdermal opioids.<ref name="Sake">Sakellariou VI, Badilas NK, Stavropoulos NA, Mazis G, Kotoulas HK, Kyriakopoulos S, et al. Treatment options for brachial plexus injuries. ISRN Orthop. 2014:314137. doi: 10.1155/2014/314137.</ref> | ||
==== Psychological Management ==== | ==== Psychological Management ==== | ||
| Line 231: | Line 227: | ||
====Physiotherapy Management''' (see also [[Brachial plexus injury|Brachial Pluxus Injury]] for Physiotherapy Management) ==== | ====Physiotherapy Management''' (see also [[Brachial plexus injury|Brachial Pluxus Injury]] for Physiotherapy Management) ==== | ||
The aim is to maintain the range of motion of the extremity, to strengthen the remaining functional muscles, to protect the denervated dermatomes, and to manage pain. | The aim is to maintain the range of motion of the extremity, to strengthen the remaining functional muscles, to protect the denervated dermatomes, and to manage pain.<ref name="Sake" /> | ||
*Pain control - acupuncture, [[Transcutaneous Electrical Nerve Stimulation (TENS)|TENS]] | *Pain control - acupuncture, [[Transcutaneous Electrical Nerve Stimulation (TENS)|TENS]] | ||
*Maintaining ROM - passive movements, | *Maintaining ROM - passive movements,exercise therapy, splinting, positioning<ref name="Sake" /> | ||
*Strengthen affected muscles - [[biofeedback]], [[Exercise Therapy in the Rehabilitation of Spondylolisthesis in Fast Bowlers in Cricket|exercise therapy]] | *Strengthen affected muscles - [[biofeedback]], [[Exercise Therapy in the Rehabilitation of Spondylolisthesis in Fast Bowlers in Cricket|exercise therapy]] | ||
*Managing chronic oedema - compression garments, advice, [[Massage|massage therapy]] | *Managing chronic oedema - compression garments, advice, [[Massage|massage therapy]] | ||
==== Intervention Management ==== | ==== Intervention Management ==== | ||
*Continuous brachial plexus block | *Continuous brachial plexus block | ||
*Transcutaneous nerve stimulation | *Transcutaneous nerve stimulation | ||
*Dorsal route entry zone (DREZ) ablation or implantable dorsal route stimulators. | *Dorsal route entry zone (DREZ) ablation or implantable dorsal route stimulators. | ||
*Surgical techniques include neurolysis, nerve grafting and nerve transfer. | *Surgical techniques include neurolysis, nerve grafting, and nerve transfer. Intercostal nerves are commonly used to reinnervate muscles after a brachial plexus injury with avulsion of spinal nerve roots.<ref name="Sake" /><ref name="Dahlin">Dahlin LB, Andersson G, Backman C, Svensson H, Björkman A. Rehabilitation, Using Guided Cerebral Plasticity, of a Brachial Plexus Injury Treated with Intercostal and Phrenic Nerve Transfers. Front Neurol. 2017; 8: 72</ref> | ||
== Brachial Plexus Block == | == Brachial Plexus Block == | ||
A [http://en.wikipedia.org/wiki/Brachial_plexus_block brachial plexus block] allows a surgeon to operate on an upper extremity without the use of a general anesthetic, when combined with a tourniquet. | A [http://en.wikipedia.org/wiki/Brachial_plexus_block brachial plexus block] allows a surgeon to operate on an upper extremity without the use of a general anesthetic, when combined with a tourniquet.<ref name="Moore">Moore KL, Dalley AF. Clinically Oriented Anatomy, 5th ed. Philadelphia: Lippincott Williams and Wilkins, 2005.</ref> | ||
[ | The location of the injection is between the posterior border of the [[sternocleidomastoid]] and the clavicle. The axillary sheath surrounds the axillary vein, axillary artery, and three cords of the brachial plexus. When the injection takes effect, the muscles and skin innervated by the cords found in the sheath are anesthetized. <ref name="Moore" /> | ||
[http://www.nysora.com/peripheral_nerve_blocks/nerve_stimulator_techniques/3075-continuous_interscalene_brachial_plexus_block.html Read more here] | |||
< | {{#ev:youtube|WqNmWAPFB7c|300}}<ref>vidRASCI.Regional Anesthesia Study Center of Iowa. Ultrasound guided interscalene brachial plexus block . Available from: http://www.youtube.com/watch?v=WqNmWAPFB7c[last accessed 08/02/13]</ref> | ||
{| class="FCK__ShowTableBorders" width="40%" cellspacing="1" cellpadding="1" border="0" align="right" | {| class="FCK__ShowTableBorders" width="40%" cellspacing="1" cellpadding="1" border="0" align="right" | ||
|- | |- | ||
| | | | ||
|} | |} | ||
== Other Information == | == Other Information == | ||
Some mnemonics for remembering the branches: | Some mnemonics for remembering the branches: | ||
*Posterior Cord Branches | *Posterior Cord Branches | ||
**STAR - subscapular (upper and lower), thoracodorsal, axillary, radial | **STAR - subscapular (upper and lower), thoracodorsal, axillary, radial | ||
**ULTRA - upper subscapular, lower subscapular, thoracodorsal, radial, axillary | **ULTRA - upper subscapular, lower subscapular, thoracodorsal, radial, axillary | ||
*Lateral Cord Branches | *Lateral Cord Branches | ||
**LLM "Lucy Loves Me" - lateral pectoral, lateral root of the median nerve, musculocutaneous | **LLM "Lucy Loves Me" - the lateral pectoral, lateral root of the median nerve, musculocutaneous | ||
*Medial Cord Branches | *Medial Cord Branches | ||
**MMMUM "Most Medical Men Use Morphine" - medial pectoral, medial cutaneous nerve of arm, medial cutaneous nerve of forearm, ulnar, medial root of the median nerve | **MMMUM "Most Medical Men Use Morphine" - medial pectoral, medial cutaneous nerve of arm, medial cutaneous nerve of forearm, ulnar, the medial root of the median nerve | ||
== Resources == | == Resources == | ||
[http://www.jbppni.com Journal of Brachial Plexus and Peripheral Nerve Injury] | [http://www.jbppni.com Journal of Brachial Plexus and Peripheral Nerve Injury] | ||
== Presentations == | == Presentations == | ||
| Line 288: | Line 280: | ||
rect 0 0 220 126 [http://www.ama-assn.org/ama1/pub/upload/mm/15/brachial_plex_how_to.pdf] | rect 0 0 220 126 [http://www.ama-assn.org/ama1/pub/upload/mm/15/brachial_plex_how_to.pdf] | ||
desc none | desc none | ||
</imagemap> | </imagemap> | ||
| [http://www.ama-assn.org/ama1/pub/upload/mm/15/brachial_plex_how_to.pdf '''Learn the Brachial Plexus in Five Minutes or Less'''] | | [http://www.ama-assn.org/ama1/pub/upload/mm/15/brachial_plex_how_to.pdf '''Learn the Brachial Plexus in Five Minutes or Less'''] | ||
This is a great little presentation to teach you the brachial plexus through simplified drawing. | This is a great little presentation to teach you the brachial plexus through simplified drawing. | ||
[http://www.ama-assn.org/ama1/pub/upload/mm/15/brachial_plex_how_to.pdf Have a go!] | [http://www.ama-assn.org/ama1/pub/upload/mm/15/brachial_plex_how_to.pdf Have a go!] | ||
|} | |} | ||
| Line 302: | Line 294: | ||
rect 0 0 220 126 [https://connect.regis.edu/p12894565/] | rect 0 0 220 126 [https://connect.regis.edu/p12894565/] | ||
desc none | desc none | ||
</imagemap> | </imagemap> | ||
| [https://connect.regis.edu/p12894565/ '''Brachial Plexus Block and Translational Manipulation for Adhesive Capsulitis'''] | | [https://connect.regis.edu/p12894565/ '''Brachial Plexus Block and Translational Manipulation for Adhesive Capsulitis'''] | ||
Created by Tom Denninger & Ben Hando as part of the Evidence in Motion, OMPT Fellowship, 2011 | Created by Tom Denninger & Ben Hando as part of the Evidence in Motion, OMPT Fellowship, 2011 | ||
[https://connect.regis.edu/p12894565/ View the presentation] | [https://connect.regis.edu/p12894565/ View the presentation] | ||
|} | |} | ||
</div> | </div> | ||
== Case Studies == | == Case Studies == | ||
Dahlin LB, Blackman C, Duppe H, Saito H, Chemnitz A, Abul-Kasim K, Maly P. [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2742518/pdf/1749-7221-4-14.pdf Compression of the lower trunk of the brachial plexus by a cervical rib in two adolescent girls: case reports and surgical treatment]. J Brachial Plex Peripher Nerve Inj. 2009;4(14).] - [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2742518/pdf/1749-7221-4-14.pdf FREE FULL TEXT] | Dahlin LB, Blackman C, Duppe H, Saito H, Chemnitz A, Abul-Kasim K, Maly P. [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2742518/pdf/1749-7221-4-14.pdf Compression of the lower trunk of the brachial plexus by a cervical rib in two adolescent girls: case reports and surgical treatment]. J Brachial Plex Peripher Nerve Inj. 2009;4(14).] - [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2742518/pdf/1749-7221-4-14.pdf FREE FULL TEXT] | ||
Saliba S, Saliba EN, Pugh KF, Chhabra A, Diduch D. [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3445178/pdf/10.1177_1941738109343544.pdf Rehabilitation considerations of a brachial plexus injury with complete avulsion of C5 and C6 nerve roots in a | Saliba S, Saliba EN, Pugh KF, Chhabra A, Diduch D. [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3445178/pdf/10.1177_1941738109343544.pdf Rehabilitation considerations of a brachial plexus injury with complete avulsion of C5 and C6 nerve roots in a college football player: A Case Study]. Sports Health. 2009:1(5): 370-375. - [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3445178/pdf/10.1177_1941738109343544.pdf FREE FULL TEXT] | ||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Anatomy]] | [[Category:Anatomy]] | ||
[[Category:Cervical_Spine]] | [[Category:Cervical_Spine]] | ||
[[Category:Shoulder]] | [[Category:Shoulder]] | ||
[[Category:Nerves]] | [[Category:Nerves]] | ||
[[Category:Neurodynamics]] | [[Category:Neurodynamics]] | ||
[[Category:Musculoskeletal/Orthopaedics]] | [[Category:Musculoskeletal/Orthopaedics]] | ||
[[Category:EIM_Residency_Project]] | [[Category:EIM_Residency_Project]] | ||
[[Category:Sports Medicine]] | [[Category:Sports Medicine]] | ||
[[Category:Upper Extremity]] | [[Category:Upper Extremity]] | ||
Revision as of 21:20, 22 July 2019
Original Editor - Matt Anderson
Top Contributors - Admin, Kapil Narale, Kim Jackson, George Prudden, Tony Lowe, Uchechukwu Chukwuemeka, Matt Anderson, Laura Ritchie, Joshua Samuel, Sweta Christian, Lucinda hampton, Wanda van Niekerk, 127.0.0.1, Amanda Ager, Wendy Walker, Evan Thomas, Scott Buxton, Naomi O'Reilly and WikiSysop
Introduction[edit | edit source]
The Brachial Plexus is a network of nerve fibers that run from the spine, passing through the cervico-axillary canal to reach axilla. It is formed by the ventral rami of the lower four cervical and first thoracic nerve roots (C5-C8, T1).[1]
Function[edit | edit source]
The brachial plexus is responsible for cutaneous and muscular innervation of the entire upper limb, with two exceptions: the trapezius muscle innervated by the spinal accessory nerve (CN XI) and an area of skin near the axilla innervated by the intercostobrachial nerve.[2]
Description[edit | edit source]
Path[3][4][edit | edit source]
The brachial plexus is divided into Roots, Trunks, Divisions, Cords, and Branches. There are five "terminal" branches and numerous other "pre-terminal" or "collateral" branches that leave the plexus at various points along its length.
- The five Roots are the five anterior rami of the lower four cervical and first thoracic nerve roots (C5-C8, T1) after they have given off their segmental supply to the muscles of the neck. These Roots merge to form three Trunks:
- Upper Trunk (C5-C6)
- Middle Trunk (C7)
- Lower Trunk (C8, T1)
- Each Trunk then splits into anterior and posterior divisions, to form six Divisions. The anterior/ posterior divisions innervate flexor groups versus extensor groups:
- anterior divisions of the upper, middle, and lower trunks
- posterior divisions of the upper, middle, and lower trunks
- These six Divisions will regroup to become the three Cords. The Cords are named by their position to the axillary artery.
- The Posterior Cord is formed from the three posterior divisions of the trunks (C5-C8, T1)
- The Lateral Cord is the anterior divisions from the upper and middle trunks (C5-C7)
- The Medial Cord is simply a continuation of the anterior division of the lower trunk (C8, T1)
Specific Branches[1][3][edit | edit source]
The branches are listed below. They mostly branch from the cords, but some originate from earlier structures (indicated in italics).
Bold indicates primary spinal root component of the nerve. Italics indicate spinal roots that frequently, but not always, contribute to the nerve.
| From | Nerve | Roots | Muscles | Cutaneous |
| roots | Dorsal scapular nerve | C4, C5 | Rhomboid muscles and Levator scapulae | - |
| roots | Long thoracic nerve | C5, C6, C7 | Serratus anterior | - |
| upper trunk | Nerve to the subclavius | C5, C6 | Subclavius muscle | - |
| upper trunk | Suprascapular nerve | C5, C6 | Supraspinatus and Infraspinatus | - |
| lateral cord | Lateral pectoral nerve | C5, C6, C7 | Pectoralis major and Pectoralis minor (by communicating with the Medial pectoral nerve) | - |
| lateral cord | Musculocutaneous nerve | C5, C6, C7 | Coracobrachialis, Brachialis and Biceps brachii | becomes the Lateral cutaneous nerve of the forearm |
| lateral cord | lateral root of the Median nerve | C6, C7 | fibres to the median nerve | - |
| posterior cord | Upper subscapular nerve | C5, C6 | Subscapularis (upper part) | - |
| posterior cord | Thoracodorsal nerve (middle subscapular nerve) | C6, C7, C8 | Latissimus dorsi | - |
| posterior cord | Lower subscapular nerve | C5, C6 | subscapularis (lower part ) and Teres major | - |
| posterior cord | Axillary nerve | C5, C6 | anterior branch: deltoid and a small area of overlying skin posterior branch: Teres minor and deltoid muscles | posterior branch becomes Upper lateral cutaneous nerve of the arm |
| posterior cord | Radial nerve | C5, C6, C7, C8, T1 | Triceps brachii, Supinator, Anconeus, the extensor muscles of the Forearm, and Brachioradialis | skin of the posterior arm as the Posterior cutaneous nerve of the arm |
| medial cord | Medial pectoral nerve | C8, T1 | Pectoralis major and Pectoralis minor | - |
| medial cord | medial root of the Median nerve | C8, T1 | fibres to the median nerve | portions of hand not served by ulnar or radial |
| medial cord | Medial cutaneous nerve of the arm | C8, T1 | - | front and medial skin of the Arm |
| medial cord | Medial cutaneous nerve of the forearm | C8, T1 | - | medial skin of the forearm |
| medial cord | Ulnar nerve | C8, T1 | Flexor carpi ulnaris, the medial two bellies of Flexor digitorum profundus, the intrinsic hand muscles except the Thenar muscles and the two most lateral lumbricals | the skin of the medial side of the hand and medial one and a half fingers on the palmar side and medial two and a half fingers on the dorsal side |
Specific branches can be visualised on the diagram below:
Injuries[edit | edit source]
Injury to the brachial plexus can be very problematic because the nerves branching off of the plexus provide innervation to the upper extremity. Clinical signs and symptoms vary with which area of the plexus is involved, and generally result in paralysis or anesthesia.[3]
Symptoms can range from transient nerve dysfunction to complete upper extremity weakness. Because of the anatomical variants[5] of the brachial plexus these injuries can be a challenge to diagnose.
Mechanism of Injury[edit | edit source]
The main causes of brachial plexus palsies are traction, due to extreme movements, and heavy impact. [6]
Brachial plexus injury can occur in a variety of ways and can occur as a result of shoulder trauma, tumours, or inflammation. The rare Parsonage-Turner Syndromecauses brachial plexus inflammation without obvious injury, but with nevertheless disabling symptoms. But in general, brachial plexus lesions can be classified as either traumatic or obstetric.
- Obstetric injuries may occur from a mechanical injury involving shoulder dystocia during a difficult childbirth. During birth, excessive stretching of the neck or pulling the upper extremity can result in an upper brachial plexus injury or inferior trunk, respectively. The incidence of brachial plexus injury is approximately 1 in 1,000 live births.[7]
- Traumatic injury may arise from penetrating or sports-related injuries, falls, work-related injuries, radiation therapy and iatrogenic causes (i.e. first rib resection, shoulder surgery, brachial plexus block). However, the most common mechanism of injury is a traction injury due to the forceful separation of the neck from the shoulder.
Common associated injuries can include fractures of the proximal humerus, clavicle, scapula, cervical spine and upper limb vascular injuries. [6]Management of these injuries may complicate the picture when diagnosing brachial plexus injury but can also guide in determining the mechanism of injury.
Classification of Injury[edit | edit source]
There are many classification systems for brachial plexus injuries, they can be divided into three types:
- An upper brachial plexus lesion, which occurs from excessive lateral neck flexion away from the shoulder. Most commonly, forceps delivery or falling on the neck at an angle causes upper plexus lesions leading to Erb's Palsy. This type of injury produces a very characteristic sign called Waiter's tip deformity due to loss of the lateral rotators of the shoulder, arm flexors, and hand extensor muscles.[1]
- Less frequently, the whole brachial plexus lesion occurs.
- Most infrequently, sudden upward pulling on an abducted arm (as when someone breaks a fall by grasping a tree branch) produces a lower brachial plexus lesion, in which the eighth cervical (C8) and first thoracic (T1) nerves are injured either before or after they have joined to form the lower trunk. The subsequent paralysis affects the intrinsic muscles of the hand and the flexors of the wrist and fingers.This results in a form of paralysis known as Klumpke's Paralysis.[1]
However, a commonly used one is Leffert's classification system which is based on etiology and level of injury:
- I Open (usually from stabbing)
- II Closed (usually from a motorcycle accident)
- IIa Supraclavicular (preganglionic or postganglionic)
- IIb Infraclavicular
- IIc Combined
- III Radiation-induced
- IV Obstetric
- IVa Erb's (upper root)
- IVb Klumpke (lower root)
- IVc Mixed
Signs and Symptoms[edit | edit source]
Nerve damage causes a multifaceted clinical picture consisting of sensorimotor disturbances (pain, muscle atrophy, muscle weakness, secondary deformities) as well as the reorganisation of the Central Nervous System that may be associated with upper limb underuse.[8]
- Pain is most common, in particular, those affecting the preganglionic fibres[9]. Often described as crushing with intermittent severe attacks shooting down the arm.
- Paralysis and anaesthesiain affected extremity.
- Bizarre sensations, hyperalgesia, dysesthesia, and allodynia.
- Myoclonic jerks in the affected extremity.
- Ipsilateral Horners Syndromewith T1 injury.
Investigations[4][edit | edit source]
- Xray of the shoulder area and cervical spine to determine if any boney abnormalities are causing the lesion.
- MRI will help to visualise causative pathology such as tumors, neuritis, radiation injury.
- EMG and NCS help to confirm a diagnosis, localise the lesion and determine the degree of axonal loss. These tests are the most useful tests to determine localisation of the plexopathy, especially, the sensory nerve conduction studies (SCSs) because sensory nerve action potential amplitude will decrease in plexopathies due to Wallerian degeneration of the postganglionic sensory fibers[10].
- Histamine test to differentiate between pre and postganglionic lesion[9].
Management[edit | edit source]
brachial plexus injury may result in severe and chronic impairments in both adults and children, thus requiring early and long-lasting treatment. [8]
Medical Management[edit | edit source]
- The main aspect of medical management is pain control. Often treated in a similar way to neuropathic pain with NSAID, tricyclic antidepressants, anticonvulsants, and oral or transdermal opioids.[11]
Psychological Management[edit | edit source]
- Psychological problems and a lack of cooperation by the patient may limit rehabilitation effects and increase disability.[8]
Physiotherapy Management (see also Brachial Pluxus Injury for Physiotherapy Management)[edit | edit source]
The aim is to maintain the range of motion of the extremity, to strengthen the remaining functional muscles, to protect the denervated dermatomes, and to manage pain.[11]
- Pain control - acupuncture, TENS
- Maintaining ROM - passive movements,exercise therapy, splinting, positioning[11]
- Strengthen affected muscles - biofeedback, exercise therapy
- Managing chronic oedema - compression garments, advice, massage therapy
Intervention Management[edit | edit source]
- Continuous brachial plexus block
- Transcutaneous nerve stimulation
- Dorsal route entry zone (DREZ) ablation or implantable dorsal route stimulators.
- Surgical techniques include neurolysis, nerve grafting, and nerve transfer. Intercostal nerves are commonly used to reinnervate muscles after a brachial plexus injury with avulsion of spinal nerve roots.[11][12]
Brachial Plexus Block[edit | edit source]
A brachial plexus block allows a surgeon to operate on an upper extremity without the use of a general anesthetic, when combined with a tourniquet.[13]
The location of the injection is between the posterior border of the sternocleidomastoid and the clavicle. The axillary sheath surrounds the axillary vein, axillary artery, and three cords of the brachial plexus. When the injection takes effect, the muscles and skin innervated by the cords found in the sheath are anesthetized. [13]
Other Information[edit | edit source]
Some mnemonics for remembering the branches:
- Posterior Cord Branches
- STAR - subscapular (upper and lower), thoracodorsal, axillary, radial
- ULTRA - upper subscapular, lower subscapular, thoracodorsal, radial, axillary
- Lateral Cord Branches
- LLM "Lucy Loves Me" - the lateral pectoral, lateral root of the median nerve, musculocutaneous
- Medial Cord Branches
- MMMUM "Most Medical Men Use Morphine" - medial pectoral, medial cutaneous nerve of arm, medial cutaneous nerve of forearm, ulnar, the medial root of the median nerve
Resources[edit | edit source]
Journal of Brachial Plexus and Peripheral Nerve Injury
Presentations[edit | edit source]
 |
Learn the Brachial Plexus in Five Minutes or Less
This is a great little presentation to teach you the brachial plexus through simplified drawing. |
 |
Brachial Plexus Block and Translational Manipulation for Adhesive Capsulitis
Created by Tom Denninger & Ben Hando as part of the Evidence in Motion, OMPT Fellowship, 2011 |
Case Studies[edit | edit source]
Dahlin LB, Blackman C, Duppe H, Saito H, Chemnitz A, Abul-Kasim K, Maly P. Compression of the lower trunk of the brachial plexus by a cervical rib in two adolescent girls: case reports and surgical treatment. J Brachial Plex Peripher Nerve Inj. 2009;4(14).] - FREE FULL TEXT
Saliba S, Saliba EN, Pugh KF, Chhabra A, Diduch D. Rehabilitation considerations of a brachial plexus injury with complete avulsion of C5 and C6 nerve roots in a college football player: A Case Study. Sports Health. 2009:1(5): 370-375. - FREE FULL TEXT
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 TeachMeAnatomy. TeachMeSeries, Educational Health Care Resource. http://teachmeanatomy.info/upper-limb/nerves/brachial-plexus/. (accessed 9 Apr 2017).
- ↑ Hoppenfeld S. Physical Examination of the Spine and Extremities. CTI Reviews 2014.
- ↑ 3.0 3.1 3.2 Dutton M. Orthopaedic Examination, Evaluation and Intervention. 2nd Ed. New York: McGraw-Hill, 2008.
- ↑ 4.0 4.1 SlideShare, LinkedIn Corporation. Brachial Plexus:Anatomy and localisation of lesion. www.slideshare.net/anjupaed/brachial-plexus (accessed 9 Apr 2017)
- ↑ Orebaugh SL, Williams BA. Brachial Plexus Anatomy: Normal and Variant. The Scientific World Journal. 2009;9:300-312.
- ↑ 6.0 6.1 Coene LN. Mechanisms of brachial plexus lesions. Clinical Neurology and Neurosurgery. 1993;95:24-29.
- ↑ Joyner B, Soto MA, Henry M. Adam. Brachial Plexus Injury. Pediatrics in Review. 2006;27:238
- ↑ 8.0 8.1 8.2 Smania N, Berto G, La Marchina E, Melotti C, Midiri A, Roncari L et al. Rehabilitation of brachial plexus injuries in adults and children. European Journal of Physical and Rehabilitation Medicine 2012; 48:483-506
- ↑ 9.0 9.1 Tabitha A. Washington, Khalilah M. Brown, Gilbert J. Fanciullo. Pain. Oxford University Press, 2012
- ↑ Higashihara M, Sonoo M. Electrodiagnosis in plexopathies; an update. Rinsho Shinkeigaku. 2012;52(11):1243-5.
- ↑ 11.0 11.1 11.2 11.3 Sakellariou VI, Badilas NK, Stavropoulos NA, Mazis G, Kotoulas HK, Kyriakopoulos S, et al. Treatment options for brachial plexus injuries. ISRN Orthop. 2014:314137. doi: 10.1155/2014/314137.
- ↑ Dahlin LB, Andersson G, Backman C, Svensson H, Björkman A. Rehabilitation, Using Guided Cerebral Plasticity, of a Brachial Plexus Injury Treated with Intercostal and Phrenic Nerve Transfers. Front Neurol. 2017; 8: 72
- ↑ 13.0 13.1 Moore KL, Dalley AF. Clinically Oriented Anatomy, 5th ed. Philadelphia: Lippincott Williams and Wilkins, 2005.
- ↑ vidRASCI.Regional Anesthesia Study Center of Iowa. Ultrasound guided interscalene brachial plexus block . Available from: http://www.youtube.com/watch?v=WqNmWAPFB7c[last accessed 08/02/13]