Avascular Necrosis: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) No edit summary |
||
| (33 intermediate revisions by 9 users not shown) | |||
| Line 6: | Line 6: | ||
== Definition/Description == | == Definition/Description == | ||
Avascular necrosis | Avascular necrosis/Osteonecrosis is a degenerative bone condition characterised by the death of cellular components of the bone secondary to an interruption of the subchondral blood supply. It typically affects the epiphysis of long bones at weight-bearing joints. Advanced disease may result in subchondral collapse which threatens the viability of the joint involved. Non-traumatic cases will typically present with mechanical pain of variable onset and severity and often difficult to localize. In early disease, the physical examination is often normal which inevitably causes a delay in diagnosis.<ref name=":0">Matthews AH, Stitson D. [https://www.ncbi.nlm.nih.gov/books/NBK537007/ Osteonecrosis]. InStatPearls. 2019. StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537007/ (last accessed 6 October 2019)</ref> | ||
This short video gives a good summary of the condition | |||
{{#ev:youtube|https://www.youtube.com/watch?v=w2ZOTDbEe-0|width}}<ref>Dr ER tv Avascular necrosis Available from: https://www.youtube.com/watch?v=w2ZOTDbEe-0 (last accessed 6.10.19)</ref> | |||
See [[Avascular Necrosis Femoral Head]] | |||
== | == Causes == | ||
Osteonecrosis is most common in the [[Hip Anatomy|hip]], but also seen in the [[humerus]], [[knee]], and talus and more rarely seen in the smaller bones of the [[Wrist and Hand|wrist]] such as the [[lunate]]<ref name=":0" /> or [[Scaphoid Fracture|scaphoid]]. | |||
It can be caused by trauma or non-traumatic events | |||
# '''Joint or bone trauma''' | |||
* An injury, such as a dislocated joint, might damage nearby blood vessels. | |||
* A [[fracture]] in a bone eg femoral head. | |||
* [[Cancer Rehabilitation and the Importance of Balance Training|Cancer]] treatments involving radiation also can weaken the bone and harm blood vessels. | |||
2. '''Non-traumatic''' | |||
* [[Alcoholism|Heavy drinking]] <ref name="Gruson">Gruson K, Kwon Y. Atraumatic osteonecrosis of the humeral head. Bulletin of the NYU Hospital for Joint Diseases. 2009;67(1):6-14.</ref><span style="font-size: 13.28px;"> and </span>[[Anabolic Steroid Abuse|steroid abuse]]<span style="font-size: 13.28px;"> </span>have been identified as major risk factors | |||
* Numerous studies have also concluded that hyperlipidemia in the femoral head, induced by steroid and alcohol use, are associated with osteonecrosis. Both of these factors precipitate an increase in fat volume in the bone marrow and blood lipid levels, thereby increasing the deposition of fat and interrupting blood flow to the femoral head. | |||
* Numerous studies have also concluded that hyperlipidemia in the femoral head, induced by steroid and alcohol use, are associated with | |||
* Glucocorticoid intake was found to have an even stronger association than alcohol use. | * Glucocorticoid intake was found to have an even stronger association than alcohol use. | ||
* Cigarette smoking: due to changes in nitric oxide bioavailability, there is an increased oxidative stress level and endothelial dysfunction | * Cigarette smoking: due to changes in nitric oxide bioavailability, there is an increased oxidative stress level and endothelial dysfunction | ||
* Obesity: osteonecrosis is positively associated with BMI. Overweight and obesity are, just like steroid and alcohol use, often associated | * [[Obesity]]: osteonecrosis is positively associated with BMI. Overweight and obesity are, just like steroid and alcohol use, often associated with hyperlipidemia. | ||
* A medical condition, such as [[Sickle Cell Anemia|sickle cell anemia]]<span style="font-size: 13.28px;"> or </span>[[Systemic Lupus Erythematosus]]<span style="font-size: 13.28px;">.</span> | * A medical condition, such as [[Sickle Cell Anemia|sickle cell anemia]]<span style="font-size: 13.28px;"> or </span>[[Systemic Lupus Erythematosus]]<span style="font-size: 13.28px;">.</span> | ||
<br> | <br>Studies show that there is a higher prevalence among males, this could be attributed to higher levels of smoking and alcohol use. Greater fluctuations in climate temperatures may also contribute to higher rates of non-traumatic osteonecrosis. <ref>Zhao DW, Yu M, Hu K, Wang W, Yang L, Wang BJ, et al. Prevalence of Nontraumatic Osteonecrosis of the Femoral Head and its Associated Risk Factors in the Chinese Population: Results from a Nationally Representative Survey. Chin Med J. 2015;128(21) : 2843-2850 (level 1a)</ref><br> | ||
Studies show that there is a higher prevalence among males, this could be attributed to higher levels of smoking and alcohol use. Greater fluctuations in climate temperatures may also contribute to higher rates of non-traumatic osteonecrosis. | |||
== Clinical Presentation | === Clinical Presentation === | ||
Symptoms include [[Pain Assessment|pain]] and decreased range of motion in the affected joint. In some cases, the condition is diagnosed during routine [[X-Rays|x-ray imaging]], due to a lack of overt symptoms<ref name="Gruson" />. The most common location for this condition to manifest is the head or neck of the [[Hip Anatomy|femur]] or [[Glenohumeral Joint|humerus]], and the [[Knee|knee joint]]<ref name="Gruson" />. | |||
In the beginning, this disease is asymptomatic. It is also plausible there is a segmental collapse present and the patient doesn’t feel it. As the disease progresses, the hip can become stiffer, which is visible in the gait of the patient when he starts to limp. Pain is also observed by support on the leg, in the buttock, groin, and thigh. | |||
Avascular necrosis can be classified into five different stages:<ref name="Lee">Lee MS, Hsieh PH, Shih CH, Wang CJ. Non-traumatic osteonecrosis of the femoral head – from clinical to bench. Chang Gung Med J 2010;33(4):351-360</ref> | |||
*'''Stage 1''': Radiographic changes are absent or show minor osteopenia. An MRI scan is required for identification (can show oedema). The onset of this disease is asymptomatic. | |||
*'''Stage 1''': Radiographic changes are absent or show minor | |||
*'''Stage 2''': First stage with radiographic changes. This stage is characterized by sclerosis of the superior central portion of the joint head and/or osteopenia and/or subchondral cysts. <br> | *'''Stage 2''': First stage with radiographic changes. This stage is characterized by sclerosis of the superior central portion of the joint head and/or osteopenia and/or subchondral cysts. <br> | ||
*'''Stage 3''': In this stage, the articular surface is depressed so that the round contour is compromised, without being significantly deformed. This leads to a joint space narrowing. | *'''Stage 3''': In this stage, the articular surface is depressed so that the round contour is compromised, without being significantly deformed. This leads to a joint space narrowing. A plain radiograph shows a crescent sign. | ||
*'''Stage 4''': This stage is characterized by a wide collapse of the subchondral bone and destruction of the underlying trabecular pattern. This can lead to secondary arthritis. | *'''Stage 4''': This stage is characterized by a wide collapse of the subchondral bone and destruction of the underlying trabecular pattern. This can lead to secondary arthritis. | ||
*'''Stage 5''': The final stage where both articular surfaces are affected, which leads to a dysfunctional joint. | *'''Stage 5''': The final stage where both articular surfaces are affected, which leads to a dysfunctional joint. | ||
For example, if a case presents itself where the patient | For example, if a case presents itself where the patient has [[Avascular Necrosis Femoral Head|osteonecrosis of the femoral head]]. Avascular necrosis most commonly affects the hip in more than 72% of the cases. The patient will have mild chronic pain in the hip, the groin, around the buttocks and at the antero-medial thigh, with a normal radiograph, they should undergo observation for ONFH and a Hip joints MRI. This pain is most commonly aggravated by activity and internal rotation in flexion. As the disease progresses, the pain may also become present at rest. Without treatment, 85% will progress to the collapse of the articular surface and will eventually require [[Total Hip Replacement|total hip arthroplasty]]. <ref name=":1">Bentley G. 2012. European Instructional. Lectures13th EFORT Congress. Berlin,Germany. 2012; 12: 148 e.v. (level 1a)</ref> | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
Osteonecrosis can be diagnosed with a thorough check of the historical background of the patient combined with physical examination. [[Anabolic Steroid Abuse|Steroid exposure]] and [[Alcoholism|alcohol abuse]] are important risk factors. The age of the patient can also provide clues to the disease | Osteonecrosis can be diagnosed with a thorough check of the historical background of the patient combined with physical examination. [[Anabolic Steroid Abuse|Steroid exposure]] and [[Alcoholism|alcohol abuse]] are important risk factors. The age of the patient can also provide clues to the disease because patients with osteonecrosis are generally younger than those with [[Osteoarthritis|osteoarthritis]]. Locking, popping, or a painful click during mobilization of the affected joint can point to the presence of loose osteochondral fragments<ref name="Gruson" />. In further stages of the disease, loss of mobilization and increased pain can be detected<ref name="Gruson" />. Once osteonecrosis is detected, the physician should assess other joints that may be at risk, such as the [[Hip|hip]], [[Shoulder|shoulder]], and [[Knee|knee]]<ref name="Gruson" />. | ||
In the early stages, this condition is asymptomatic, which makes diagnosis almost impossible. However early screening with [[MRI Scans|MRI]] is currently the best modality for diagnosis due to its sensitivity. The double line sign is an [[MRI Scans|MRI]] finding seen at the periphery of a region of osteonecrosis. It consists of an inner bright line representing granulation tissue and an outer dark line representing sclerotic bone. Measurement of the size and location of the necrotic lesion is a crucial prognostic parameter to predict collapse and can be better defined on an [[MRI Scans|MRI]]. <ref> | In the early stages, this condition is asymptomatic, which makes diagnosis almost impossible. However early screening with [[MRI Scans|MRI]] is currently the best modality for diagnosis due to its sensitivity. The double line sign is an [[MRI Scans|MRI]] finding seen at the periphery of a region of osteonecrosis. It consists of an inner bright line representing granulation tissue and an outer dark line representing sclerotic bone. Measurement of the size and location of the necrotic lesion is a crucial prognostic parameter to predict collapse and can be better defined on an [[MRI Scans|MRI]]. <ref>Niknejad MT, Gaillard F. Crescent sign of avascular necrosis. Available from<nowiki/>https://radiopaedia.org/articles/crescent-sign-of-avascular-necrosis-1' (accessed 22 February 2020)(level 5)</ref> <br> | ||
At a more advanced stage, standard [[Diagnostic Imaging for Physical Therapists|radiographs]] can confirm the diagnose. Tissue affected by avascular necrosis will appear | At a more advanced stage, standard [[Diagnostic Imaging for Physical Therapists|radiographs]] can confirm the diagnose. Tissue affected by avascular necrosis will appear denser (increased whiteness) and possibly sclerotic (patchy) on the radiograph<ref name="Magee">Magee DJ. Orthopedic physical assessment. Saunders:St Louis, MO;2008.</ref>. An [[MRI Scans|MRI]] can assist in making the diagnosis. It can show a subchondral radiolucency called a “crescent sign”, it indicates imminent articular collapse. <br> | ||
== Outcome Measures == | == Outcome Measures == | ||
A functional outcome measure is useful for establishing the patient's baseline function and setting measurable goals. See [[Outcome Measures]] Database for more. | |||
Choice of outcome measure will be dependent on the joint affected | Choice of outcome measure will be dependent on the joint affected. | ||
1. [[Harris Hip Score|The Harris Hip Score]] | 1. [[Harris Hip Score|The Harris Hip Score]] | ||
2.[[4-Item Pain Intensity Measure (P4)]], [[Numeric Pain Rating Scale]], or [[Visual Analogue Scale]] ( if the patient reports symptoms of pain) | |||
3. [[Hip Disability and Osteoarthritis Outcome Score|Hip Disability and Osteoarthritis Outcome Score ]]<span style="font-size: 13.28px;"> (HOOS) </span> | |||
== Medical Management == | |||
*'''Pharmacological Therapy<br>'''Pharmacological therapy with anticoagulants, statins, and vasodilators seems to be effective to delay the progress of joint degeneration in the early stages of avascular necrosis. Although, there is very low evidence to support the use of these pharmacological agents in the treatment of osteonecrosis. Another still experimental treatment is Bisphosphonates. Hypothetically in the early stages of AVN the use of bisphosphonates could inhibit osteoclastic activity preventing subchondral bone collapse. <ref name="Klumpp">Klumpp R, Trevisan C. Aseptic osteonecrosis of the hip in the adult: current evidence on conservative treatment. Clinical Cases in Mineral and Bone Metabolism. 2015;12(Suppl 1):39–42. (level 2a)</ref><br> | |||
*'''Surgical Treatment'''<br><u>Core decompression</u> (for stages 1 and 2 of the disease) creates a tract for example in the femoral head that decompresses the head. Hereby facilitating increased blood flow, which will then promote neo-vascularization that could possibly stimulate new bone growth. With the<br>advent of microsurgery, this surgery can also be done with a bone graft. After you debride the necrotic array, you substitute the necrotic bone with a viable bone (most of the time 15 centimeters of the fibula with the peroneal artery connected to the ascending branch of the<br>lateral femoral circumflex artery and vein) and to initiate callus formation inside the femoral head.<br><br><u>[[Osteotomy|Osteotomy]]</u> is a surgical operation whereby a bone is cut to shorten or lengthen it or to change its alignment to decrease the load from the necrotic bone either by rotation of the femoral head and neck or by a varus or valgus angulation of the proximal [[femur]]. This treatment is only for young patients without co-morbidities interfering with bone healing. In the United States, angular osteotomy for stage II or III diseases at the time of intervention has had limited success ranging from 70% to 90% at a follow up from 3 to 18 years.<ref name=":1" /> <br><br>When all other things fail, a <u>[[Total Hip Replacement|total hip arthroplasty]]</u> (commonly in stages 3 and 4) is the only option. In this [[Total Hip Replacement|total hip replacement]] the damaged bone and cartilage are removed and replaced with prosthetic components.<br> • The damaged femoral head is removed and replaced with a metal stem that is placed into the hollow center of the femur.<br> • A metal or ceramic ball is placed on the upper part of the stem (replaces the femoral head)<br> • The damaged cartilage surface of the socket (acetabulum) is removed and replaced with a metal socket.<br> • A plastic, ceramic, or metal spacer is inserted between the new ball and the socket to allow for a smooth gliding surface.<br>Studies show that total hip arthroplasty (32-mm alumina-on-alumina ) in patients with avascular necrosis of the femoral head after a 2 to 10-year follow-up, show good results for long-lasting replacements. It shows a better Harris hip score and pain relief after surgery. <ref>Garino JP, Steinberg ME. Total Hip Arthroplasty in Patients with Avascular Necrosis of the Femoral Head; A 2-to 10-Year Followup. Clinical orthopaedics and related research. 1997; 334: 108-115. (level 2a)</ref> | |||
== Physical Therapy Management == | |||
= Physical Therapy Management = | |||
Appropriate treatment for avascular necrosis is necessary to prevent further deterioration of the joint. If untreated, most patients will experience severe pain and limitation of movement within two years. Although physical therapy cannot cure avascular necrosis, it can slow down the progression of the disease and decrease associated pain. It is suggested that patients with Stage 1 and 2 osteonecrosis could benefit from a physical therapy program<ref name="Lee" />. Most patients will eventually need surgical treatment, such as core decompression or arthroplasty<ref name="Gruson" />. | Appropriate treatment for avascular necrosis is necessary to prevent further deterioration of the joint. If untreated, most patients will experience severe pain and limitation of movement within two years. Although physical therapy cannot cure avascular necrosis, it can slow down the progression of the disease and decrease associated pain. It is suggested that patients with Stage 1 and 2 osteonecrosis could benefit from a physical therapy program<ref name="Lee" />. Most patients will eventually need surgical treatment, such as core decompression or arthroplasty<ref name="Gruson" />. | ||
| Line 112: | Line 81: | ||
#Improvement of functionality | #Improvement of functionality | ||
Nonoperative treatment begins with patient education and addressing known risk factors, such as smoking and alcohol abuse. In addition, corticosteroids should be avoided<ref name="Lee" />. | Nonoperative treatment begins with patient education and addressing known risk factors, such as smoking and alcohol abuse. In addition, [[Corticosteroid Medication|corticosteroids]] should be avoided<ref name="Lee" />. | ||
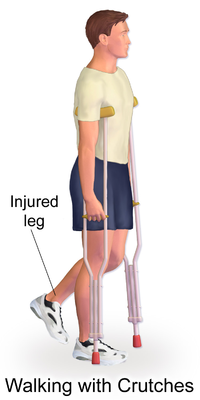
[[File:Crutches Walking.png|right|frameless|400x400px]] | |||
To assist the patient in regaining function and relieve painful symptoms, [[Crutches|crutches]] or other [[Walking Aids|gait aids]] can be introduced. The physical therapist should instruct the patient | To assist the patient in regaining function and relieve painful symptoms, [[Crutches|crutches]] or other [[Walking Aids|gait aids]] can be introduced. The physical therapist should instruct the patient on how to properly use these devices. <br>By using crutches, the load that the hip joint bears, will be decreased. This weight-bearing restriction is an important conservative treatment. In literature, it is considered that weight-bearing restriction as a stand-alone therapy is insufficient in preventing disease progression, but it’s a reasonable treatment option when combined with pharmacological agents or surgery. <ref name="Klumpp" /> | ||
Physical therapy treatment focuses on exercises to maintain joint mobility and strengthen the muscles around the affected joint. During physical therapy, excessive compressive and shear forces on the joint should be avoided. The outcome depends on the lesion’s size and stage at the initiation of the treatment. | Physical therapy treatment focuses on exercises to maintain joint mobility and strengthen the muscles around the affected joint. During physical therapy, excessive compressive and shear forces on the joint should be avoided. The outcome depends on the lesion’s size and stage at the initiation of the treatment. | ||
In order to maintain joint mobility, both passive and active exercises should be initiated. Passive exercises contain passive movements of the hip and stretching exercises. Active exercises consist of 3dimensional motions of the hip joint and can be applied during standing, sitting on a chair or while lying down. In the next stage, strengthening exercises are added. These exercises will focus on the muscles of the hip and thigh but will also include exercises for the core area as they play a large supporting role. To improve functionality it is important to implement endurance training and coordination training in a more advanced stage of the therapy. Endurance can be trained by walking on a treadmill or cycling on a home trainer. To improve coordination, walking exercises with increased complexity and balancing exercises can be adopted in physical therapy sessions. | In order to maintain joint mobility, both passive and active exercises should be initiated. Passive exercises contain passive movements of the hip and stretching exercises. Active exercises consist of 3dimensional motions of the hip joint and can be applied during standing, sitting on a chair or while lying down. In the next stage, strengthening exercises are added. These exercises will focus on the muscles of the hip and thigh but will also include exercises for the core area as they play a large supporting role. To improve functionality it is important to implement endurance training and coordination training in a more advanced stage of the therapy. Endurance can be trained by walking on a treadmill or cycling on a home trainer. To improve coordination, walking exercises with increased complexity and balancing exercises can be adopted in physical therapy sessions. <ref name="Lynne">Neumayr LD, Aguilar C, Earles AN, Jergesen HE, Haberkern CM, Kammen BF, et al. Physical therapy alone compared with core decompression and physical therapy for femoral head osteonecrosis in sickle cell disease. J Bone Joint Surg Am. 2006; 88(12): 2573-2582. (level 1b)</ref><br> | ||
Physical therapy after surgery is also a key component for recovery. It starts immediately the day after surgery. They prepare the patients for discharge by showing them how to do their everyday activities like getting in and out of bed and walking with a walker or crutches. <ref>Mass general, Total Hip Replacement, Rehabilitation & Physical Therapy Protocols 'http://www.massgeneral.org/ortho-hip-knee/patient-education/pt-ed-hiprehab.pdf' (level 5)</ref>(level 5) | |||
= Resources = | <br>In a more advanced stage of the therapy, the therapist instructs the patient on exercises to strengthen their muscles, improve range of motion, work on balance and gait speed. The patient specifically learns how to move, while maintaining hip precautions. The rehabilitation protocol is combined with a home exercise program. Below is an example of a training program in an advanced phase of recovery <ref>Paula Miller, Treating Avascular Necrosis, 21(17):23 (level 5)</ref> | ||
== Resources == | |||
Gruson K, Kwon Y. Atraumatic osteonecrosis of the humeral head. Bulletin of the NYU Hospital for Joint Diseases 2009;67(1):6-14. | Gruson K, Kwon Y. Atraumatic osteonecrosis of the humeral head. Bulletin of the NYU Hospital for Joint Diseases 2009;67(1):6-14. | ||
Lee MS, Hsieh PH, Shih CH, Wang CJ. Non-traumatic osteonecrosis of the femoral head – from clinical to bench. Chang Gung Med J 2010;33(4) | Lee MS, Hsieh PH, Shih CH, Wang CJ. Non-traumatic osteonecrosis of the femoral head – from clinical to bench. Chang Gung Med J 2010;33(4):351-60 | ||
Huijbregts P. Osteonecrosis of the humeral head: a literature review and two case studies. J Man Manip Ther 2000;8(4):175-182. | Huijbregts P. Osteonecrosis of the humeral head: a literature review and two case studies. J Man Manip Ther 2000;8(4):175-182. | ||
Hasan | Hasan SS, Romeo AA, Nontraumatic osteonecrosis of the humeral head. J Shoulder Elbow Surg 2002;11:281-98 | ||
= | == References == | ||
= References = | |||
<references /> | <references /> <br> | ||
[[Category: | [[Category:Bones]] | ||
[[Category:Conditions]] | |||
[[Category:Musculoskeletal/Orthopaedics]] | |||
[[Category:Bone - Conditions]] | |||
Latest revision as of 13:27, 15 December 2022
Original Editor - Kenny Bosmans
Top Contributors - Linde Van Droogenbroeck, Kenny Bosmans, Kim Jackson, Uchechukwu Chukwuemeka, Lucinda hampton, Admin, Rachael Lowe, Daphne Jackson, WikiSysop, 127.0.0.1, Tony Lowe, Evan Thomas and Vidya Acharya
Definition/Description[edit | edit source]
Avascular necrosis/Osteonecrosis is a degenerative bone condition characterised by the death of cellular components of the bone secondary to an interruption of the subchondral blood supply. It typically affects the epiphysis of long bones at weight-bearing joints. Advanced disease may result in subchondral collapse which threatens the viability of the joint involved. Non-traumatic cases will typically present with mechanical pain of variable onset and severity and often difficult to localize. In early disease, the physical examination is often normal which inevitably causes a delay in diagnosis.[1]
This short video gives a good summary of the condition
See Avascular Necrosis Femoral Head
Causes[edit | edit source]
Osteonecrosis is most common in the hip, but also seen in the humerus, knee, and talus and more rarely seen in the smaller bones of the wrist such as the lunate[1] or scaphoid.
It can be caused by trauma or non-traumatic events
- Joint or bone trauma
- An injury, such as a dislocated joint, might damage nearby blood vessels.
- A fracture in a bone eg femoral head.
- Cancer treatments involving radiation also can weaken the bone and harm blood vessels.
2. Non-traumatic
- Heavy drinking [3] and steroid abuse have been identified as major risk factors
- Numerous studies have also concluded that hyperlipidemia in the femoral head, induced by steroid and alcohol use, are associated with osteonecrosis. Both of these factors precipitate an increase in fat volume in the bone marrow and blood lipid levels, thereby increasing the deposition of fat and interrupting blood flow to the femoral head.
- Glucocorticoid intake was found to have an even stronger association than alcohol use.
- Cigarette smoking: due to changes in nitric oxide bioavailability, there is an increased oxidative stress level and endothelial dysfunction
- Obesity: osteonecrosis is positively associated with BMI. Overweight and obesity are, just like steroid and alcohol use, often associated with hyperlipidemia.
- A medical condition, such as sickle cell anemia or Systemic Lupus Erythematosus.
Studies show that there is a higher prevalence among males, this could be attributed to higher levels of smoking and alcohol use. Greater fluctuations in climate temperatures may also contribute to higher rates of non-traumatic osteonecrosis. [4]
Clinical Presentation[edit | edit source]
Symptoms include pain and decreased range of motion in the affected joint. In some cases, the condition is diagnosed during routine x-ray imaging, due to a lack of overt symptoms[3]. The most common location for this condition to manifest is the head or neck of the femur or humerus, and the knee joint[3].
In the beginning, this disease is asymptomatic. It is also plausible there is a segmental collapse present and the patient doesn’t feel it. As the disease progresses, the hip can become stiffer, which is visible in the gait of the patient when he starts to limp. Pain is also observed by support on the leg, in the buttock, groin, and thigh.
Avascular necrosis can be classified into five different stages:[5]
- Stage 1: Radiographic changes are absent or show minor osteopenia. An MRI scan is required for identification (can show oedema). The onset of this disease is asymptomatic.
- Stage 2: First stage with radiographic changes. This stage is characterized by sclerosis of the superior central portion of the joint head and/or osteopenia and/or subchondral cysts.
- Stage 3: In this stage, the articular surface is depressed so that the round contour is compromised, without being significantly deformed. This leads to a joint space narrowing. A plain radiograph shows a crescent sign.
- Stage 4: This stage is characterized by a wide collapse of the subchondral bone and destruction of the underlying trabecular pattern. This can lead to secondary arthritis.
- Stage 5: The final stage where both articular surfaces are affected, which leads to a dysfunctional joint.
For example, if a case presents itself where the patient has osteonecrosis of the femoral head. Avascular necrosis most commonly affects the hip in more than 72% of the cases. The patient will have mild chronic pain in the hip, the groin, around the buttocks and at the antero-medial thigh, with a normal radiograph, they should undergo observation for ONFH and a Hip joints MRI. This pain is most commonly aggravated by activity and internal rotation in flexion. As the disease progresses, the pain may also become present at rest. Without treatment, 85% will progress to the collapse of the articular surface and will eventually require total hip arthroplasty. [6]
Diagnostic Procedures[edit | edit source]
Osteonecrosis can be diagnosed with a thorough check of the historical background of the patient combined with physical examination. Steroid exposure and alcohol abuse are important risk factors. The age of the patient can also provide clues to the disease because patients with osteonecrosis are generally younger than those with osteoarthritis. Locking, popping, or a painful click during mobilization of the affected joint can point to the presence of loose osteochondral fragments[3]. In further stages of the disease, loss of mobilization and increased pain can be detected[3]. Once osteonecrosis is detected, the physician should assess other joints that may be at risk, such as the hip, shoulder, and knee[3].
In the early stages, this condition is asymptomatic, which makes diagnosis almost impossible. However early screening with MRI is currently the best modality for diagnosis due to its sensitivity. The double line sign is an MRI finding seen at the periphery of a region of osteonecrosis. It consists of an inner bright line representing granulation tissue and an outer dark line representing sclerotic bone. Measurement of the size and location of the necrotic lesion is a crucial prognostic parameter to predict collapse and can be better defined on an MRI. [7]
At a more advanced stage, standard radiographs can confirm the diagnose. Tissue affected by avascular necrosis will appear denser (increased whiteness) and possibly sclerotic (patchy) on the radiograph[8]. An MRI can assist in making the diagnosis. It can show a subchondral radiolucency called a “crescent sign”, it indicates imminent articular collapse.
Outcome Measures[edit | edit source]
A functional outcome measure is useful for establishing the patient's baseline function and setting measurable goals. See Outcome Measures Database for more.
Choice of outcome measure will be dependent on the joint affected.
2.4-Item Pain Intensity Measure (P4), Numeric Pain Rating Scale, or Visual Analogue Scale ( if the patient reports symptoms of pain)
3. Hip Disability and Osteoarthritis Outcome Score (HOOS)
Medical Management[edit | edit source]
- Pharmacological Therapy
Pharmacological therapy with anticoagulants, statins, and vasodilators seems to be effective to delay the progress of joint degeneration in the early stages of avascular necrosis. Although, there is very low evidence to support the use of these pharmacological agents in the treatment of osteonecrosis. Another still experimental treatment is Bisphosphonates. Hypothetically in the early stages of AVN the use of bisphosphonates could inhibit osteoclastic activity preventing subchondral bone collapse. [9]
- Surgical Treatment
Core decompression (for stages 1 and 2 of the disease) creates a tract for example in the femoral head that decompresses the head. Hereby facilitating increased blood flow, which will then promote neo-vascularization that could possibly stimulate new bone growth. With the
advent of microsurgery, this surgery can also be done with a bone graft. After you debride the necrotic array, you substitute the necrotic bone with a viable bone (most of the time 15 centimeters of the fibula with the peroneal artery connected to the ascending branch of the
lateral femoral circumflex artery and vein) and to initiate callus formation inside the femoral head.
Osteotomy is a surgical operation whereby a bone is cut to shorten or lengthen it or to change its alignment to decrease the load from the necrotic bone either by rotation of the femoral head and neck or by a varus or valgus angulation of the proximal femur. This treatment is only for young patients without co-morbidities interfering with bone healing. In the United States, angular osteotomy for stage II or III diseases at the time of intervention has had limited success ranging from 70% to 90% at a follow up from 3 to 18 years.[6]
When all other things fail, a total hip arthroplasty (commonly in stages 3 and 4) is the only option. In this total hip replacement the damaged bone and cartilage are removed and replaced with prosthetic components.
• The damaged femoral head is removed and replaced with a metal stem that is placed into the hollow center of the femur.
• A metal or ceramic ball is placed on the upper part of the stem (replaces the femoral head)
• The damaged cartilage surface of the socket (acetabulum) is removed and replaced with a metal socket.
• A plastic, ceramic, or metal spacer is inserted between the new ball and the socket to allow for a smooth gliding surface.
Studies show that total hip arthroplasty (32-mm alumina-on-alumina ) in patients with avascular necrosis of the femoral head after a 2 to 10-year follow-up, show good results for long-lasting replacements. It shows a better Harris hip score and pain relief after surgery. [10]
Physical Therapy Management [edit | edit source]
Appropriate treatment for avascular necrosis is necessary to prevent further deterioration of the joint. If untreated, most patients will experience severe pain and limitation of movement within two years. Although physical therapy cannot cure avascular necrosis, it can slow down the progression of the disease and decrease associated pain. It is suggested that patients with Stage 1 and 2 osteonecrosis could benefit from a physical therapy program[5]. Most patients will eventually need surgical treatment, such as core decompression or arthroplasty[3].
Nonoperative treatment involves three main goals:[3]
- Relief of symptoms
- Prevention of disease progression
- Improvement of functionality
Nonoperative treatment begins with patient education and addressing known risk factors, such as smoking and alcohol abuse. In addition, corticosteroids should be avoided[5].
To assist the patient in regaining function and relieve painful symptoms, crutches or other gait aids can be introduced. The physical therapist should instruct the patient on how to properly use these devices.
By using crutches, the load that the hip joint bears, will be decreased. This weight-bearing restriction is an important conservative treatment. In literature, it is considered that weight-bearing restriction as a stand-alone therapy is insufficient in preventing disease progression, but it’s a reasonable treatment option when combined with pharmacological agents or surgery. [9]
Physical therapy treatment focuses on exercises to maintain joint mobility and strengthen the muscles around the affected joint. During physical therapy, excessive compressive and shear forces on the joint should be avoided. The outcome depends on the lesion’s size and stage at the initiation of the treatment.
In order to maintain joint mobility, both passive and active exercises should be initiated. Passive exercises contain passive movements of the hip and stretching exercises. Active exercises consist of 3dimensional motions of the hip joint and can be applied during standing, sitting on a chair or while lying down. In the next stage, strengthening exercises are added. These exercises will focus on the muscles of the hip and thigh but will also include exercises for the core area as they play a large supporting role. To improve functionality it is important to implement endurance training and coordination training in a more advanced stage of the therapy. Endurance can be trained by walking on a treadmill or cycling on a home trainer. To improve coordination, walking exercises with increased complexity and balancing exercises can be adopted in physical therapy sessions. [11]
Physical therapy after surgery is also a key component for recovery. It starts immediately the day after surgery. They prepare the patients for discharge by showing them how to do their everyday activities like getting in and out of bed and walking with a walker or crutches. [12](level 5)
In a more advanced stage of the therapy, the therapist instructs the patient on exercises to strengthen their muscles, improve range of motion, work on balance and gait speed. The patient specifically learns how to move, while maintaining hip precautions. The rehabilitation protocol is combined with a home exercise program. Below is an example of a training program in an advanced phase of recovery [13]
Resources[edit | edit source]
Gruson K, Kwon Y. Atraumatic osteonecrosis of the humeral head. Bulletin of the NYU Hospital for Joint Diseases 2009;67(1):6-14.
Lee MS, Hsieh PH, Shih CH, Wang CJ. Non-traumatic osteonecrosis of the femoral head – from clinical to bench. Chang Gung Med J 2010;33(4):351-60
Huijbregts P. Osteonecrosis of the humeral head: a literature review and two case studies. J Man Manip Ther 2000;8(4):175-182.
Hasan SS, Romeo AA, Nontraumatic osteonecrosis of the humeral head. J Shoulder Elbow Surg 2002;11:281-98
References[edit | edit source]
- ↑ 1.0 1.1 Matthews AH, Stitson D. Osteonecrosis. InStatPearls. 2019. StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537007/ (last accessed 6 October 2019)
- ↑ Dr ER tv Avascular necrosis Available from: https://www.youtube.com/watch?v=w2ZOTDbEe-0 (last accessed 6.10.19)
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 Gruson K, Kwon Y. Atraumatic osteonecrosis of the humeral head. Bulletin of the NYU Hospital for Joint Diseases. 2009;67(1):6-14.
- ↑ Zhao DW, Yu M, Hu K, Wang W, Yang L, Wang BJ, et al. Prevalence of Nontraumatic Osteonecrosis of the Femoral Head and its Associated Risk Factors in the Chinese Population: Results from a Nationally Representative Survey. Chin Med J. 2015;128(21) : 2843-2850 (level 1a)
- ↑ 5.0 5.1 5.2 Lee MS, Hsieh PH, Shih CH, Wang CJ. Non-traumatic osteonecrosis of the femoral head – from clinical to bench. Chang Gung Med J 2010;33(4):351-360
- ↑ 6.0 6.1 Bentley G. 2012. European Instructional. Lectures13th EFORT Congress. Berlin,Germany. 2012; 12: 148 e.v. (level 1a)
- ↑ Niknejad MT, Gaillard F. Crescent sign of avascular necrosis. Available fromhttps://radiopaedia.org/articles/crescent-sign-of-avascular-necrosis-1' (accessed 22 February 2020)(level 5)
- ↑ Magee DJ. Orthopedic physical assessment. Saunders:St Louis, MO;2008.
- ↑ 9.0 9.1 Klumpp R, Trevisan C. Aseptic osteonecrosis of the hip in the adult: current evidence on conservative treatment. Clinical Cases in Mineral and Bone Metabolism. 2015;12(Suppl 1):39–42. (level 2a)
- ↑ Garino JP, Steinberg ME. Total Hip Arthroplasty in Patients with Avascular Necrosis of the Femoral Head; A 2-to 10-Year Followup. Clinical orthopaedics and related research. 1997; 334: 108-115. (level 2a)
- ↑ Neumayr LD, Aguilar C, Earles AN, Jergesen HE, Haberkern CM, Kammen BF, et al. Physical therapy alone compared with core decompression and physical therapy for femoral head osteonecrosis in sickle cell disease. J Bone Joint Surg Am. 2006; 88(12): 2573-2582. (level 1b)
- ↑ Mass general, Total Hip Replacement, Rehabilitation & Physical Therapy Protocols 'http://www.massgeneral.org/ortho-hip-knee/patient-education/pt-ed-hiprehab.pdf' (level 5)
- ↑ Paula Miller, Treating Avascular Necrosis, 21(17):23 (level 5)