Upper-Crossed Syndrome
This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! (5/05/2020)
Introduction[edit | edit source]
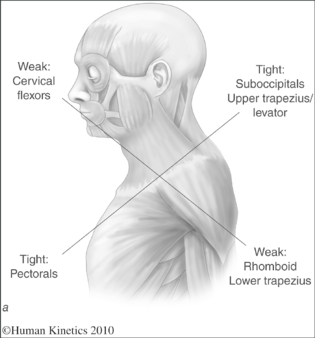
Upper-crossed syndrome (UCS) is also referred to as proximal or shoulder girdle crossed syndrome. In UCS, tightness of the upper trapezius and levator scapula on the dorsal side crosses with tightness of the pectoralis major and minor. Weakness of the deep cervical flexors ventrally crosses with weakness of the middle and lower trapezius. This pattern of imbalance creates joint dysfunction, particularly at the atlanto-occipital joint, C4-C5 segment, cervicothoracic joint, glenohumeral joint, and T4-T5 segment. Janda noted that these focal areas of stress within the spine correspond to transitional zones in which neighboring vertebrae change in morphology. Specific postural changes are seen in UCS, including forward head posture, increased cervical lordosis and thoracic kyphosis, elevated and protracted shoulders, and rotation or abduction and winging of the scapulae. These postural changes decrease glenohumeral stability as the glenoid fossa becomes more vertical due to serratus anterior weakness leading to abduction, rotation, and winging of the scapulae. This loss of stability requires the levator scapula and upper trapezius to increase activation to maintain glenohumeral centration[1].Exposure of the human body to gravity forces, e.g., when standing or walking, is necessary to ensure proper activity of the skeletal muscles responsible for maintaining good body posture. When these muscles are not stimulated to resist gravity for an extended period, e.g., during prolonged sitting or lying, their stabilizing function is disturbed by the hypoactivity reaction resulting in muscular weakness and atrophy. The deficit of the locomotor system stability triggers a compensatory mechanism—the stabilizing function is overtaken by the mobilizing muscles. However, as a side effect, such compensation leads to mobilizers’ increased activity (hyperactivity) and, subsequently, their decreased flexibility, which may finally lead to a pathological chain of reactions within the musculoskeletal system[2][3][4][5][6][7].
Mechanism of Injury / Pathological Process[edit | edit source]
According to Karel Lewit (1994), muscle imbalance usually occurs before functional dysfunction[8]. V Janda (2013), also describes this muscle imbalance as a condition in which some muscles become inhibit and weak and others become short and stiff. Such imbalance can bring changes in tissues, which may cause inappropriate movement patterns in the individual. Such conditions can eventually cause side effects such as pain and inflammation. Janda attributes these predicted patterns to a large extent, due to the immobile conditions and repetitive tasks[9][10]. Muscle balance can be defined as a relative equality of muscle length or strength between an agonist and an antagonist; this balance is necessary for normal movement and function[1].
In this syndrome, mainly the posterior superior muscles in the neck and the anterior neck, which are tonic, are short and the anterior deep muscles of the neck and posterior shoulder girdle, which are mainly phasic, are inhibited and weakened. This condition is caused by the changes in the elevation, protraction and abduction of the shoulder by increasing the angle of forward head and hyperextension of the upper part of the cervical spine, which are often associated with forward head, round shoulder, protracted scapulae, and thoracic kyphosis[9][10].These muscle imbalances and movement dysfunctions may have a direct effect on joint surfaces, thus potentiallyleading to joint degeneration. In some cases, joint degen-eration may be a direct source of pain, but the actual causeof pain has been often secondary to muscle imbalance[11].
Muscles may become unbalanced as a result of adaptation or dysfunction. Such muscle imbalances can be either functional or pathological:
- Functional muscle imbalances occur in response to adaptation for complex movement patterns, including imbalances in strength or flexibility of antagonistic muscle groups[1]. The structural approach focuses on actual damage to musculoskeletal structures such as rotator cuff tendonitis or a ligament injury. The functional approach examines factors that contribute to structural lesions. This approach is most useful for physical therapy management of chronic ‘dysfunctions’ such as persistent joint pain and tendonitis[12].
- When muscle imbalance impairs function, it is considered to be pathological. Pathological muscle imbalance typically is associated with dysfunction and pain, although its cause may or may not result from an initial traumatic event. Pathological imbalance may also be insidious; many people have these muscle imbalances without pain. Ultimately, however, pathological muscle imbalance leads to joint dysfunction and altered movement patterns, which in turn lead to pain. Note that this muscle imbalance continuum may progress in either direction; muscle imbalance may lead to altered movement patterns and vice versa. Some injuries cause muscle imbalance, while others may result from muscle imbalance.Sometimes pathological imbalances are a functional compensation for an injury[1].For example, unbalanced biomechanical joint stresses that result from muscle imbalance may lead to joint damage, setting up a vicious cycle of pain and inflammation. The structural inflammation then affects the neuromuscular system of the joint, creating further dysfunction. Eventually, the body adapts the motor program for movement to compensate for the dysfunction. The functional cause of the problem is muscle imbalance, while the symptom is pain and inflammation resulting from a structural lesion. Therefore, it is possible to have both a structural and a functional lesion, but for accurate diagnosis and treatment, the clinician must decide which lesion is the actual cause of dysfunction[1].
| Functional imbalance | Pathological imbalance |
|---|---|
| Atraumatic | With or without trauma |
| Adaptive change | Adaptive change |
| Activity specific | Associated with dysfunction |
| No pain | With or without pain |
Proprioceptive senses are the senses used to control the positions and motions of the trunk and parts of the body in space[13]. Proprioceptive senses related to the spatial recognition of the head require not only information from the vestibular organs and visual information, but also proprioceptive sense information from the cervical spine[14] Proprioceptive senses perform two important roles in the neck: they provide information on posture and motion of the cervical spine to the central nervous system, and they provide cervical reflexes for stability and protection of the cervical spine[15]. Pathology, injuries, muscle fatigue, and aging have been reported as causes of damage to cervical spine positional senses, and recent studies have reported that position sense declines in patients with damage to the cervical spine or who complain of pain[16][17].
Clinical Presentation[edit | edit source]
Individuals who present with upper crossed syndrome will show a forward head posture (FHP), hunching of the thoracic spine-as well as changed function in the shoulder girdle, elevated and protracted shoulders, scapular winging, and decreased mobility of the thoracic spine[18][19]. Ofen upper crossed syndrome is is associated with postural disorders and other dysfunction of upper body. Kendall et al. proposed a definition of good human posture: “good posture is that state of muscular and skeletal balance which protects the supporting structures of the body against the injury or progressive deformity, irrespective of the attitude (erect, lying, squatting or stooping) in which these structures are working or resting. Under such conditions, the muscles will function most efficiently, and the optimum positions are afforded for the thoracic and abdominal organs[20].
Weak muscles:
- Lower and middle trapezius
- Serratus anterior
- Infraspinatus
- Deep neck flexors
Tight muscles:
- Upper trapezius
- Pectorals,tightness of the pectoralis major creates an anterior force on the glenohumeral joint with a consequent decrease in stability[21].A tight pectoralis minor limits scapular upward rotation, external rotation, and posterior tilt, thereby reducing SAS[22].
- Levator scapulae [23]
Upper crossed syndrome summary according to NASM[24][edit | edit source]
| Short muscles | Lengthened muscles | Altered joints mechanics | Possible injuries |
|---|---|---|---|
| Upper trapezius | Deep cervical flexors | Increased: | Headaches |
| Levator scapulae | Serratus anterior | Cervical extention | Biceps tendonitis |
| Sternocleidomastoid | Rhomboids | Scapular protraction/elevation | Rotator cuff impingement |
| Scalenes | Mid-trapezius | Thoracic outlet syndrome | |
| Latissimus dorsi | Lower trapezius | Decreased: | |
| Teres minor | Teres minor | Shoulder extention | |
| Subscapularis | Infraspinatus | Shoulder external rotation | |
| Pectoralis major/minor |
Diagnostic Procedures[edit | edit source]
- In clinical practice, it is advisable to begin muscle evaluation by analyzing erect standing posture and gait. The c1inician is given an overall view of the patient's muscle function through posture and gait analysis and is challenged to look comprehensively at the patient's entire motor system and not to limit attention to the local level of the lesion[25].
- Muscle Analysis of Standing Posture:Posterior View/Anterior View/Lateral View[1].
- Evaluation of Balance[1].
- Hipermobility[1].
- Evaluation of muscle imbalance in a patient with an acute pain syndrome, however, is unreliable and must be undertaken with precaution. A precise evaluation of tight muscles and movement patterns can be performed only if the patient is pain-free or almost pain-free. Its usefulness is greatest in the chronic phase or in patients with recurrent pain after the acute episode has subsided[25].
Upper-Quarter Muscles[edit | edit source]
The muscles of the upper quarter include those of the cervical spine, shoulder, andarm. The muscles prone to tightness are those involved in a protective flexor response. Tightness of the upper trapezius, pectoral muscles, and suboccipitals in particular is a hallmark sign of Janda's UCS[1].
Upper trapezius m.is tested with the patient supine, with the head passively flexed and side-bent to the contralateral side. Once the slack is taken up, the shoulder girdle is pushed distally. Normally, a sort barrier is felt at the end of the push; however,when the movement is restricted, the barrier has an abrupt firm to hard end-reel[25].
Levator scapulae m. is examined in a similar manner, except that the head is also rotated to the contralateral side[25].
Deep posterior neck m. muscles can be tested only by thorough palpation. Evaluation of the sternocleidomastoid is not reliable because it crosses too many segments[25].
Pectoralis major m. is tested with the patient supine. The trunk must be stabilized before the arm is placed into abduction because a possible twist of the trunk might mimic the normal range of movement. The arm should reach the horizontal level. To estimate the clavicular portion, the arm is allowed to hang down loosely and the examiner applies a posterior glide to the shoulder. Normally, only a slight soft barrier is felt[25]. V.Janda had suggested testing pectoralis major muscule. The different portions of the pectoralis major are tested separately. The clinician is able to target the specific portions by changing the amount of shoulder abduction.
• Lower sternal fibers. The clinician abducts the patient's arm to 150° with slight external rotation. The normal length of these pectoral fibers allows the patient's arm to rest in a horizontal position; slight overpressure produces end-feel resistance. The clinician should also palpate the sternal fibers medial to the axilla for tenderness. Shortness or hypertonicity of the muscle is indicated by an inability of the arm to reach horizontal or a palpable tenderness in the muscle.
• Midsternal fibers. The clinician abducts the patient's arm to 90° and palpates the muscle fibers at the second rib interspace. The normal length of these fibers allows the patient's arm to rest below the horizontal. There is gradual end-feel resistance when the clinician applies slight overpressure. Palpation does not produce tenderness.
• Clavicular fibers. The clinician places the patient's arm in an extended position close to the body and allows the arm to come to a rest. The normal length of these fibers allows the patient's arm to rest below the horizontal. The clinician applies a gentle anteroposterior and caudal pressure through the glenohumeral joint as well as palpates the fibers just inferior to the clavicle. Resistance to this pressure should be gradual and fibers should not be tender to palpation[1].
Pectoralis Minor m. is tested swith the patient supine.The clinician views the mark on the patient from a superior view. The normal distance between the acromion and the table is 1 in. The horizontal levels of the anterior aspects of the acromions can be compared with each other. The two acromions should be on the same level; a higher acromion indicates possible pectoralis minor tightness[1].
Latissimus Dorsi m. is tested swith the patient supine. The clinician stands beside the arm being tested.The clinician passively elevates the patient's arm toward the head of the table. The normal length of the latissimus dorsi allows the arm to rest horizontally to the table with the lumbar spine flat on the table. Tightness of this muscle is indicated by the arm resting above horizontal or by the lumbar spine going into extension[1].
Janda's Basic Movement Patterns[edit | edit source]
Janda identified six basic movement patterns that provide overall information about a particular patient's movement quality and control; these movements form the basis of the hip extension, hip abduction, curl-up, cervical flexion, push-up, and shoulder abduction movement pattern tests.The clinician should observe both the left and right sides for comparison. Muscle or limb trembling during these tests is considered a positive finding, indicating weakness or fatigue. Some patients do not need to perform all six tests at once; the clinician should decide which tests are indicated based on the postural analysis and history[1].
Cervical Flexion Movement Pattern Test
Push-Up Movement Pattern Test
Shoulder Abduction Movement Pattern Test
Additional Movement Tests[edit | edit source]
Craniocervical Flexion Test
Breathing Patterns
The primary muscles responsible for respiration are the diaphragm, intercostals, scalenes, TrA, pelvic floor muscles, and deep intrinsic spinal muscles. Each of these muscles plays a role in both respiration and spinal stabilization. According to Kendall, McCreary, and Provance, of the 20 primary and accessory muscles associated with respiration, almost all of them have a postural function. Some patients may show relatively normal respiratory patterns when relaxed in a supine position but may change into accessory-muscle or chest breathers when challenged in a functional position such as sitting at a computer or standing erect. Thus respiration patterns should be assessed with the patient in various positions, especially any painful positions used in ADL. A simple test is for the clinician to gently rest her hands on the patient's shoulders during quiet breathing to note any upward movement of the shoulders that would indicate accessory respiration (figure 6.9). There are several things to observe in assessing respiration:
- Initiation of breath—the initiation of breathing should be at the abdominal region and not the chest.
- Lateral excursion of the lower rib cage during inspiration—movement of the rib cage is best assessed with the patient in the seated or standing position.
- Upper-chest expansion during the final phase of inspiration—the most common faulty pattern is the superior or cranial excursion, or lifting of the upper ribs by the scalenes and upper trapezius to substitute for inefficient or inhibited diaphragm activity[1].
Hence, for the assessment of UCS, the alignment and its side effects are often evaluated, such as increase in thoracic kyphosis or forward head angles, while less attention has been paid to the keystone, i.e., the scapulae, and the relevant altered muscle activation and movement patterns[31]. In this regard, many researchers and therapists have only evaluated one of the affected regions, such as head, shoulders, or spine, separately and reported a degree of postural deviation regardless of other relevant malalignments and patterns of the muscle activation and related movement patterns, such as scapulohumeral rhythm or neck flexion[32]
Outcome Measures[edit | edit source]
Shoulder pain and Disability Index (SPADI)[33]
SF-36 questionnaire[35]
McGill-Melzack Pain Questionnaire[35]
Visual analogue scale (VAS)[11]
Management / Interventions[edit | edit source]
Over recent decades, therapists have been seeking to design appropriate exercises to correct musculoskeletal malalignments mainly through structural and functional approaches[36][37][38].In the traditional structural approach, the changes observed in malalignments such as in UCS are attributed to biomechanics and are presumed to lead to adjustments in the length and strength of local muscles[36][37].This may account for the stretching of short muscles and strengthening of weakened muscles at the site of the problem in the correction phase, while ignoring other related malalignments[39].Interestingly, despite the popularity of this method, very little research has been conducted based on this theory[40]. Furthermore, some review studies have questioned the effectiveness of strengthening and stretching exercises to improve postural disorders[41].
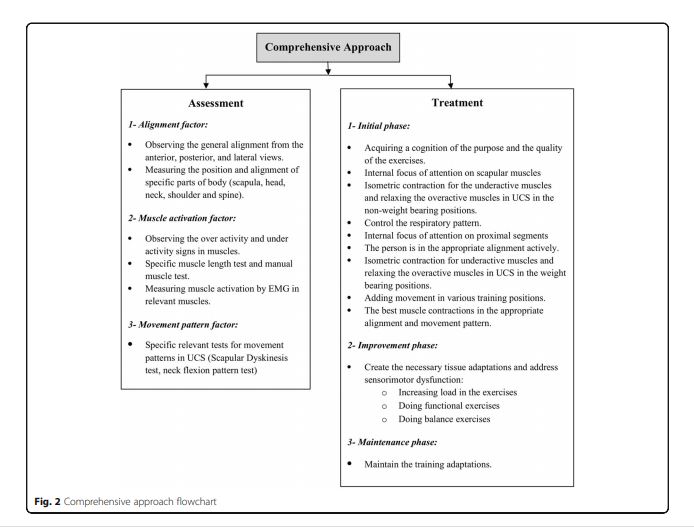
In contrast, the functional (neurological) approach to musculoskeletal problems is based on the interaction of the central and peripheral nervous systems, and the involvement of the muscular and skeletal structures in producing and controlling motion[42]. In this functional approach, the musculoskeletal problems are attributed to the role of muscles in motor function; furthermore, changes in the alignment result not only from changes in muscle length and strength but also from more important changes in muscle neuromuscular factors, such as muscle recruitments[38].In fact, the motor control unit may change the muscle activation strategy for temporary stabilization due to the presence of dysfunction. These changes in motor recruitment will alter the muscular balance, movement patterns, and eventually the motor program[37]. Similarly, Hodges et al. noted that motor control interventions require tailoring to each individual’s posture, muscle activation, and movement pattern[43].
There have been some studies showing effective exercise programmes for people with UCS,and one of these is Comprehensive corrective exercise program (CCEP)[44], Below is the list of exercises used in the CCEP:
Each exercise session begins with 10 min of warm-up activity and ends with 5 min of cool-down. Selected exercises are designed in three phases: initial, improvement, and maintenance.
The initial phase exercises include laying supine on a foam roll in three different arm abduction angles (exercise 1A–C), side-lying external rotation (exercise 2), side-lying forward flexion (exercise 3), standing diagonal flexion (exercise 4), and military press (exercise 5). Participants with less ability can do exercises 4 and 5 in a sitting position. Once a participant regains muscle balance in the static conditions, he will try to add upper extremity movements in exercise positions. Exercises progress in frequency and intensity during this phase, as long as participants are able to demonstrate good quality movement. The initial phase duration is 2 weeks and the exercises will be performed for seven sets of 10-s hold to ten sets of 15-s hold.
Janda firmly believed that the CNS and motor system function as one unit, the sensorimotor system. He suggested treatment be organized into three stages:
Normalization of the peripheral structures. All peripheral structures outside the CNS must be treated in order to improve the quality of afferent information being received by the CNS.
a) Central Indirect Technique: Vojta approach, primal reflex release technique (PRRT), and Feldenkrais.
b) Local Direct Techniques: soft-tissue techniques, neural tension techniques and neurodynamics, joint mobility techniques and others.
2. Restoration of muscle balance. The balance between the phasic and tonic muscle systems must be improved as a prerequisite for improving coordination.
3. Facilitation of afferent system and sensory motor training. This training improves movement coordination and therefore promotes ideal mechanical loading of biological structures and efficient motor execution.
Science-based evidence
- Apoorva Phadke et al. in the study has conluded muscle energy technique was better than stretching technique in improving pain and functional disability in people with mechanical neck pain[45].
- Rasoul Arshadi et al. in the study has conluded eight week corrective exercises balance muscles activity and can be used to manage developing upper quadrant musculoskeletal disorders in person with UCS [46].
Differential Diagnosis[edit | edit source]
Scheuermann's Disease
Stress and anxiety
Pseudoradicular syndrome
Scalene syndrome
Resources[edit | edit source]
add appropriate resources here
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 Page P, Frank C.C, Lardner R. Assessment and treatment of muscle imbalance: The Janda Approach 2010, Champaign, IL: Human Kinetics.
- ↑ Sahrmann S. Diagnosis and treatment of movement impairment syndromes. St. Louis: Mosby; 2002
- ↑ Richardson CA, Hodges PW, Hides J. Therapeutic exercise for lumbopelvic stabilization: a motor control approach for the treatment and prevention of low back pain. 2. Edinburgh: Churchill Livingstone; 2004.
- ↑ Richardson C. The muscle designation debate: the experts respond. J Bodyw Mov Ther. 2000;4(4):235–236.
- ↑ Hides J.A, Belavý D.L, Stanton W, Wilson S.J, Rittweger J, Felsenberg D, Richardson CA. Magnetic resonance imaging assessment of trunk muscles during prolonged bed rest. Spine (Phila Pa 1976). 2007 Jul 1; 32(15):1687-92.
- ↑ Hides JA, Lambrecht G, Richardson CA, Stanton WR, Armbrecht G, Pruett C, Damann V, Felsenberg D, Belavý DL.The effects of rehabilitation on the muscles of the trunk following prolonged bed rest.Eur Spine J. 2011 May; 20(5):808-18.
- ↑ Belavý DL, Richardson CA, Wilson SJ, Rittweger J, Felsenberg D.Superficial lumbopelvic muscle overactivity and decreased cocontraction after 8 weeks of bed rest.Spine (Phila Pa 1976). 2007 Jan 1; 32(1):E23-9.
- ↑ Lewit K. The functional approach. Orthop J Sports Med. 1994;16(3):73-4
- ↑ 9.0 9.1 Moore MK. Upper crossed syndrome and its relationship to cervicogenic headache. J Manipulative Physiol Ther. 2004; 27(6):414-20
- ↑ 10.0 10.1 Janda V. Muscle function testing. Elsevier; 2013; 230-58
- ↑ 11.0 11.1 Phadke A,Bedekar N et al. Effect of muscle energy technique and static stretching on pain and functional disability in patients with mechanical neck pain: A randomized controlled trial. Hong Kong Physiotherapy Journal Volume 35, December 2016, Pages 5-11
- ↑ Page P. Shoulder muscle imbalance and subacromial impingement syndrome in overhead athletes.Int J Sports Phys Ther. 2011 Mar; 6(1): 51–58.
- ↑ Janda V: Muscles and motor control in cervicogenic disorders. New York: Churchill Livingstone, 1994
- ↑ Repositioning error in low back pain. Comparing trunk repositioning error in subjects with chronic low back pain and control subjects. Newcomer K, Laskowski ER, Yu B, Larson DR, An KN Spine (Phila Pa 1976). 2000 Jan 15; 25(2):245-50.
- ↑ Hogervorst T, Brand RA J Mechanoreceptors in joint function. Bone Joint Surg Am. 1998 Sep; 80(9):1365-78.
- ↑ Pinsault N, Vuillerme N, Pavan P.Cervicocephalic relocation test to the neutral head position: assessment in bilateral labyrinthine-defective and chronic, nontraumatic neck pain patients. Arch Phys Med Rehabil. 2008 Dec; 89(12):2375-8.
- ↑ Haldeman S: Principles and practices of chiropractic. 3rd ed. USA: Appleton & Lange, 2004
- ↑ Public Education Section Department of Business and Consumer Business Oregon OSHA.Introduction to the Ergonomics of Manual Material Handling. Diunduhdari: Diakses Tanggal Maret; 2012.
- ↑ Page P, Frank C.C, Lardner R. Assessment andtreatment of muscle imbalance: The Janda Approach 2010, Champaign, IL: Human Kinetics.
- ↑ Kendall F, McCreary E, Provance PG, Rodgers M, Romani WA. Muscle testing and function with posture and pain. Baltimore: Lippincott Williams & Wilkins; 2005
- ↑ Labriola J.E.et al. , Stability and instability of the glenohumeral joint: the role of shoulder muscles. J Shoulder Elbow Surg. 2005;14(1 Suppl S):32S–38S
- ↑ Borstad J.D.Ludewig P.M., The effect of long versus short pectoralis minor resting length on scapular kinematics in healthy individuals. J Orthop Sports Phys Ther. 2005;35(4):227–238
- ↑ Page P. Shoulder muscle imbalance and subacromial impingement syndrome in overhead athletes.Int J Sports Phys Ther. 2011 Mar; 6(1): 51–58.
- ↑ NASM https://www.nasm.org/docs/PDF/nasm-cpt-website-exam_study_final.pdf
- ↑ 25.0 25.1 25.2 25.3 25.4 25.5 Liebenson C. Rehabilitation of the Spine: A Practitioner's Manual. Lippincott Williams & Wilkins Philadelphia, Pennsylvania: 2007
- ↑ ThinkStrong. Muscle Tightness - What Causes Muscle Tightness?Available from: https://www.youtube.com/watch?v=hJmeunUXndQ [last accessed 5/5/2020]
- ↑ Ccedseminars. Janda Cervical Flexion Movement Pattern Test. Available from: https://www.youtube.com/watch?v=aOYkX6g4Cjw [last accessed 26/4/2020]
- ↑ Ccedseminars. Janda Push up Movement Pattern Test. Available from: https://www.youtube.com/watch?v=2LwbBmkosos [last accessed 26/4/2020]
- ↑ Ccedseminars. Janda Shoulder Abduction Movement Pattern Test. Available from: https://www.youtube.com/watch?v=O-txyuVDJ1s [last accessed 26/4/2020]
- ↑ BU PT623: MS III Spine Lab. Cranial Cervical Flexion Test Available from: https://www.youtube.com/watch?v=bkb6XjvS0aU [last accessed 5/5/2020]
- ↑ Bae WS, Lee HO, Shin JW, Lee KC. The effect of middle and lower trapezius strength exercises and levator scapulae and upper trapezius stretching exercises in upper crossed syndrome. J Phys Ther Sci. 2016;28(5):1636–9
- ↑ Vaughn DW, Brown EW. The influence of an in-home based therapeutic exercise program on thoracic kyphosis angles. J Back Musculoskelet Rehabil. 2007;20(4):155–65
- ↑ Sneha J, Namrata S. To Compare the Effectiveness of Active Release Technique and Conventional Physical Therapy in the Management of Upper Cross Syndrome.Indian Journal of Physiotherapy & Occupational Therapy . Oct-Dec2018, Vol. 12 Issue 4, p51-54. 4p.
- ↑ Salvatori R, Rowe RH, Osborne R, Beneciuk JM.Use of thoracic spine thrust manipulation for neck pain and headache in a patient following multiple-level anterior cervical discectomy and fusion: a case report.J Orthop Sports Phys Ther. 2014 Jun;44(6):440-9. doi: 10.2519/jospt.2014.5026. Epub 2014 May 10.
- ↑ 35.0 35.1 M. S., İnce; R., Gözil; H., Demirköse; G., Aytaç. Evaluation of the frequency of "upper cross syndrome" among the medicine students. International Journal of Experimental & Clinical Anatomy . Aug2019, Vol. 13 Issue Supplement2, pS122-S122. 1/3p.
- ↑ 36.0 36.1 Czaprowski D, Stoliński Ł, Tyrakowski M, Kozinoga M, Kotwicki T. Nonstructural misalignments of body posture in the sagittal plane. Scoliosis Spinal Disord. 2018;13(1):6.
- ↑ 37.0 37.1 37.2 Page P. Sensorimotor training: a “global” approach for balance training. J Bodyw Mov Ther. 2006;10(1):77–84.
- ↑ 38.0 38.1 Frank C, Kobesova A, Kolar P. Dynamic neuromuscular stabilization & sports rehabilitation. Int J Sports Phys Ther. 2013;8(1):62
- ↑ Sahrmann S, Azevedo DC, Van Dillen L. Diagnosis and treatment of movement system impairment syndromes. Braz J Phys Ther. 2017;21(6):391–9
- ↑ Seidi F, Rajabi R, Ebrahimi I, Alizadeh MH, Minoonejad H. The efficiency of corrective exercise interventions on thoracic hyper-kyphosis angle. J Back Musculoskelet Rehabil. 2014;27(1):7–16
- ↑ Hrysomallis C. Effectiveness of strengthening and stretching exercises for the postural correction of abducted scapulae: a review. J Strength Cond Res. 2010;24(2):567–74
- ↑ Hamill J, van Emmerik RE, Heiderscheit BC, Li L. A dynamical systems approach to lower extremity running injuries. Clin Biomech. 1999;14(5):297–308.
- ↑ Hodges P, Paul W, Van Dieën JH, Cholewicki J. Time to reflect on the role of motor control in low back pain. Alexandria: JOSPT Inc.; 2019.
- ↑ Bayattork, M., Seidi, F., Minoonejad, H. et al. The effectiveness of a comprehensive corrective exercises program and subsequent detraining on alignment, muscle activation, and movement pattern in men with upper crossed syndrome: protocol for a parallel-group randomized controlled trial. Trials 21, 255 (2020). https://doi.org/10.1186/s13063-020-4159-9
- ↑ Phadke A et al.Effect of muscle energy technique and static stretching on pain and functional disability in patients with mechanical neck pain: A randomized controlled trial. Hong Kong Physiotherapy Journal Volume 35, December 2016, Pages 5-11
- ↑ Arshadi R. Effects of an 8-week selective corrective exercises program on electromyography activity of scapular and neck muscles in persons with upper crossed syndrome: Randomized controlled trial. Physical Therapy in Sport Volume 37, May 2019, Pages 113-119