Understanding Red Flags in Patellofemoral Pain: Difference between revisions
Carin Hunter (talk | contribs) No edit summary |
Carin Hunter (talk | contribs) No edit summary |
||
| Line 154: | Line 154: | ||
== Assessment Tools == | == Assessment Tools == | ||
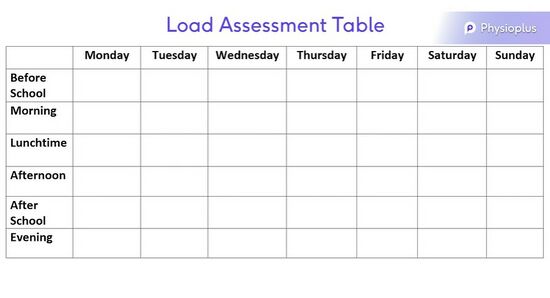
When advising an individual to modify their activity levels, it is advisable to print out a table, as pictured below, for them to accurately track their volume of exercise in a week. Be sure to encourage them to fill out the form accurately as this will be the best way to offer advice. It is also advisable to correctly record the length of time spent on each activity and the intensity of the activity. | |||
See a Load Assessment Table for Growth Tracking pictured below.[[File:Load Assessment Table.jpg|alt=|center|frameless|550x550px|link=https://www.physio-pedia.com/File:Load_Assessment_Table.jpg]] | |||
== References == | == References == | ||
[[Category:Course Pages]] | [[Category:Course Pages]] | ||
Revision as of 13:58, 29 August 2022
Top Contributors - Carin Hunter, Jess Bell and Kim Jackson
Introduction[edit | edit source]
Red flags are an important aspect of our assessments, but this often is overlooked in a patient with knee pain.
We need to know what might be a red flag for patient safety and for correct referral to the appropriate place. If there has been any trauma to the knee it is advisable to make sure the correct investigations have been carried out. This could mean imaging or special tests.
For more information on red flags please see Red Flags.
Non-Traumatic Masquerading Conditions[edit | edit source]
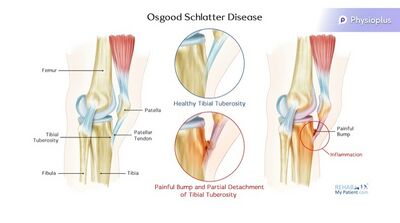
Osgood Schlatters[edit | edit source]
Signs and Symptoms:
- This condition is common in the 11-15 year old age group.[1]
- It is prevalent in children participating in quadricep dominant sports, ie running, kicking and jumping[1]
- It presents with an obvious bump at the tibial tubercle[2]
- Pain is specific to tibial tubercle
- Inflammation and elevation of the growth plates are present in the tibial tuberosity
- An MRI to show level of inflammation can be used as confirmation but this will not change treatment plan
- Pain can worsen to a point that it can prevent any participation in sport if left untreated
Treatment:
- Education
- Activity modification[1][2] - Try to eliminate the patients least favourite sport or change the playing position to a less active one to decrease load
- NSAIDS (Non-steroidal Anti-inflammatories)
- Ice Massage - This will provide symptomatic relief
- Address overload
For more information, please see Osgood-Schlatters Disease
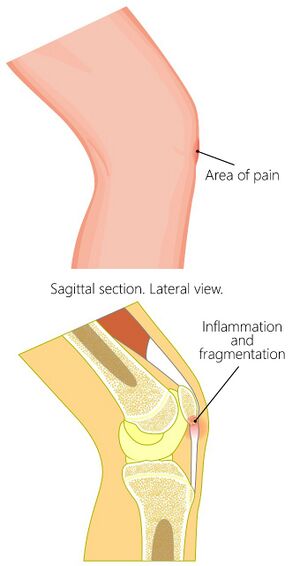
Sinding-Larsen-Johansson Disease[edit | edit source]
Sinding Larsen Johansson Syndrome (SLJS) is a juvenile osteochondrosis and traction epiphysitis affecting the extensor mechanism of the knee which disturbs the patella tendon attachment to the inferior pole of the patella. The tenderness of the inferior pole of the patella is usually accompanied by X-ray evidence of splintering of that pole. Most patients with SLJS also show a calcification at the inferior pole of the patella.[5]
The syndrome usually appears in adolescence, during the growth spurt. It’s associated with localised pain which is worsened by exercise. Usually a localised tenderness and soft tissue swelling is observed. There is also a tightness of the surrounding muscles, the quadriceps, hamstrings and gastrocnemius in particular. This tightness usually results in inflexibilities of the knee joint, altering the stress through the patellofemoral joint.[6]
Signs and Symptoms:
- Inflammation at the growth plate of the distal pole of the patella[7]
- This condition is most likely to be seen during growth spurts
- Primary treatment tactics track growth for activity modification during a growth spurt[8]
- Pain can worsen to a point that it can prevent any participation in sport
Treatment:
- Education
- Activity modification - Try to eliminate the patients least favourite sport or change the playing position to a less active one to decrease load
- NSAIDS (Non-steroidal Anti-inflammatories)
- Ice Massage - This will provide symptomatic relief
- Address overload
- Extrinsic factors
- Load management of sport
- Footwear
- Landing technique
- Intrinsic factors
- Muscle length
- Muscle strength
- Extrinsic factors
For more information, please see Sinding-Larsen-Johansson Disease
Knee Effusion[edit | edit source]
There is no situation where a child should have a knee effusion without a cause. This should therefore always be investigated. A knee effusion can often lead to patellofemoral pain.
Possible Effusion Causes:
- Systemic autoimmune disease (eg. juvenile arthritis)
- Infective arthritis
- Osteochondritis Dissecans
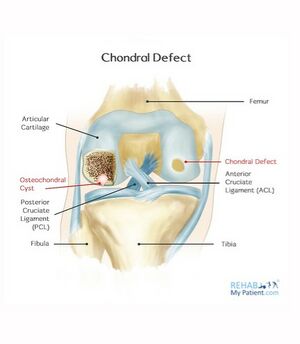
Osteochondritis Dissecans/Osteochondral Defect[edit | edit source]
Osteochondritis Dissecans (OCD) is defined as an inflammatory pathology of bone and cartilage. This can result in localized necrosis and fragmentation of bone and cartilage. [9] Cartilage and subchondral bone can break off and float in the joint. This irritates the synovium, which causes an effusion.
Osteochondritis Dissecans Treatment:
- Manage conservatively for stable lesions[10]
- Possible debridement/knee wash out
- Possible surgical resection (resect back to a stable margin)
- Review the osteochondral defects with an MRI[11]. Check for stability of the margins of the osteochondral defect and if the location is a weight-bearing zone.
- Monitor bone oedema around a defect. This should decrease when serially monitored.
- Physiotherapy advice: Load management
- With a trochlear osteochondral defect, in the patellofemoral joint, avoid excessive deep loaded flexion
Autoimmune Disease Red Flags:
- Multiple joint involvement
- Joint was stiff on waking
- Fatigue
Infective Arthritis Red Flags:
- Temperature
- Recent Illness
For more information, please see Osteochondritis Dissecans and Osteochondritis Dissecans of the Knee
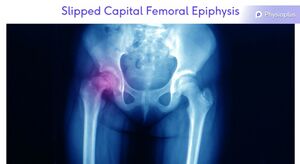
Slipped Capital Femoral Epiphysis[edit | edit source]
Slipped capital femoral epiphysis is not common but needs to be considered as a differential diagnosis[12]. This condition has been known to refer to the anteromedial knee. A mild condition, with an early diagnosis has a better outcome as the condition will progress until the epiphysis is fused.[12]
For more information, please see Slipped Capital Femoral Epiphysis
Others[edit | edit source]
Less common but more serious:
- Systemic Auto-Immune Disease
- Slipped Epiphysis
- FAI
- Leukaemia
- Metastatic Neuroblastoma
- Primary Bone Tumour
- Red Flags
- Night pain
- Weight loss
- Malaise
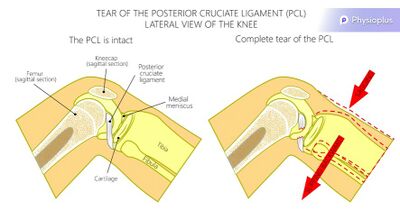
Posterior Cruciate Ligament Rupture[edit | edit source]
A rupture of the posterior cruciate ligament can be caused by a blow to the front of the knee[13]. This can present with the only patient reported symptom being patellofemoral join pain. It is advised to assess all ligaments to see if surgery is necessary[13]. Physiotherapy will often focus on Quadriceps rehabilitation.
For more information, please see PCL
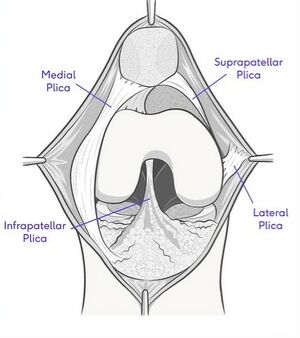
Synovial Plica[edit | edit source]
A plica is a fold in the synovial membrane. They are common and are normally asymptomatic. A plica can often be palpated anteromedially, next to the superior half of the patella. Occasionally, they can get trapped into the patellofemoral joint, and can become impinged or inflamed and sore[14].
Diagnosis:
- Inject with local anaesthetic for symptomatic relief. If this is successful, it is a strong indication of an inflamed synovial plica.
Treatment:
- Steroid injections to decrease inflammation
- Plica resection
- Rehabilitation[14]
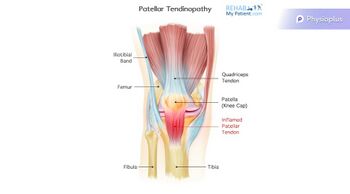
Patella Tendinopathy[edit | edit source]
Tendinopathy is a failed healing response of the tendon, with haphazard proliferation of tenocytes, intracellular abnormalities in tenocytes, disruption of collagen fibers, and a subsequent increase in noncollagenous matrix.[15][16][17] The term tendinopathy is a generic descriptor of the clinical conditions ( both pain and pathological characteristics) associated with overuse in and around tendons.[18]
Treatment:
- Heavy resistance loading
- Eccentric[19] decline loading
| Patella Tendinopathy | Patellofemoral Pain | |
|---|---|---|
| Aggravating Factors | Being still[20]
Early morning |
Being still if knee at end of range flexion |
| Description of Pain | Pinpoint to proximal tendon[20] | Vague |
| Effect of Excercise | Pain decreases as tendon warms up[20] | Worsens with repetitive load |
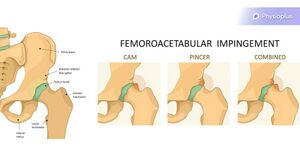
Femoroacetabular Impingement[edit | edit source]
While femeroacetabular impingement is not common, it has been known to refer pain to the anteromedial knee. This can sometimes be confused with patellofemoral pain. One quick test that can be performed is the Quadrant Test. This involves flexion, adduction, internal rotation[21] of this hip. A positive test would be that the knee pain is replicated.
For more information, please see Femoroacetabular Impingement
Assessment Tools[edit | edit source]
When advising an individual to modify their activity levels, it is advisable to print out a table, as pictured below, for them to accurately track their volume of exercise in a week. Be sure to encourage them to fill out the form accurately as this will be the best way to offer advice. It is also advisable to correctly record the length of time spent on each activity and the intensity of the activity.
See a Load Assessment Table for Growth Tracking pictured below.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Neuhaus C, Appenzeller-Herzog C, Faude O. A systematic review on conservative treatment options for OSGOOD-Schlatter disease. Physical Therapy in Sport. 2021 May 1;49:178-87.
- ↑ 2.0 2.1 Corbi F, Matas S, Álvarez-Herms J, Sitko S, Baiget E, Reverter-Masia J, López-Laval I. Osgood-Schlatter Disease: Appearance, Diagnosis and Treatment: A Narrative Review. InHealthcare 2022 May 30 (Vol. 10, No. 6, p. 1011). MDPI.
- ↑ O’Sullivan IC, Crossley KM, Kamper SJ, van Middelkoop M, Vicenzino B, Franettovich Smith MM, Menz HB, Smith AJ, Tucker K, O’Leary KT, Costa N. HAPPi Kneecaps! A double-blind, randomised, parallel group superiority trial investigating the effects of sHoe inserts for adolescents with patellofemoral PaIn: phase II feasibility study. Journal of Foot and Ankle Research. 2021 Dec;14(1):1-1.
- ↑ Gaulrapp H, Nührenbörger C. The Osgood-Schlatter disease: A large clinical series with evaluation of risk factors, natural course, and outcomes. International Orthopaedics. 2022 Feb;46(2):197-204.
- ↑ Medlar RC, Lyne ED. Sinding-Larsen-Johansson disease. Its etiology and natural history. The Journal of Bone and Joint surgery. American Volume. 1978 Dec 1;60(8):1113-6.
- ↑ Houghton, K. M., ‘Review for the generalist: evaluation of anterior knee pain’, Paediatric Rheumatology, (2007), vol. 5, p. 4-10.
- ↑ Fischer AN. Sinding-Larsen-Johansson Syndrome. InCommon Pediatric Knee Injuries 2021 (pp. 63-68). Springer, Cham.
- ↑ McCormick KL, Tedesco LJ, Bixby EC, Swindell HW, Popkin CA, Redler LH. Sinding-Larsen-Johansson Disease: Analysis of the Associated Factors in the Largest Cohort to Date. Orthopaedic Journal of Sports Medicine. 2022 May 31;10(5_suppl2):2325967121S00503.
- ↑ Osteochondritis Dissecans of the Elbow
- ↑ Chau MM, Klimstra MA, Wise KL, Ellermann JM, Tóth F, Carlson CS, Nelson BJ, Tompkins MA. Osteochondritis dissecans: current understanding of epidemiology, etiology, management, and outcomes. JBJS. 2021 Jun 16;103(12):1132-51.
- ↑ Detterline AJ, Goldstein JL, Rue JP, Bach BR. Evaluation and treatment of osteochondritis dissecans lesions of the knee. Journal of Knee Surgery. 2008;21(02):106-15.
- ↑ 12.0 12.1 Purcell M, Reeves R, Mayfield M. Examining delays in diagnosis for slipped capital femoral epiphysis from a health disparities perspective. Plos one. 2022 Jun 24;17(6):e0269745.
- ↑ 13.0 13.1 Perelli S, Masferrer-Pino Á, Morales-Ávalos R, Fernández DB, Ruiz AE, Gallego JT, Idiart R, Fabregat ÁA, Alcaraz10 NU. Current management of posterior cruciate ligament rupture. A narrative review. Rev Esp Artrosc Cir Articul. 2021;28(3):180-91.
- ↑ 14.0 14.1 Casadei K, Kiel J. Plica syndrome. StatPearls [Internet]. 2021 Jul 25.
- ↑ Maffulli N, Longo UG, Franceschi F, Rabitti C, Denaro V. Movin and Bonar scores assess the same characteristics of tendon histology. Clinical orthopaedics and related research. 2008 Jul;466(7):1605-11.
- ↑ Maffulli N, Longo UG, Maffulli GD, Rabitti C, Khanna A, Denaro V. Marked pathological changes proximal and distal to the site of rupture in acute Achilles tendon ruptures. Knee Surgery, Sports Traumatology, Arthroscopy. 2011 Apr;19(4):680-7.
- ↑ Alexander L, Shim J, Harrison I, Moss R, Greig L, Pavlova A, Parkinson E, Maclean C, Morrissey D, Swinton P, Brandie D. Exercise therapy for tendinopathy: a scoping review mapping interventions and outcomes.
- ↑ Maffulli N. Overuse tendon conditions: time to change a confusing terminology. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 1998 Nov 1;14(8):840-3.
- ↑ Challoumas D, Pedret C, Biddle M, Ng NY, Kirwan P, Cooper B, Nicholas P, Wilson S, Clifford C, Millar NL. Management of patellar tendinopathy: a systematic review and network meta-analysis of randomised studies. BMJ open sport & exercise medicine. 2021 Nov 1;7(4):e001110.
- ↑ 20.0 20.1 20.2 Rosen AB, Wellsandt E, Nicola M, Tao MA. Current clinical concepts: clinical management of patellar tendinopathy. Journal of Athletic Training. 2021 Oct 1.
- ↑ Hale RF, Melugin HP, Zhou J, LaPrade MD, Bernard C, Leland D, Levy BA, Krych AJ. Incidence of femoroacetabular impingement and surgical management trends over time. The American journal of sports medicine. 2021 Jan;49(1):35-41.