Spina Bifida: Difference between revisions
No edit summary |
No edit summary |
||
| Line 45: | Line 45: | ||
*Trunk hypotonia | *Trunk hypotonia | ||
*Delayed automatic postural reactions <ref name="Path" /> | *Delayed automatic postural reactions <ref name="Path" /> | ||
===Signs and Symptoms=== | |||
Children with Spina Bifida can have a variety of symptoms which can vary from mild to severe. The main symptoms include: | |||
*Cognitive symptoms - As spina bifida occurs due to problems with the developing spine and spinal cord, this can have an associated effect on development of the brain. Specifically areas of the brain involved in memory, learning, as well as concentration, understanding and the processing of language. Children may have difficulty with complex motor tasks such as tying laces where good visual and physical coordination is required <ref>BARF, H.A., VERHOEF, M., JENNEKENS-SCHINKEL, A., POST, M.W.M., GOOSHKENS, R.H.J.M. & PREVE, A.J.H., 2003. Cognitive status of young adults with spina bifida. Dev Med Child Neurol. Vol. 45, pp. 813-20.</ref>.6 out of 10 children born with spina bifida will have normal intelligence levels, although around half of these will have some form of learning disability <ref>HINDERER, K.A., HINDERER, S.R. & SHURTLEFF, D.B., 2006. Myelodysplasia. In CAMPBELL, S.K., VANDER LINDEN, D.W. & PALISANO, R.J. Physical Therapy for Children. 3rd edition. Pp. 735-789. Philadelphia: Saunders Elsevier</ref>. | |||
*Mobility Symptoms - The spinal cord allows information to travel up and down to brain in order to control movements made by muscles and joints. As the spinal cord and nerves can be compromised in certain types of Spina Bifida, there are often problems with muscle control and joint movement. In some cases, there may be paralysis of certain muscles which can result in the development of misshapen bones, particularly the feet, and abormal curving of the spine known as Scoliosis <ref name="PARK">PARK BROWN, J., 2001. Orthopaedic care of children with Spina Bifida: You’ve come a long way, baby! Orthopaedic Nursing. Vol. 20 (4), pp. 51-58</ref>. Those with severe mobility restrictions may also develop thin bones or osteoporosis due to the lack of use of the limbs <ref>AUSILI, E., FOCARELLI, B., TABACCO, F., FORTUNELLI, G., CARADONNA., P., MASSIMI, L., SIGISMONDI, M., SALVAGGIO, E. & RENDELI,C., 2008. Bone mineral density and body composition in a myelomeningocoele children population: effects of walking ability and sport activity. European Review for Medical and Pharmacological Sciences. Vol. 12, pp. 349-354</ref>. The spinal cord and nerves also provide the brain with sensory information through touch. As the spinal nerves can be daged in some forms of Spina Bifida, there may be associated loss of sensation and feeling in the pelvic region and legs. This can cause problems with pressure sores and skin breakdown in infants who are unable to feel the need to change position <ref name="TAPPIT">TAPPIT-EMAS, E., 2008. Spina Bifida. In J.S, TECKLIN, 4TH eds. Pediatric Physical Therapy. Phyiladelphia: Wolters Kluwer & Lippincott Williams and Wilkins, pp. 231-280</ref> | |||
*Incontinence (Urinary and Bowel) - The nerves travelling through the spinal cord also supply the bladder and bowel, ensuring the muscles within these organs can contract to contain urine and stools within the body. As a result, most children born with Spina Bifida will experience some degree of urinary and bowel incontinence <ref name="SAND">SANDLER., A.D., 2010. Children with Spina Bifida: Key Clinical Issues. Pediatr Clin N Am. Vol. 57, pp. 879-892.</ref> | |||
== Associated Co-morbidities == | == Associated Co-morbidities == | ||
| Line 59: | Line 67: | ||
*Decubitis Ulcer: these occur due to the altered sensation an individual may experience from the neurological deficit <ref name="Odd" /> | *Decubitis Ulcer: these occur due to the altered sensation an individual may experience from the neurological deficit <ref name="Odd" /> | ||
===Medical Management=== | |||
Medical management of the newly born child with Spina Bifida varies according to the severity of their condition. Those with Spina Bifida Occulta do not ususally require any specific treatment. Some people with Spina Bifida Occulta do not exhibit any symptoms and may only discover they have the condition when they are older after having an XRAY. Children born with myelocoele or myelomeningocoele will require surgery normally within 2-3 days of birth in order to close the gap in the spine and return the spinal cord and nerves to their original place within the spinal column <ref name="TAPPIT2">TAPPIT-EMAS, E., 2008. Spina Bifida. In J.S, TECKLIN, 4TH eds. Pediatric Physical Therapy. Phyiladelphia: Wolters Kluwer & Lippincott Williams and Wilkins, pp. 231-280</ref>. This aims to prevent infection and further damage to the exposed spinal cord and spinal nerves. Following surgery, the child will be monitored closely for signs of common pos-operative problems associated with this type of surgery, namely hydrocephalus and leaking of cerebrospinal fluid <ref name="SAND2">SANDLER., A.D., 2010. Children with Spina Bifida: Key Clinical Issues. Pediatr Clin N Am. Vol. 57, pp. 879-892.</ref> | |||
As the infant gets older, management of incontinence will be an important role of the medical team. Effective management strategies include the use of Clean Intermittent Catheterisation (CIC) and certain drugs which can increase the storage volume of the bladder <ref>LAPIDES, J., DIOKNO, A.C., SILBER, S.J., ET AL 1972. Clean, intermittent self-catheterisation in the treatment of urinary tract disease. J Urol. Vol. 107, pp. 458-61.</ref>. Children can also develop constipation due to lack of bowel movements and will require the development of a bowel programme which may involve assisted evacuation of stools. However, this will be based on an individualised assessment of the child and may involve educating the family in order to ensure the programme is effectively integrated into the child’s daily routine <ref>LEIBOLD, S., 2008. Neurogenic bowel and continence programmes for the individual with spina bifida. J Pediatr Rehabil Med. Vol. 1, pp. 325-36</ref> Effective strategies in managing incontinence in children with spina bifida are extremely important in allowing them to socially integrate themselves as they get older and attend school <ref name="SAND2" />. | |||
== Medications == | == Medications == | ||
Revision as of 13:02, 3 August 2020
Original Editors -Ally O'Bryan & Stephanie Smith from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Stephanie Smith, Allison O'Bryan, Shaimaa Eldib, Nikhil Benhur Abburi, Kim Jackson, Admin, Elaine Lonnemann, Wendy Walker, Naomi O'Reilly, Garima Gedamkar, Rucha Gadgil, Aminat Abolade, Vidya Acharya, WikiSysop, Meaghan Rieke, 127.0.0.1 and Aya Alhindi
Definition/Description[edit | edit source]
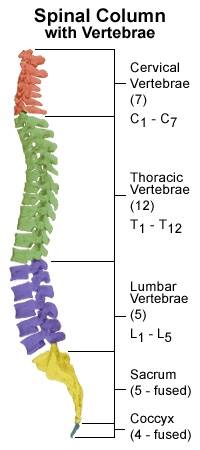
Spina Bifida, in general, is defined as "a neural tube defect (NTD) that results when the inferior neuropore does not close, although it has also been suggested that a closed tube may reopen in some cases.[1] Developing vertebrae do not close around an incomplete neural tube, resulting in a bony defect at the distal end of the tube." [2]The exact cause of spina bifida is unknown but there may be associated with genetic, environmental and dietary factors that can predispose the development of the condition in certain individuals. The most commonly researched factor is the association of low levels of maternal folic acid. Folic acid is a vitamin present in many foods and is often added to breakfast cereals. It can also be found as a supplement in the pharmacy. It is thought to be involved in the development and formation of fetal cells and tissues, therefore, it is advised that folic acid should be taken daily in the upcoming months before conceiving and also during pregnancy [3].
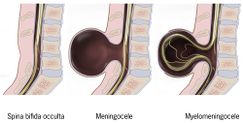
Spina Bifida Occulta is described as a "benign closed NTD posterior vertebral defect only without a meningeal sac; location: lumbar-sacral spine; usually asymptomatic but can be associated with occult spinal dysraphism; usually no associated defects." [5]
Meningocele is described as a "closed NTD without extrusion of spinal cord elements into a meningeal sac; location: cervical, thoracic, lumbar, and/or sacral spine; motor deficits are less likely than with myelomeningocele; structural brain anomalies and Chiari II malformation are less likely." [5]
Myelomeningocele is described as an "open NTD posterior vertebral defect and extrusion of spinal cord elements into a meningeal sac; location: cervical, thoracic, lumbar, and/or sacral spine, leads to paraplegia and insensitivity below the lesion and neurogenic bowel and bladder; associated defects include structural brain anomalies.[5]
Prevalence[edit | edit source]
In the United States, spina bifida occurs in less than 1 in 1,000 births.[5] According to the CDC in 2002, there were approximately 24,860 children and adolescents living with spina bifida in the United States.[6] The prevalence is higher among Caucasian children than black children, however, it is most common in Hispanic populations. [6]
Characteristics/Clinical Presentation[edit | edit source]
Spina Bifida Occulta presents with:
- Depression or dimple in the lower back
- A small patch of dark hair
- Soft fatty deposits
- Port-wine nevi (deep red-purple macular lesions). [7]
Spina Bifida Meningocele presents with:
- A Saclike cyst that protrudes outside the spine [7]
Spina Bifida Occulta and Meningocele usually do not present with neurological deficits; however, bowel and bladder incontinence may be present depending on the level of the lesion.
Spine Bifida Myelomeningocele produces more severe impairments:
- Flaccid or spastic paralysis
- Bladder incontinence
- Musculoskeletal deformities (scoliosis, hip dysplasia, hip dislocation, club foot, hip/knee contracture)
- Hydrocephalus, alone with Type I or II Arnold Chiari malformation
- Trunk hypotonia
- Delayed automatic postural reactions [7]
Signs and Symptoms[edit | edit source]
Children with Spina Bifida can have a variety of symptoms which can vary from mild to severe. The main symptoms include:
- Cognitive symptoms - As spina bifida occurs due to problems with the developing spine and spinal cord, this can have an associated effect on development of the brain. Specifically areas of the brain involved in memory, learning, as well as concentration, understanding and the processing of language. Children may have difficulty with complex motor tasks such as tying laces where good visual and physical coordination is required [8].6 out of 10 children born with spina bifida will have normal intelligence levels, although around half of these will have some form of learning disability [9].
- Mobility Symptoms - The spinal cord allows information to travel up and down to brain in order to control movements made by muscles and joints. As the spinal cord and nerves can be compromised in certain types of Spina Bifida, there are often problems with muscle control and joint movement. In some cases, there may be paralysis of certain muscles which can result in the development of misshapen bones, particularly the feet, and abormal curving of the spine known as Scoliosis [10]. Those with severe mobility restrictions may also develop thin bones or osteoporosis due to the lack of use of the limbs [11]. The spinal cord and nerves also provide the brain with sensory information through touch. As the spinal nerves can be daged in some forms of Spina Bifida, there may be associated loss of sensation and feeling in the pelvic region and legs. This can cause problems with pressure sores and skin breakdown in infants who are unable to feel the need to change position [12]
- Incontinence (Urinary and Bowel) - The nerves travelling through the spinal cord also supply the bladder and bowel, ensuring the muscles within these organs can contract to contain urine and stools within the body. As a result, most children born with Spina Bifida will experience some degree of urinary and bowel incontinence [13]
Associated Co-morbidities[edit | edit source]
Co-morbidities:
- Osteopenia or Osteoporosis: due to the decreased level of activities of many of these individuals this will ultimately cause a decrease in bone density that will put them at risk for fractures [14]
- Obesity: due to decreased activity and sedentary lifestyle
Complications:
- Tethered Cord Syndrome: the spinal cord becomes fixated and begins to stretch which can cause further neurological deterioration [15]
- Urinary Tract Infection: often in individuals who have bowel and bladder incontinence will experience recurrent urinary tract infections [14]
- Decubitis Ulcer: these occur due to the altered sensation an individual may experience from the neurological deficit [14]
Medical Management[edit | edit source]
Medical management of the newly born child with Spina Bifida varies according to the severity of their condition. Those with Spina Bifida Occulta do not ususally require any specific treatment. Some people with Spina Bifida Occulta do not exhibit any symptoms and may only discover they have the condition when they are older after having an XRAY. Children born with myelocoele or myelomeningocoele will require surgery normally within 2-3 days of birth in order to close the gap in the spine and return the spinal cord and nerves to their original place within the spinal column [16]. This aims to prevent infection and further damage to the exposed spinal cord and spinal nerves. Following surgery, the child will be monitored closely for signs of common pos-operative problems associated with this type of surgery, namely hydrocephalus and leaking of cerebrospinal fluid [17]
As the infant gets older, management of incontinence will be an important role of the medical team. Effective management strategies include the use of Clean Intermittent Catheterisation (CIC) and certain drugs which can increase the storage volume of the bladder [18]. Children can also develop constipation due to lack of bowel movements and will require the development of a bowel programme which may involve assisted evacuation of stools. However, this will be based on an individualised assessment of the child and may involve educating the family in order to ensure the programme is effectively integrated into the child’s daily routine [19] Effective strategies in managing incontinence in children with spina bifida are extremely important in allowing them to socially integrate themselves as they get older and attend school [17].
Medications[edit | edit source]
No specific medications are prescribed for the treatment of Spina Bifida. Depending on the location of the protruding sac, the individual may require the use of an assistive device to aid in walking- such as braces, walker, crutches, or a wheelchair. [20]
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
Before Birth
- Alpha-fetoprotein blood test when 16-18 weeks pregnant [20] [21] [22]
- Amniocentesis may be done to further determine the cause of an increase in alpha-fetoprotein [15] [21] [22]
- Ultra-sound of the spine [20] [21]
After Birth
Etiology/Causes[edit | edit source]
Pathology:
- Neural groove develops to form the neural tube around day 20 after conception. In normal development, the upper end is supposed to close at day 25 and the lower end is supposed to close at day 27. Three opportunities could cause abnormal closure of the neural tube. If the hyaluronic acid matrix or actin microfilaments have abnormalities early on, the neural tube will not close. If an overgrowth occurs over the caudal end the neural tube will not close, but this occurs later in development. The last chance for the tube not to close properly occurs when the glycoproteins that typically hold the cells together during closure fail to adhere to the tube together. [7]
There is no exact reason known for the cause of Spina Bifida, but there are a variety of environmental and genetic factors that may be potential risk factors. [22] [21]
Mother’s nutrition:
- Folic acid- less than 400 µg of folic acid per day [20] [2] [23]
- Increase of: Vitamin A, valproic acid, solvents, lead herbicides, glycol ether, clomiphene, carbamazepine, aminopterin, alcohol [7]
Genetic:
- 3%-8% reoccurrence rate for parents who already conceived a child affected with spina bifida [7]
- Incidence rate increases 20x's if the parents already have a child affected with a neural tube defect [23]
- In comparison to African-Americans, Caucasians more commonly have it, and Hispanics have a higher incidence rate than non-Hispanics [23]
Environmental Factors:
- Radiation and viruses may have an impact on developing fetus [21]
Systemic Involvement[edit | edit source]
Occulta and Meningocele: no neurological dysfunction typically present [7]
Myelomeningocele: permanent neurological and musculoskeletal deficits present [7]
- Neurological: muscle weakness, bowel and bladder problems, seizures, paralysis, absent reflexes, sensory impairments [7] [14] [20] [22]
- Musculoskeletal: hip dislocation, syringomyelia, scoliosis, foot and ankle deformities [21]
Medical Management[edit | edit source]
The management of spina bifida varies depending on the degree the individual is affected with the disease.
Spina Bifida Occulta:
- There is generally no medical treatment required
Spina Bifida Meningocele:
- Surgery is often performed early after birth, but the severity of deficits after surgery depends on if there is neural tissue in the sac. Further treatment is similar to the management listed below for myelomeningocele. [20]
Spina Bifida Myelomeningocele:
- Generally, surgery follows within the first few days of life to close the spinal cord defect. It is crucial during this time period prior to surgery to protect the nerves that are exposed in the protruding sac. It is also important to prevent infection and additional trauma to the exposed tissues. [15] [20]
- Additional surgeries may be required to manage other problems in the feet, hips, or spine. The individuals with hydrocephalus will also require subsequent surgeries due to the shunt needing to be replaced. [15] [20]
- The level of malformation of the spinal cord and subsequent neurological defects will influence the individual’s ability to ambulate. Assistive devices may be necessary to aid the individual around the community. [15]
- Due to the bowel and bladder problems that are often caused by the neural tube defect, a bowel and bladder program may be necessary. This may include catheterization or a strict bowel and bladder regimen to remain regular. [15]
- The MOMS study is a trial that was done to look at the effectiveness of having fetal surgery to fix the malformation of the fetus's spine prior to birth in comparison to waiting until after the child is born to have the surgery. The idea behind it was that neurological function tends to decrease as pregnancy progresses, so by performing the surgery in utero the baby would not be exposed to such extensive neurological deficits as it would if the surgery was performed after birth. However, there is a safety concern for both the mother and the fetus when this fetal surgery is performed. The success of the MOMS trial has now made fetal surgery a treatment option in some cases. [24] [25]
Neurogenic bladder is a common complication for people with spina bifida. It is normally treated with pharmaceuticals and intermittent catheterization; however for some patients this treatment does not suffice. New research suggests the idea of tissue engineering and neuromodulation.
Tissue engineering is used to generate new tissue to augment the bladder. Two different theories are utilized: unseeded and seeded. Unseeded “involves the incorporation of a scaffold material (synthetic or biologic) into the host organ, which is used as a template for the ingrowth of native cells that then initiate the regenerative process.” Seeded technology is similar to unseeded; however it adds “cultured cells to the scaffold prior to implantation into the host.”
Neuromodulation modifies the innervation of the bladder so it can potentially function in a normal manner. Neuromodulation includes “non-operative measures such as transurethral electrical bladder stimulation, minimally invasive procedures such as implantation of a sacral neuromodulation pacemaker device, as well as operative measures that reconfigure sacral nerve root anatomy.”
Researchers are still in the early stages of development for this treatment option, however with advancements in technology is could prove to be a promising option for patients with spina bifida.
Physical Therapy Management[edit | edit source]
The main goal is to achieve maximal independence in mobility and to maximize their function, quality of life, and community participation. Spina bifida is a congenital-onset condition that requires intervention by the PT from infancy through adolescence Different factors can affect an individual with myelomeningocele’s ability to ambulate. The most prominent factor found between other socioeconomic and therapeutic factors was the location of the malformation. Individuals who had a higher lesion in the thoracic and upper lumbar spine were more likely to be in wheelchairs in comparison to those with lower lumbar and sacral malformations. Another important factor on an individual's walking ability is the use of assistive devices, whether it is a brace, crutches or a walker. In order to promote walking capacity, an assistive device may be necessary. [14]
In order to properly prescribe exercise training submaximal and maximal testing is necessary. Research has shown that treadmill speed and 6-minute walk distance are the best ways for detecting change. However, heart rate and VO2 peak measures are reliable ways to measure physiological output in ambulatory children with spina bifida, especially when combined with functional outcomes such as the treadmill speed and 6-minute walk distance. [27]
There have been benefits shown in individuals with spina bifida that can be attributed to walking such as urinary drainage, bowel function, and peripheral circulation. The use of different assistive devices has been prescribed to individuals with spina bifida. A long term study was done on individuals that were given an ORLAU Parawalker (a Reciprocal Walking Orthosis). Based on past studies the use of these orthoses are higher than other aides, such as conventional KAFOs, that have been studied in the past. This study suggests that ORLAU Parawalker for children may increase their ability to ambulate which can ultimately provide other benefits that were mentioned earlier. [28] The psychological adjustment to this congenital disability must be considered from the perspective of the parents, the family, and, of course, the child[29]
Differential Diagnosis[edit | edit source]
- Spine segmental dysgenesis: A sporadic disorder characterised by congenital acute-angle kyphosis or kyphoscoliosis that is localised to a spinal segment, usually in the thoracolumbar or upper lumbar spine. [30]
- Caudal regression syndrome (sacral agenesis): A rare disorder associated with maternal diabetes that affects the sacral or lumbosacral spine. [30]
- Multiple Vertebral Segmentation Disorder: Autosomal recessive disorder characterised by short trunk dwarfism, multiple segmentation anomalies of the vertebral column, and coastal anomalies.
- VACTERL (vertebral abnormalities, anal atresia, cardiac abnormalities, tracheo-oesophageal fistula and/or oesophageal atresia, renal agenesis, and dysplasia and limb defects): A non-random association of multiple mid-line congenital anomalies including vertebral, anal, and cardiac defects; tracheo-oesophageal fistula; renal anomalies; and limb anomalies. [30]
Case Reports/ Case Studies[edit | edit source]
Behavioural Treatment of Ambulatory Function in a Child with Myelomeningocele: A Case Report [view in Physical Therapy Journal 1984;64:1536-1539]
Behaviour Therapy in a Gait- Training Program for a Child with Myelomeningocele: A Case Report [view in Physical Therapy Journal 1981;61:1284-1287]
Resources[edit | edit source]
- Spina Bifida Association
- National Institute of Neurological Disorders and Stroke
- Spina Bifida Resource Network
- March of Dimes
- Spina Bifida Quality Toolbox
References[edit | edit source]
- ↑ Campbell LR, Sohal GS. The pattern of neural tube defects created by secondary reopening of the neural tube. J Child Neurol. 1990;5:336-340.
- ↑ 2.0 2.1 Lundy-Ekman L. Neuroscience: Fundamentals for Rehabilitation. 3rd edition. St. Louis: Saunders, 2007.
- ↑ RAY, J.G., MEIER, C., VERLEULEN, M.J., BOSS, S., WYATT, P.R. & COLE, D.E.C., 2002. Association of neural tube defects and folic acid food fortification in Canada. Lancet. Vol. 360 (9350), pp. 2047-2048.
- ↑ YouTube.Osmosis Spina bifida (myelomeningocele, meningocele, occulta) - causes, symptoms, treatment. Available at: http://www.youtube.com/watch?v=jlDZA2PNW2o (accessed 31 July 2020).
- ↑ 5.0 5.1 5.2 5.3 Burke R, Liptak Gregory. Providing a Primary Care Medical Home for Children and Youth with Spina Bifida. American Academy of Pediatrics. 2011; 128:1645-1657
- ↑ 6.0 6.1 Shin M, Besser LM, Siffel C, Kucik JE, Shaw GM, Lu C, Correa A, and the Congenital Anamoly Multistate Prevalence and Collaborative. Prevalence of Spina Bifida Among Children and Adolescents in 10 Regions in the United States. Pediatrics. 2010
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 7.7 7.8 7.9 Goodman C, Fuller K. Pathology: Implications for Physical Therapy. 3rd edition. St. Louis: Saunders,2009
- ↑ BARF, H.A., VERHOEF, M., JENNEKENS-SCHINKEL, A., POST, M.W.M., GOOSHKENS, R.H.J.M. & PREVE, A.J.H., 2003. Cognitive status of young adults with spina bifida. Dev Med Child Neurol. Vol. 45, pp. 813-20.
- ↑ HINDERER, K.A., HINDERER, S.R. & SHURTLEFF, D.B., 2006. Myelodysplasia. In CAMPBELL, S.K., VANDER LINDEN, D.W. & PALISANO, R.J. Physical Therapy for Children. 3rd edition. Pp. 735-789. Philadelphia: Saunders Elsevier
- ↑ PARK BROWN, J., 2001. Orthopaedic care of children with Spina Bifida: You’ve come a long way, baby! Orthopaedic Nursing. Vol. 20 (4), pp. 51-58
- ↑ AUSILI, E., FOCARELLI, B., TABACCO, F., FORTUNELLI, G., CARADONNA., P., MASSIMI, L., SIGISMONDI, M., SALVAGGIO, E. & RENDELI,C., 2008. Bone mineral density and body composition in a myelomeningocoele children population: effects of walking ability and sport activity. European Review for Medical and Pharmacological Sciences. Vol. 12, pp. 349-354
- ↑ TAPPIT-EMAS, E., 2008. Spina Bifida. In J.S, TECKLIN, 4TH eds. Pediatric Physical Therapy. Phyiladelphia: Wolters Kluwer & Lippincott Williams and Wilkins, pp. 231-280
- ↑ SANDLER., A.D., 2010. Children with Spina Bifida: Key Clinical Issues. Pediatr Clin N Am. Vol. 57, pp. 879-892.
- ↑ 14.0 14.1 14.2 14.3 14.4 Fujisawa D, Gois M, Dias J, Alves E, Tavares M, Cardoso J. Intervening factors in the walking of children presenting myelomeningocele. Fisioter 2011;24:275-83.
- ↑ 15.0 15.1 15.2 15.3 15.4 15.5 National Institute of Neurological Disorders and Strokes. Spina Bifida Fact Sheet. http://www.ninds.nih.gov/disorders/spina_bifida/detail_spina_bifida.htm (accessed 1 April 2012).
- ↑ TAPPIT-EMAS, E., 2008. Spina Bifida. In J.S, TECKLIN, 4TH eds. Pediatric Physical Therapy. Phyiladelphia: Wolters Kluwer & Lippincott Williams and Wilkins, pp. 231-280
- ↑ 17.0 17.1 SANDLER., A.D., 2010. Children with Spina Bifida: Key Clinical Issues. Pediatr Clin N Am. Vol. 57, pp. 879-892.
- ↑ LAPIDES, J., DIOKNO, A.C., SILBER, S.J., ET AL 1972. Clean, intermittent self-catheterisation in the treatment of urinary tract disease. J Urol. Vol. 107, pp. 458-61.
- ↑ LEIBOLD, S., 2008. Neurogenic bowel and continence programmes for the individual with spina bifida. J Pediatr Rehabil Med. Vol. 1, pp. 325-36
- ↑ 20.0 20.1 20.2 20.3 20.4 20.5 20.6 20.7 20.8 KidsHealth from Nemours. Spina Bifida. http://kidshealth.org/parent/system/ill/spina_bifida.html (accessed 30 March 2012).
- ↑ 21.0 21.1 21.2 21.3 21.4 21.5 21.6 PubMed Health. Myelomeningocele. http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0002525/ (accessed 30 March 2012).
- ↑ 22.0 22.1 22.2 22.3 Mayo Clinic. Spina Bifida. http://www.mayoclinic.com/health/spina-bifida/DS00417 (accessed 31 March 2012).
- ↑ 23.0 23.1 23.2 Spina Bifida Association. Spina Bifida. http://www.spinabifidaassociation.org/site/c.liKWL7PLLrF/b.2642323/k.8E10/Spina_Bifida.htm (accessed 30 March 2012).
- ↑ UCSF Fetal Treatment Center. Spina Bifida MOMS Trial. http://fetus.ucsfmedicalcenter.org/spina_bifida/moms_trial.asp (accessed 30 March 2012).
- ↑ MOMS: Management of Myelomeningocele Study. Overview of MOMS. http://www.spinabifidamoms.com/english/overview.html (accessed 30 March 2012).
- ↑ YouTube. Spina Bifida- MOMS Study. Available at: http://www.youtube.com/watch?feature=player_embedded&v=i0YpaYitEF4 (accessed 1 Aprile 2012).
- ↑ Groot J, Takken T, Gooskens R, Schoenmakers M, Wubbels M, Vanhees L, et al. Reproducibility of Maximal and Submaximal Exercise Testing in "Normal Ambulatory" and "Community Ambulatory" Children and Adolescents with Spina Bifida: Which is Best for the Evaluation and Application of Exercise Training? Physical Therapy Journal 2011;91:267-276.
- ↑ Roussos N, Patrick J, Hodnett C, Stallard J. A long-term review of severely disabled spina bifida patients using a reciprocal walking system. Disability and Rehabilitation 2001;23:239-244.
- ↑ Loomis JW, Javornisky JG, Monahan JJ, Burke G, Lindsay A. Relations between family environment and adjustment outcomes in young adults with spina bifida. Dev Med Child Neurol. 1997;39:620-627.
- ↑ 30.0 30.1 30.2 BMJ Evidence Center. Spina Bifida and neural tube defects: Differential Diagnosis. http://bestpractice.bmj.com/best-practice/monograph/1161/diagnosis/differential.html (accessed April 2, 2012)