Slow Transit Constipation
Original Editor - Khloud Shreif
Top Contributors - Khloud Shreif and Lucinda hampton
Introduction[edit | edit source]
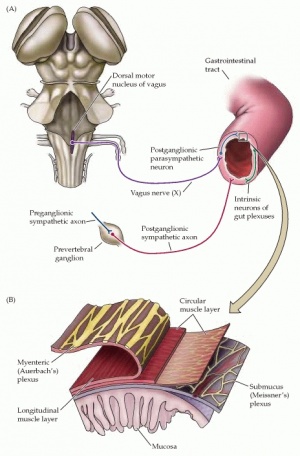
Enteric nervous system or the second brain, is an autonomic nervous system acts independently of the sympathetic, para sympathetic, and brain, it's function related to control the function of the GIT.
Slow transit constipation ( STC) or neural intestinal dysplasia (NID), a rare condition of chronic constipation defined as an ineffective colonic propulsion due to deficit and abnormalities of the enteric system that has a control on the motility of the large intestine, most common in women and may start before he age of 10. This condition may present with no pelvic floor dysfunction or underlying systematic disorder.
Pathological Process[edit | edit source]
There are studies suggested an abnormal neurotransmitters in the muscular layer of their intestinal walls such as a deficiency of a peptide known as substance P, which contribute to peristalsis of the intestinal walls , and abnormality of the number, position, or appearance of nerve cells.
Clinical Presentation[edit | edit source]
The most symptoms varying according to the following:
- Abdominal bloating/ pain.
- Constipation.
- Blood in the stools.
- Haemorrhoids
- Uncontrollable soiling
- Nausea
- Malaise
- Poor appetite.
- Diarrhea
- Malaise
- Another urogynecologic symptoms ( irregular menses, nocturia, and hesitancy). The individual with STC may complain of impair day-to-day functioning that interfere with his work. In addition bowel distention may happen due to backup of contents[1].
- Similar symptoms to functional fecal retention but softer stools, longer interval between two bowel actions.[2]
Diagnosis[edit | edit source]
STC may be diagnosed after birth if the newborn show delayed passage in meconium ≥24h compared with healthy newborn that will need further investigations.
- First, investigations to rule out other secondary causes of constipation.
- Ambulatory colonic manometry, will show impairments in colonic motor activity associated with having meals and during wakeup than normal healthy individuals[1].
- Endoscopy and contrast enema may be used with with patients who don't respond to medical treatment[3].
- Stool diaries, individual can use to note stool form and frequency and can be used to distinguishe between normal and slow transit.
Differential Diagnosis[edit | edit source]
Hirschsprung’s: a congenital birth deficit affect large intestine.
Excluded organic disorders such as:
- Hypothyroidism
- Hypocalcemia
- Drug-induced constipation
- Chronic intestinal pseudo-obstruction[3].
Management[edit | edit source]
Medical treatment[edit | edit source]
Osmotic laxatives: polyethylene glycol, magnesium citrate, stimulant laxatives such as senna/ senokot or bisacodyl/dulcolax , or a combination of the two.
Prosecretory agents: linaclotide and lubiprostone both show great results in the treatment of chronic idiopathic constipation and inflammatory bowel syndrome[3].
Surgical treatment[edit | edit source]
Indications: sever STC, colonic inertia, impairment in colonic response to food. that showed improvement in symptoms and frequency 6 months after operation. It divided into:
- Total colectomy with ileorectal anastomosis (IRA)
- Subtotal colectomy with cecorectal anastomosis (CRA), both operations show most compliant for treatment STC with sever symptoms[5].
Physical therapy treatment[edit | edit source]
Interferential current: used as a transcutaneous electrical stimulation used to increase the motility of bowel in children and showed improvement in defecation frequency, soiling, abdominal pain, urge to defecate whoever the parameters still not known, in addition, studies suggested the longer the duration the better outcome. Electrical stimulation was first applied for 20 minutes 3times/ week and show only improvement in colon motility. Further studies use 1 hour/ day for six months and showed great improvement in motility and frequency of defecations. Results was quite similar to that carried for 3 months
Application: four electrodes 4 cm × 4 cm near the belly button and the back[6][7]. Ideal time and duration not detected yet.
Pelvic floor dysfunction rehabilitation programme if it is affected.
References[edit | edit source]
- ↑ 1.0 1.1 Bharucha AE, Phillips SF. Slow transit constipation. Gastroenterology Clinics of North America. 2001 Mar 1;30(1):77-96.
- ↑ Shin YM, Southwell BR, Stanton MP, Hutson JM. Signs and symptoms of slow-transit constipation versus functional retention. Journal of pediatric surgery. 2002 Dec 1;37(12):1762-5.
- ↑ 3.0 3.1 3.2 Tillou J, Poylin V. Functional disorders: slow-transit constipation. Clinics in colon and rectal surgery. 2017 Feb;30(01):076-86.
- ↑ Medskl.com. Adult Constipation: The 3 causes to consider when presenting with less than 3 BMs a week Available from: http://www.youtube.com/watch?v=oTIVFR78J8k[last accessed 2/5/2021]
- ↑ Li F, Fu T, Tong W, Zhang A, Li C, Gao Y, Wu JS, Liu B. Effect of different surgical options on curative effect, nutrition, and health status of patients with slow transit constipation. International journal of colorectal disease. 2014 Dec;29(12):1551-6.
- ↑ Yik YI, Hutson J, Southwell B. Home‐based transabdominal interferential electrical stimulation for six months improves paediatric slow transit constipation (STC). Neuromodulation: Technology at the Neural Interface. 2018 Oct;21(7):676-81.
- ↑ Clarke MC, Chase JW, Gibb S, Robertson VJ, Catto-Smith A, Hutson JM, Southwell BR. Decreased colonic transit time after transcutaneous interferential electrical stimulation in children with slow transit constipation. Journal of pediatric surgery. 2009 Feb 1;44(2):408-12.