Scleroderma: Difference between revisions
No edit summary |
No edit summary |
||
| Line 152: | Line 152: | ||
== Case Reports/ Case Studies == | == Case Reports/ Case Studies == | ||
[[Scleroderma Case Study]] | |||
[http://www.cmj.org/Periodical/paperlist.asp?id=LW201274419102401728&linkintype=pubmed Portal hypertensive ascites can occur in limited systemic sclerosis with positive anti-centromere antibody and respond to corticosteroid treatment.]<br> | [http://www.cmj.org/Periodical/paperlist.asp?id=LW201274419102401728&linkintype=pubmed Portal hypertensive ascites can occur in limited systemic sclerosis with positive anti-centromere antibody and respond to corticosteroid treatment.]<br> | ||
| Line 160: | Line 160: | ||
[http://www.grupoaran.com/mrmUpdate/lecturaPDFfromXML.asp?IdArt=4620306&TO=RVN&Eng=1 When scleroderma affects the esophagus, patients can present with signs and symptoms similar to gastroesophageal reflux ]<br> | [http://www.grupoaran.com/mrmUpdate/lecturaPDFfromXML.asp?IdArt=4620306&TO=RVN&Eng=1 When scleroderma affects the esophagus, patients can present with signs and symptoms similar to gastroesophageal reflux ]<br> | ||
[http://www.ncbi.nlm.nih.gov/pubmed/22403762 A correlation could exist between breast cancer and the development of scleroderma] | [http://www.ncbi.nlm.nih.gov/pubmed/22403762 A correlation could exist between breast cancer and the development of scleroderma] | ||
== Resources <br> == | == Resources <br> == | ||
Revision as of 20:28, 20 January 2015
Original Editors - Amanda Schoenfelder & Katie Williams from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Bridget Ward, Katie Williams, Amanda Schoenfelder, Lucinda hampton, Admin, Elaine Lonnemann, Khloud Shreif, WikiSysop, Kim Jackson, Sehriban Ozmen and Wendy Walker
Definition/Description[edit | edit source]
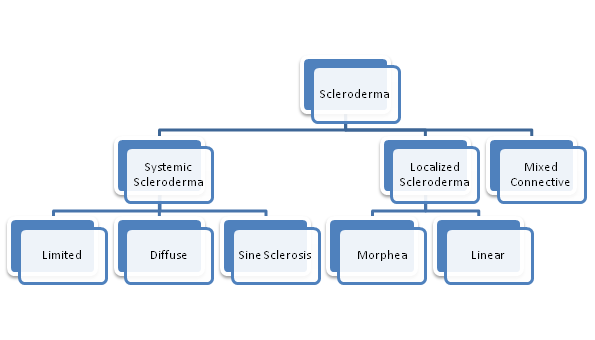
Scleroderma is a connective tissue disease that involves changes in the skin, blood vessels, muscles, and internal organs.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title It is a chronic, progressive autoimmune disorder where inflammation and the overproduction of collagen accumulate in the body.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title There are two main types of Scleroderma- Systemic and Localized.
Systemic Scleroderma may affect multiple systems such as the integumentary, cardiopulmonary, vascular, gastrointestinal, genitourinary, or musculoskeletal. There are three forms of Systemic Scleroderma.
- With Diffuse Scleroderma skin thickening occurs more rapidly and involves more skin areas than in limited. In addition, people with diffuse scleroderma have a higher risk of developing “sclerosis” or fibrous hardening of the internal organs.Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - Sine Scleroderma involves organ fibrosis with no skin involvement.Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - With Limited Scleroderma (CREST syndrome) skin thickening is less widespread, typically confined to the fingers, hands and face, and develops slowly over years. Internal problems occur, but they are less frequent and tend to be less severe than in diffuse scleroderma.Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title
Localized Scleroderma usually affects only the skin on the hands and face. It develops slowly, and rarely, if ever, spreads throughout the body or causes serious complications.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title There are two types of Localized Scleroderma.
- Morphea is characterized by waxy patches on the skin of varying sizes, shapes and color. The skin under the patches may thicken. The patches may enlarge or shrink, and often may disappear spontaneously.Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - Linear Scleroderma starts as a streak or line of hardened, waxy skin on an arm or leg or on the head and neck. Linear scleroderma tends to involve deeper layers of the skin as well as the surface layers, and sometimes affects the motion of the joints, which lie underneath.Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title Linear scleroderma often appears mostly on one side of the body. Cite error: Invalid<ref>tag; name cannot be a simple integer. Use a descriptive title
Mixed Connective Disease is when Scleroderma is diagnosed when another disease, such as systemic lupus erythematosus and polymyositis, has been previously diagnosed.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Prevalence[edit | edit source]
It’s estimated that about 300,000 Americans have scleroderma. About one third of those people have the systemic form of scleroderma. Localized scleroderma is more common in children, whereas systemic scleroderma is more common in adults. Overall, female patients outnumber male patients about 4-to-1. Although scleroderma is not directly inherited, some scientists feel there is a slight predisposition to it in families with a history of rheumatic diseases. However, scleroderma can develop in every age group from infants to the elderly, but its onset is most frequent between the ages of 25 to 55. Race and ethnic background, may influence the risk of getting scleroderma, the age of onset, and the pattern or severity of internal organ involvement.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleChoctaw Native Americans in Oklahoma are at least 20 times as likely as is the general population to develop systemic scleroderma. This increased risk doesn't apply to Choctaws living in Mississippi. African-Americans are more at risk to develop systemic scleroderma and are more likely to develop severe lung complications.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Characteristics/Clinical Presentation Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title[edit | edit source]
Associated Co-morbidities
[edit | edit source]
- Rheumatalogic/Autoimmune Disorders: Systemic Lupus Erythematosus
- Polymyositis
- Multiple Sclerosis
- Pulmonary Fibrosis
- Cancer
- Left Sided Heart Failure
- Pulmonary Artery Hypertension
- Kidney Failure
- Depression
- High Blood Pressure
- Kidney Disease
- Sjögren Disease
- Raynaud's
- GERD
Medications
[edit | edit source]
Medicines used to treat scleroderma include: [1]
• Anti-inflammatory medicines such as corticosteroids
• Immune-suppressing medications such as methotrexate and Cytoxan
• Nonsteroidal anti-inflammatory drugs (NSAIDs)
Scleroderma can affect many different organs and organ systems. Additional medications are based on the symptoms that the individual experiences.
Examples of other treatments for specific symptoms include:[1][2]
• Medicines for heartburn or swallowing problems
• Blood pressure medications (particularly ACE inhibitors) for high blood pressure or kidney problems
• Light therapy to relieve skin thickening
• Medicines to improve breathing
• Medications to treat Raynaud's phenomenon
• Intestinal dysfunction
• Medicines to increase saliva secretion in the mouth to reduce effects of Sjogren’s Syndrome (a chronic autoimmune disease in which a person’s white blood cells attack their moisture-producing glands)
Diagnostic Tests/Lab Tests/Lab ValuesCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
[edit | edit source]
Depending on your particular symptoms, a diagnosis of scleroderma may be made by:
- A general internist.
- A dermatologist (a doctor who specializes in treating diseases of the skin, hair, and nails).
- An orthopaedist (a doctor who treats bone and joint disorders).
- A pulmonologist (a lung specialist).
- A rheumatologist (a doctor specializing in treatment of musculoskeletal disorders and rheumatic diseases).
A diagnosis of scleroderma is based largely on the medical history and findings from the physical exam. Once your doctor has taken a thorough medical history, he or she will perform a physical exam. Finding one or more of the following factors can help the doctor diagnose a certain form of scleroderma:
- Changed skin appearance and texture, including swollen fingers and hands and tight skin around the hands, face, mouth, or elsewhere
- Calcium deposits developing under the skin
- Changes in the tiny blood vessels (capillaries) at the base of the fingernails
- Thickened skin patches.
Finally, your doctor may order lab tests to help confirm a suspected diagnosis. At least two proteins, called antibodies, are commonly found in the blood of people with scleroderma:
- Antitopoisomerase-1 or Anti-Scl-70 antibodies appear in the blood of up to 30 percent of people with diffuse systemic sclerosis.
- Anticentromere antibodies are found in the blood of many people with limited systemic sclerosis.
Because not all people with scleroderma have these antibodies and because not all people with the antibodies have scleroderma, lab test results alone cannot confirm the diagnosis.
In some cases, your doctor may order a skin biopsy (the surgical removal of a small sample of skin for microscopic examination) to aid in or help confirm a diagnosis.
Diagnosing scleroderma is easiest when a person has typical symptoms and rapid skin thickening. In other cases, a diagnosis may take months, or even years, as the disease unfolds and reveals itself and as the doctor is able to rule out some other potential causes of the symptoms. In some cases, a diagnosis is never made, because the symptoms that prompted the visit to the doctor go away on their own.
Etiology/Causes Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title[edit | edit source]
The cause of scleroderma is unknown, but it cannot be transmitted from person to person. Several factors that may increase a person's risk of getting scleroderma include:
Abnormal immune or inflammatory activity: In scleroderma, the immune system is thought to stimulate cells called fibroblasts so they produce too much collagen. People who already have rheumatic or autoimmune disorders are at increased risk due to previous abnormal autoimmune activity.
Genetic makeup: Although genes seem to put certain people at risk for scleroderma and play a role in its course, the disease is not passed from parent to child like some genetic diseases. Research indicates that there is a susceptibility gene, which raises the likelihood of getting scleroderma, but by itself does not cause the disease. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Environmental triggers: Research suggests that exposure to some environmental factors may trigger scleroderma-like disease in people who are genetically predisposed to it. Suspected triggers include viral infections, certain adhesive and coating materials, and organic solvents such as vinyl chloride or trichloroethylene. But no environmental agent has been shown to cause scleroderma. In the past, some people believed that silicone breast implants might have been a factor in developing connective tissue diseases such as scleroderma. But several studies have not shown evidence of a connection.
Hormones: Women develop scleroderma more often than men. Scientists suspect that hormonal differences between women and men play a part in the disease. However, the role of estrogen or other female hormones has not been proven.
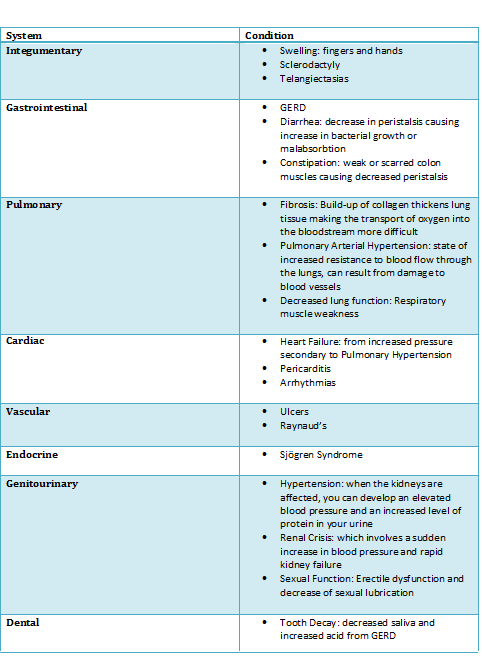
Systemic Involvement Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title[edit | edit source]
Medical Management (current best evidence) Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title[edit | edit source]
Currently, there is no treatment that controls or stops the underlying problem—the overproduction of collagen—in all forms of scleroderma. Treatment and management focus on relieving symptoms and limiting damage, which is dependent upon the problems each individual experiences.
Several different specialists may be involved in the care of one person since scleroderma can affect many different organs and organ systems. Typically, care will be managed by a rheumatologist, who may refer the patient to other specialists, depending on the specific problems they are having.
These specialists can include:
• Dermatologist for the treatment of skin symptoms
• Nephrologist for kidney complications
• Cardiologist for heart complications
• Gastroenterologist for problems of the digestive tract
• Pulmonary specialist for lung involvement
Physical Therapy Management (current best evidence)[edit | edit source]
Physical therapy can be very beneficial in the treatment of scleroderma. Physical therapists can design a program of regular stretching and gentle exercise to help:
• Manage pain
• Improve strength
• Improve/maintain mobility
• Minimize joint contractures
• Improve circulation
• Enhance/maintain performance of activities of daily living in order to encourage independence
In addition, an appropriate level of exercise can promote relaxation and a sense of well-being. [3]
Alternative/Holistic Management (current best evidence)[edit | edit source]
Yoga, meditation, and biofeedback can help manage stress and anxiety caused by the frustrations and complications of scleroderma.
Some nutritional supplements can improve or worsen the symptoms caused by scleroderma. [3]
File:Table nutrition complex pt.png
Differential Diagnosis Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title[edit | edit source]
A number of other diseases have symptoms similar to those seen in scleroderma.
Some of the most common include:
Eosinophilic fasciitis (EF): This disease involves the fascia, the thin connective tissue around the muscles, particularly those of the forearms, arms, legs, and trunk. EF causes the muscles to become encased in collagen, the fibrous protein that makes up tissue such as the skin and tendons. Contractures may develop, sometimes causing disfigurement and problems with joint motion and function. EF may begin after hard physical exertion. The disease usually fades away after several years, but people sometimes have relapses. Although the upper layers of the skin are not thickened in EF, the thickened fascia may cause the skin to look somewhat like the tight, hard skin of scleroderma. A skin biopsy easily distinguishes between the two diseases.
Skin thickening on the fingers and hands: This also appears with diabetes, mycosis fungoides, amyloidosis, and adult celiac disease. It can also result from hand trauma.
Generalized scleroderma-like skin thickening: This may occur with scleromyxedema, graft-versus-host disease, porphyria cutanea tarda, and human adjuvant disease.
Internal organ damage: Similar to that seen in systemic sclerosis, this may instead be related to primary pulmonary hypertension, idiopathic pulmonary fibrosis, or collagenous colitis.
Raynaud’s phenomenon (pictured below): This condition also appears with atherosclerosis or systemic lupus erythematosus or in the absence of underlying disease.
Case Reports/ Case Studies[edit | edit source]
Scleroderma can present with pulmonary nodules
A correlation could exist between breast cancer and the development of scleroderma
Resources
[edit | edit source]
American College of Rheumatology
National Institute of Arthritis and Musculoskeletal and Skin Diseases
Scleroderma Research Foundation
Recent Related Research (from Pubmed)[edit | edit source]
References[edit | edit source]
see adding references tutorial.
- ↑ 1.0 1.1 Teitel A D. Medline Plus [internet]. Bethesda (MD): U.S. National Library of Medicine; c1997-2013. Scleroderma; 2013 Feb 27 [cited 2013 Mar 6]; [about 5 screens]. Available from: http://www.nlm.nih.gov/medlineplus/ency/article/000429.htm
- ↑ Scleroderma Research Foundation [internet]. San Francisco: Scleroderma Research Foundation; c2013. Current Treatments; [unknown publication date][cited 2013 Mar 6]; [about 11 screens]. Available from: http://www.srfcure.org/for-patients/current-treatments
- ↑ 3.0 3.1 Scleroderma Research Foundation [internet]. San Francisco: Scleroderma Research Foundation; c2013. Tips for Living with Scleroderma; [unknown publication date][cited 2013 Mar 6]; [about 7 screens]. Available from: http://www.srfcure.org/for-patients/tips-for-living