Scaphoid Fracture: Difference between revisions
Abbey Wright (talk | contribs) No edit summary |
Abbey Wright (talk | contribs) No edit summary |
||
| Line 56: | Line 56: | ||
Plain [[X-Rays|X-rays]] are commonly used to diagnose the fracture, but this approach may miss up to 16% of fractures in the absence of clear-cut lucent lines on plain radiographs<ref name=":2">Bäcker HC, Wu CH, Strauch RJ. [https://pubmed.ncbi.nlm.nih.gov/32025360/ Systematic Review of Diagnosis of Clinically Suspected Scaphoid Fractures]. J Wrist Surg. 2020 Feb;9(1):81-89. doi: 10.1055/s-0039-1693147. Epub 2019 Jul 21. PMID: 32025360; PMCID: PMC7000269.</ref>. Plain radiographs have 64% specificity for scaphoid fractures. | Plain [[X-Rays|X-rays]] are commonly used to diagnose the fracture, but this approach may miss up to 16% of fractures in the absence of clear-cut lucent lines on plain radiographs<ref name=":2">Bäcker HC, Wu CH, Strauch RJ. [https://pubmed.ncbi.nlm.nih.gov/32025360/ Systematic Review of Diagnosis of Clinically Suspected Scaphoid Fractures]. J Wrist Surg. 2020 Feb;9(1):81-89. doi: 10.1055/s-0039-1693147. Epub 2019 Jul 21. PMID: 32025360; PMCID: PMC7000269.</ref>. Plain radiographs have 64% specificity for scaphoid fractures. | ||
Research has shown that the use of [[MRI Scans|MRI]]<nowiki/>ior [[CT Scans|CT]]<nowiki/>s effective in indeterminate a scaphoid fracture. Both methods have been shown to detect fractures, but the MRI found some significant ligamentous and carpal instabilities in addition to the scaphoid fracture.<ref name=":2" /><ref name="p0">Moran | Research has shown that the use of [[MRI Scans|MRI]]<nowiki/>ior [[CT Scans|CT]]<nowiki/>s effective in indeterminate a scaphoid fracture. Both methods have been shown to detect fractures, but the MRI found some significant ligamentous and carpal instabilities in addition to the scaphoid fracture.<ref name=":2" /><ref name="p0">Parvizi J, Wayman J, Kelly P, Moran CG. [https://pubmed.ncbi.nlm.nih.gov/9665518/ Combining the clinical signs improves diagnosis of scaphoid fractures. A prospective study with follow-up]. J Hand Surg Br. 1998 Jun;23(3):324-7. </ref><ref name=":3">Clementson, M., Björkman, A., & Thomsen, N. (2020). [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7047900/ Acute scaphoid fractures: guidelines for diagnosis and treatment.] ''EFORT open reviews'', ''5''(2), 96–103. </ref><br> | ||
== Outcome Measures == | == Outcome Measures == | ||
*[[DASH Outcome Measure|DASH]] or QuickDASH (Disabilities of Arm, Shoulder or Hand) | *[[DASH Outcome Measure|DASH]] or QuickDASH (Disabilities of Arm, Shoulder or Hand) | ||
*[https://physio-pedia.com/PRWE_Score?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal#share PRWE], a fifteen-item questionnaire was designed to measure wrist pain and disability.<ref name="p4">Mc Dermid, Patient Rating of Wrist Pain and Disability: A Reliable and Valid Measurement Tool, 1998.</ref> | *[https://physio-pedia.com/PRWE_Score?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal#share PRWE], a fifteen-item questionnaire was designed to measure wrist pain and disability.<ref name="p4">Mc Dermid, Patient Rating of Wrist Pain and Disability: A Reliable and Valid Measurement Tool, 1998.</ref> | ||
*PEM | *PEM (Patient Evaluation Measure) has a simple layout with questions asked in a visual analog form. Patients are asked to read and comprehend the question alone and not the description of each interval answer.<ref name="p5" /> | ||
== Assessment == | == Assessment == | ||
| Line 98: | Line 96: | ||
=== Conservative management === | === Conservative management === | ||
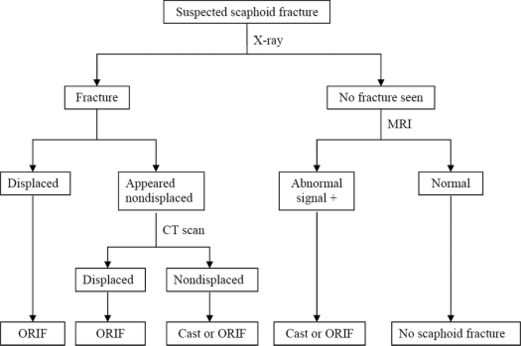
* Fractures that are non-displaced and within the distal third of the bone can be managed non-operatively with immobilization in a cast. Debate exists as to whether a long or short arm cast is optimal and whether a thumb spica should be included to immobilize the thumb, no evidence currently suggests one option is better than the other. | *[[File:Scaphoid fracture algorythm.jpg|thumb|521x521px|<ref>Kawamura, K., & Chung, K. C. (2008). [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4405116/ Treatment of scaphoid fractures and nonunions]. ''The Journal of hand surgery'', ''33''(6), 988–997. </ref>]]Fractures that are non-displaced and within the distal third of the bone can be managed non-operatively with immobilization in a cast. Debate exists as to whether a long or short arm cast is optimal and whether a thumb spica should be included to immobilize the thumb, no evidence currently suggests one option is better than the other. | ||
* Six weeks immobilization is normally required with repeat radiographs taken at this time to assess for the union. | * Six weeks immobilization is normally required with repeat radiographs taken at this time to assess for the union. | ||
* Time to union varies depending on the location of the fracture. | * Time to union varies depending on the location of the fracture. | ||
| Line 113: | Line 111: | ||
The fractured scaphoid exhibits certain behavior that inhibits healing. Fracture fragments are inherently unstable and prone to displacement and require motionless contact to achieve union.<ref name="p5" /> As mentioned before, the blood supply of the scaphoid is tenuous. | The fractured scaphoid exhibits certain behavior that inhibits healing. Fracture fragments are inherently unstable and prone to displacement and require motionless contact to achieve union.<ref name="p5" /> As mentioned before, the blood supply of the scaphoid is tenuous. | ||
For therapeutic decision making, the scaphoid is divided into three anatomic sections: proximal, medial, and distal. Fractures are further subdivided into displaced and non-displaced types.<ref name="p3" /> | For therapeutic decision making, the scaphoid is divided into three anatomic sections: proximal, medial, and distal (see image). Fractures are further subdivided into displaced and non-displaced types.<ref name="p3" /> | ||
[[Image:Scaphoid fracture types.gif|left|450x400px]] | [[Image:Scaphoid fracture types.gif|left|450x400px]] | ||
=== Non-displaced Fractures === | === Non-displaced Fractures === | ||
<br>Non-displaced distal fractures heal well with strict immobilization in a well-molded short arm thumb spica. Controversy exists over whether to use a long arm or a short arm cast. | <br>Non-displaced '''distal''' fractures heal well with strict immobilization in a well-molded short arm thumb spica. Controversy exists over whether to use a long arm or a short arm cast. he current treatment for this type of fracture is a thumb spica, but some evidence suggests that the thumb could be omitted from the cast.<ref name="p9">Fowler, C., Sullivan, B., Williams, L. ''et al.'' [https://link.springer.com/article/10.1007/s002560050459 A comparison of bone scintigraphy and MRI in the early diagnosis of the occult scaphoid waist fracture.] Skeletal Radiol 27, 683–687 (1998).</ref> | ||
Screw fixation may speed recovery to pre-injury activities; referral for surgery may be indicated, depending on the needs of the patient<ref name="p0" />. As the fracture line moves proximally, there is more risk of displacement and nonunion; therefore, it would be appropriate to refer these patients for orthopedic consultation. If conservative treatment is attempted, a long arm cast with thumb immobilization is appropriate.<ref name="p3" /><ref>Grewal, | Screw fixation may speed recovery to pre-injury activities; referral for surgery may be indicated, depending on the needs of the patient<ref name="p0" />. | ||
As the fracture line moves '''proximally''', there is more risk of displacement and nonunion; therefore, it would be appropriate to refer these patients for orthopedic consultation. If conservative treatment is attempted, a long arm cast with thumb immobilization is appropriate.<ref name="p3" /><ref>Grewal R, Suh N, MacDermid JC. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5034027/# Is Casting for Non-Displaced Simple Scaphoid Waist Fracture Effective? A CT Based Assessment of Union.] Open Orthop J. 2016 Sep 15;10:431-438. </ref><br> | |||
=== Displaced Fractures === | === Displaced Fractures === | ||
<br>Fractures with even small amounts of displacement are prone to nonunion, and operative treatment is recommended<ref name="p1" />. | <br>Fractures with even small amounts of displacement are prone to nonunion, and operative treatment is recommended<ref name="p1" />. | ||
For the fixation, double-threaded headless screws are preferred. Which operative technique to use depends on the fracture morphology.<ref>Schädel-Höpfner, M., et al. "Acute scaphoid fractures: Management under consideration of the new S3-level guideline." ''Der Orthopade'' 45.11 (2016): 945-950. (level of evidence 5)</ref> Splinting and referral are indicated.<ref name="p3" /> | |||
Traditionally, undisplaced and stable scaphoid fractures are treated by casting in short- or long-arm casts. After the immobilization, you must start with stretching exercises en strengthening exercises.<ref name="p2" /><ref name="p3" /><br><br>''Stretching exercises:'' | Traditionally, undisplaced and stable scaphoid fractures are treated by casting in short- or long-arm casts. After the immobilization, you must start with stretching exercises en strengthening exercises.<ref name="p2" /><ref name="p3" /><br><br>''Stretching exercises:'' | ||
Revision as of 16:02, 11 November 2020
Original Editor - Dawn Waugh
Top Contributors - Dawn Waugh, Mats Vandervelde, Abbey Wright, Inoa De Pauw, Admin, Chrysolite Jyothi Kommu, Kim Jackson, Evan Thomas, Rachael Lowe, Amanda Ager, Anas Mohamed, Lucinda hampton, Johnathan Fahrner, WikiSysop, Wanda van Niekerk, 127.0.0.1, Nupur Smit Shah, Vanessa Rhule, Naike De Win and Claire Knott
Definition/ Description[edit | edit source]
The scaphoid bone is the most commonly fractured carpal bone. In young children and the elderly population, scaphoid fractures are rare. The scaphoid bone is stronger than the relatively weak distal radius in these age groups.[1][2]
A delay in diagnosis of scaphoid fractures can lead to a variety of adverse outcomes that include nonunion (no consolidation), delayed union, decreased grip strength, and range of motion, along with osteoarthritis of the radiocarpal joint. Timely diagnosis, appropriate immobilization, and referral to surgical opinion when indicated can decrease the likelihood of adverse outcomes.[3][2]
Scaphoid fractures are common, but present unique challenges because of the particular geometry of the fractures and the tenuous vascular pattern of the scaphoid. Delays in diagnosis and inadequate treatment for acute scaphoid fractures can lead to non-unions and subsequent degenerative wrist arthritis.[4]
Clinically Relevant Anatomy[edit | edit source]
The scaphoid is one of the 8 carpal bones of the wrist. It is a boat-shaped carpal bone that articulates with the distal radius, trapezium, and capitate. During the extension and radial deviation of the wrist, the movement is limited by the scaphoid conflicting with the radius.
Anatomically, the scaphoid has proximal and distal poles with a waist between the two. Blood supply to the scaphoid bone is predominantly from branches of the radial artery (dorsal carpal branch). The retrograde nature of the blood supply means that fractures at the waist of the scaphoid leave the proximal pole at a high risk of avascular necrosis.
Epidemiology[edit | edit source]
- Scaphoid fractures predominantly affect young adults, with a mean age of 29 years.
- Higher incidence in males.
- Unusual in the pediatrics population and the elderly population where the physis or distal radius, respectively, are more likely to fracture first.
- Scaphoid fractures account for 15% of acute wrist injuries.[5]
- Scaphoid fractures have a high incidence of nonunion (8-10%), frequent malunion, and late sequelae of carpal instability and post-traumatic arthritis[6].
- No blood vessels enter the proximal pole of the scaphoid, thus a higher incidence of aseptic necrosis and nonunion is noted with fractures on this side of the scaphoid [6].
- Displaced fractures frequently are associated with ligamentous tears in the wrist.[6]
Characteristics/ Clinical Presentation[edit | edit source]
Patients typically present with wrist pain following a fall onto an outstretched hand.
- Axial loading of the wrist with it in forced hyperextension and radial deviation can cause the fracture as the scaphoid impacts on the dorsal rim of the radius.
- Traumatic injury through contact sports and road traffic accidents are also common causes.[5]
Following the traumatic event there will be a massive force of the hand on the arm through the scaphoid bone[1][2][7].
The symptoms will likely be:
- Deep, dull ache in the radial part of the wrist.
- Aggravated pain by pinching and gripping.
- Localised wrist swelling with fullness in the anatomical snuffbox
- Localised bruising
- Tenderness on palpation of the radial side of the wrist
Differential Diagnosis[edit | edit source]
These diagnoses can be differentiated by the location of tenderness, pain with certain maneuvers, and radiographic abnormalities.[2][8]
- Distal radius fracture
- Other carpal bone fractures
- Scapholunate dissociation
- De Quervain’s tenosynovitis
- Osteoarthritis
- Tendinopathy[5]
Diagnostic Procedures[edit | edit source]
Plain X-rays are commonly used to diagnose the fracture, but this approach may miss up to 16% of fractures in the absence of clear-cut lucent lines on plain radiographs[9]. Plain radiographs have 64% specificity for scaphoid fractures.
Research has shown that the use of MRIior CTs effective in indeterminate a scaphoid fracture. Both methods have been shown to detect fractures, but the MRI found some significant ligamentous and carpal instabilities in addition to the scaphoid fracture.[9][10][11]
Outcome Measures[edit | edit source]
- DASH or QuickDASH (Disabilities of Arm, Shoulder or Hand)
- PRWE, a fifteen-item questionnaire was designed to measure wrist pain and disability.[7]
- PEM (Patient Evaluation Measure) has a simple layout with questions asked in a visual analog form. Patients are asked to read and comprehend the question alone and not the description of each interval answer.[6]
Assessment[edit | edit source]
Subjective assessment[edit | edit source]
- History of trauma i.e. fall onto an outstretched hand
- Dull pain which is aggravated by hand and wrist movements
- Restricted thumb range of movement[4]
Objective exam[edit | edit source]
When examining a patient with a suspected scaphoid injury, it is important to compare the injured wrist with the uninjured wrist.
Presentation may include:
- Anatomical snuffbox tenderness on examination - highly sensitive 90% indication of scaphoid fracture, but it is nonspecific 40%[1]
- Tenderness of the scaphoid tubercle: the physician extends the patient’s wrist with one hand and applies pressure to the tuberosity at the proximal wrist crease with the opposite hand. This provides better diagnostic information; sensitivity 87%, specificity 57%[1]
- Pain with the scaphoid compression test (i.e. axially/longitudinally compressing a patient’s thumb along the line of the first metacarpal) was shown to be helpful in identifying a scaphoid fracture, but in another study[3][2],
- Pain in the snuffbox with pronation of the wrist followed by ulnar deviation (52% percent positive predictive value, 100% percent negative predictive value)[2]
Medical Management[edit | edit source]
Suspected fractures with positive clinical findings on examination but negative radiographs should have a follow-up with films repeated in 7-14 days. If pain persists and radiographs are still normal, then further imaging in the form of MRI or CT should be undertaken. Pain management with the assistance of pharmacists should be considered.
Surgical Management[edit | edit source]
Indications for operative management include:
- Displacement greater than 1mm
- An intrascaphoid angle greater than 35 degrees (humpback deformity)
- A radiolunate angle of more than 15 degrees
- Transcaphoid perilunate dislocation
- Proximal pole fractures
- Comminuted fractures
- Non displaced waist fractures in individuals that need to return quickly to work/sport
- Nonunion or avascular necrosis
Surgical fixation involves the insertion of a single or multiple screws and can be done percutaneously or via an open procedure. The latter is preferable for non-unions and those fractures that exhibit gross displacement with the former for acute, minimally displaced fractures[5].
Conservative management[edit | edit source]
- Fractures that are non-displaced and within the distal third of the bone can be managed non-operatively with immobilization in a cast. Debate exists as to whether a long or short arm cast is optimal and whether a thumb spica should be included to immobilize the thumb, no evidence currently suggests one option is better than the other.
- Six weeks immobilization is normally required with repeat radiographs taken at this time to assess for the union.
- Time to union varies depending on the location of the fracture.
- The distal-third would be expected to heal within 6-8 weeks for approximately 90% of non-displaced or minimally displaced (≤ 0.5 mm) scaphoid waist fractures,
- middle-third within 8-12 weeks
- proximal third within weeks.
- Scaphoid waist fractures with moderate displacement (0.5-1.5 mm) can be treated conservatively, require prolonged cast immobilization for eight to ten weeks.[11]
- The relative increase in time to healing while moving from distal to proximal is secondary to the tenuous blood supply and retrograde arterial flow.[5]
As a basic rule, in a patient with a clinically suspected scaphoid fracture but negative initial radiographs, it is reasonable to apply a short arm thumb spica and re-evaluate the patient in two weeks. If a cast is not applied, the fracture can worsen over the following months. At the two-week visit, the patient should be free of pain, and a follow-up radiograph should be obtained.[2]
Types of fracture[edit | edit source]
The fractured scaphoid exhibits certain behavior that inhibits healing. Fracture fragments are inherently unstable and prone to displacement and require motionless contact to achieve union.[6] As mentioned before, the blood supply of the scaphoid is tenuous.
For therapeutic decision making, the scaphoid is divided into three anatomic sections: proximal, medial, and distal (see image). Fractures are further subdivided into displaced and non-displaced types.[2]
Non-displaced Fractures[edit | edit source]
Non-displaced distal fractures heal well with strict immobilization in a well-molded short arm thumb spica. Controversy exists over whether to use a long arm or a short arm cast. he current treatment for this type of fracture is a thumb spica, but some evidence suggests that the thumb could be omitted from the cast.[13]
Screw fixation may speed recovery to pre-injury activities; referral for surgery may be indicated, depending on the needs of the patient[10].
As the fracture line moves proximally, there is more risk of displacement and nonunion; therefore, it would be appropriate to refer these patients for orthopedic consultation. If conservative treatment is attempted, a long arm cast with thumb immobilization is appropriate.[2][14]
Displaced Fractures[edit | edit source]
Fractures with even small amounts of displacement are prone to nonunion, and operative treatment is recommended[1].
For the fixation, double-threaded headless screws are preferred. Which operative technique to use depends on the fracture morphology.[15] Splinting and referral are indicated.[2]
Traditionally, undisplaced and stable scaphoid fractures are treated by casting in short- or long-arm casts. After the immobilization, you must start with stretching exercises en strengthening exercises.[3][2]
Stretching exercises:
- Flexion: bend your wrist forward
- Extension: bend your wrist backward
- Radial and ulnar deviation: move your wrist side to side
- Wrist stretch: press the back of the hand on your injured side with your other hand to help bend your wrist.
- Wrist extension stretch: Stand at a table with your palms down, fingers flat, and elbows straight. Lean your body weight forward.
Strengthening exercises:
- Wrist flexion and extension: Hold a weight in your hand and bend your wrist upward and downward.
- Finger flexion an extension: exercises with a power web™
- Forearm pronation and supination: keep your arm in an angle of 90°, Turn your palm up and hold for 5 seconds. Then slowly turn your palm down and hold for 5 seconds.[2]
Revalidation week to week
Rehabilitation considerations immediately following an injury to 1 week[6]
For casted fractures
- Active range of motion (AROM) and passive range of motion (PROM) to the digits, except the thumb, which is immobilized
- AROM and active-assisted range of motion (AAROM) exercises to the shoulder
- Isometric exercises to the biceps, triceps, and deltoid muscles
Following open reduction internal fixation (ORIF) surgery
- Elevation of the arm to treat dependent edema
- AROM and PROM of digits, except the thumb
- AROM and AAROM exercises to the elbow and shoulder
- Isometric exercises to the biceps, triceps, and deltoid muscles
- Limitation of supination and pronation
Rehabilitation considerations in 2 weeks[6]
The clinician may obtain bone or CT scans in the event of continued pain and tenderness over the snuffbox with negative radiographic findings.
Bone stimulators have been increasingly used for stable, non-displaced fractures and for suspected scaphoid fractures with negative radiographic findings, although both uses are still somewhat controversial.
A short-arm cast is indicated for a suspected fracture, while a long-arm cast is used for a known fracture.
The patient should continue ROM exercises for casted fractures and ORIF, as above.
Rehabilitation considerations in 4-6 weeks[6]
For casted fractures
- Continue exercises as above.
- Limit supination and pronation.
- Change the long-arm cast to a short-arm cast (bridging callus indicates stability).
Following ORIF surgery
- Advance therapy with gentle AROM of the wrist and gentle opposition and flexion/extension exercises to the thumb.
- Continue elbow and shoulder exercises.
- Remove the short-arm cast at 6 weeks if the fracture appears to be radiographically healed.
- Use a wrist splint for protection.
Rehabilitation considerations in 8-12 weeks[6]
For casted fractures
- Remove the short-arm cast at 10-12 weeks if the fracture appears to be radiographically and clinically healed.
- A wrist splint may be used for protection
For casted fractures and following ORIF
- Consider pulsed electrical stimulation if no evidence of union is noted by 8 weeks, and consider surgery with bone grafting if progress is not observed by 12-14 weeks
- Advance therapy with gentle AROM of the wrist and with thumb exercises
- Begin grip strengthening with the use of silicone putty at 10 weeks
- Advance as tolerated to progressive resistive exercises (PREs)
The video below shows the brief cause, radiological views and management of the scaphoid fractures
Additional Resources[edit | edit source]
- Scott R. Laker et all, Scaphoid injury (Epidemiology), Medspace. 2015, 6 April. Level of evidence:5
- Phillips TG et al. Diagnosis and Management of Scaphoid Fractures, Am Fam Physician. 2004; 70(5): 879-884. Level of evidence: 5
Clinical Bottom Line[edit | edit source]
The scaphoid bone is the most commonly fractured carpal bone. Stress on the scaphoid, due to a forceful motion, may have a fracture as result (mostly due to a fall on an outstretched arm). The pain, which often is mild, is aggravated by pinching and gripping. The diagnoses can be differentiated by the location of tenderness, pain with certain maneuvers, and radiographic abnormalities. The length of immobilization affects negatively the outcomes. Internal fixation provided a satisfactory outcome for control of instability and early functional recovery of the wrist. There are different fractures types classified by Herbert and Fisher's system. To recognize these different fracture types, it is essential that adequate radiographs are taken of both wrists.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Gutierrez G, Office management of scaphoid fractures. Phys Sports Med. 1996;24:60–70.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 T. Grant Phillips et al, Diagnosis and Management of Scaphoid Fractures, Am Fam Physician. 2004 Sep 1;70(5):879-884.
- ↑ 3.0 3.1 3.2 Greene WB, Essentials of musculoskeletal care. 2d ed. Rosemont, Ill.: American Academy of Orthopaedic Surgeons, 2001:252–4.
- ↑ 4.0 4.1 Kawamura,K. & Chung, C.C. (2008). Treatment of Scaphoid Fractures and Nonunions. J Hand Surg Am. 2008 Jul-Aug; 33(6): 988–997. doi: 10.1016/j.jhsa.2008.04.026
- ↑ 5.0 5.1 5.2 5.3 5.4 Hayat Z, Varacallo M. Scaphoid Wrist Fracture. InStatPearls [Internet] 2019 Jan 4. StatPearls Publishing.Available from:https://www.ncbi.nlm.nih.gov/books/NBK536907/ (last accessed 23.3.2020)
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 6.7 6.8 Scott R. Laker et al, Scaphoid injury (Epidemiology), Medscape. 2019.
- ↑ 7.0 7.1 Mc Dermid, Patient Rating of Wrist Pain and Disability: A Reliable and Valid Measurement Tool, 1998.
- ↑ Bill Schloss Gillian Lieberman, MD, Scaphoid fractures, Harvard Medical School, Year Harvard Medical School, Year-IV. Januari 2001: pg 3. Level of evicence: 5
- ↑ 9.0 9.1 Bäcker HC, Wu CH, Strauch RJ. Systematic Review of Diagnosis of Clinically Suspected Scaphoid Fractures. J Wrist Surg. 2020 Feb;9(1):81-89. doi: 10.1055/s-0039-1693147. Epub 2019 Jul 21. PMID: 32025360; PMCID: PMC7000269.
- ↑ 10.0 10.1 Parvizi J, Wayman J, Kelly P, Moran CG. Combining the clinical signs improves diagnosis of scaphoid fractures. A prospective study with follow-up. J Hand Surg Br. 1998 Jun;23(3):324-7.
- ↑ 11.0 11.1 Clementson, M., Björkman, A., & Thomsen, N. (2020). Acute scaphoid fractures: guidelines for diagnosis and treatment. EFORT open reviews, 5(2), 96–103.
- ↑ Kawamura, K., & Chung, K. C. (2008). Treatment of scaphoid fractures and nonunions. The Journal of hand surgery, 33(6), 988–997.
- ↑ Fowler, C., Sullivan, B., Williams, L. et al. A comparison of bone scintigraphy and MRI in the early diagnosis of the occult scaphoid waist fracture. Skeletal Radiol 27, 683–687 (1998).
- ↑ Grewal R, Suh N, MacDermid JC. Is Casting for Non-Displaced Simple Scaphoid Waist Fracture Effective? A CT Based Assessment of Union. Open Orthop J. 2016 Sep 15;10:431-438.
- ↑ Schädel-Höpfner, M., et al. "Acute scaphoid fractures: Management under consideration of the new S3-level guideline." Der Orthopade 45.11 (2016): 945-950. (level of evidence 5)
- ↑ Medgeeks,Scaphoid Fractures-Don't miss this! Available from: https://youtu.be/ElD_Eh9fE9Q (Assessed 31 July 2020)