Running Mechanics for Clinicians
Original Editor - Mariam Hashem
Top Contributors - Mariam Hashem, Kim Jackson, Tarina van der Stockt, Jess Bell and Robin Tacchetti
This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work!
Overview of Running Injuries[edit | edit source]
Lower extremity running-related injuries range from 19.4 to 79.3 percent[1]. The most common injnuries are[2]:
- Patellofemoral pain
- Medial tibial stress syndrome (shin splints)
- Achilles tendinopathy
- Iliotibial band syndrome
- Plantar fasciitis
- Stress fractures of the metatarsals and tibia
Hamstrings and calf problems were reported by men marathon runners, while hip pain problems were common among women[3]. Most of these injuries have a high recurrence rates.
A 2015 systematic review[4] of 15 studies identified different risk factors for women and men:
| Women | Men contributing factors to tissue stress | |
|---|---|---|
| Age | History of previous injury | |
| History of previous sports activity | Running experience for 2 years | |
| running on a concrete surface | History of previous injury | |
| Participating in a marathon | Average weekly running distance (20–29 miles) | |
| weekly running distance (30–39 miles) | ||
| wearing running shoes for 4 to 6 months |
Stress Frequency Model[edit | edit source]
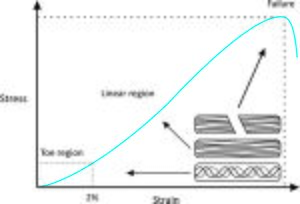
Running Injuries are caused by an inter-relation of multiple factors. A simple injury causation model using the stress frequency curve can help us to develop an idea on the contributing factors and how to address them in the management plan.
A tissue is influenced by the applied stress and the frequency of application. If the stress and it's frequency are below the injury threshold, the tissue will function normally within it's capacity. However, if either or both of these factors exceeded the injury threshold, the tissue is moer likely to be injured. This explains why some runners may not experience injury for long time and develop one as soon as they increase their frequency of training such as training for a marathon.
Considering stress and frequecny is important to understand individual tissue's capacity.
Running mechanics influence the stress applied to the body, magnitude, type (bending, shear or tension) and the speed of application on each foot contact. Assessing running mechanics leads us to think about the stressed structure and explains the presented symptoms. For example; landing on toes -forefoot strike- results in greater stresses on achillies tendons and the calf muscle forces.
Assessing frequency of running and training volume to understand the effect of the accumulated tissue stress . If falling below the tissue's threshold the likelihood of developing injury will be low and vice versa. Subjective examination can help us to understand the frequency, ask your client about them about their weekly training and what is your standard trainig like? How much running they do? what wa the frequency of applied stress before the injury occured?
the next thing is wehre is identifying the injury threashold which refers to the interaction between the tissue capacity to tolerate the stress an the tissue capacity to tolerate the frequncy of the applied stress. Tissue capacity refers to the functional capabilities of a specific tiussue to cope with stress type and frequency. A muscle capable of producing high peak force may be able to tolerate high level of stress on an individual foot contact. On the contrary , if the mscule's capability is low, applying stress with high frequency the muscle may not be able to cope well leading to injuries. To translate this into practical application, when assessing a runner we should think of adjusting the mechanical pattern or push up the tissue's endurance to tolerate the applied load. Lowering the applied stress by reducing the amoint of running can be a method of off-loading the injured tissue while building up the tissue resileince to cope with the functional aspiration.
Clinical Running Assessment Set Ups[edit | edit source]
Many of the common running-related biomechanical patterns can be identified by 2D analysis using inexpensive tools[1] such as a mobile phone or tablet camera. Satndaridizing the method of assessment is improtant for accuracy of identifying the patterns and to make sure your findings are not due to viewing angles.
Settings:
Tools/equipment: High speed camera or mobile phone/table camera and a tripod.
Distance: 1.5-2 meters from the treadmill
Height:0.8-1 meter-pelvic height
Views: side (saggital) and rear (frontal)
Timing: initial contact and mid-stance
Joints/regions: thorax, pelvis. hips, knees and ankles.
Follow a structured process of assessment by looking at one joint/region at a time. To end up with a structured problem list, slow down the speed of the camera to allow you to go backward and forward and take still pictures to draw lines and identify areas of stress.
Common Mechanical Patterns[edit | edit source]
Bramah et al found that similar mechanical patterns were associated with multiple injuries[6].
Looking from the saggital plan, we can identify the following patterns:
1- Foot Inclination Angle at Initial Contact:by drawing lines to compare the angle between the sole of the shoes and the treadmill. A great angle indicates greater foot inclination. It can potentially be caused by rear foot strike if the runner's toes are too high compared to the heel or a forefoot strike when the inclincation is mainly due to a high angle at the heel. Neither strikes are considered to be superior to the other. Landing with high inclination will limit the ability to engage in dorsiflexion which serves as shock absorption. High inclined foot will take longer time to get the foot flat on floor to start the shock absorption mechanics resulting in high impact vertical loading[7]. Fig 3 in the study by Souza RB shows how to identify foot inclination.
Conversely, landing with forefoot strike (on tip-toes) allows less time to engage in dorsiflexion utilizing the calf complex and possibly stressing the achillies tendon. Refer to this link to see the difference between different foot strike patterns.
In the management plan, a relatively low inclincation angle where foot is low to the ground regardless of the type of strike (heel or toe) minimzes the stress on achillies for forefoot runners or engage dorsiflexion for heelstrike runners.
2- Knee flexion angle:
Initial conact: draw a line straigh thruoogh femur, then down to floor. another one through lateral condyle of femur to laterl malleoulus. the greater the angle indicates more knee flexio. the smaller knee extension.
The injured runners tend to land with more knee extension at intial contact- influencing tissue stress- impact the ability to absorb shock. knee and ankle dunction as suspensions as you run, if you can land with knee in flexion and foot flat on floor you can start to engage you suspension spring form the moment you touch dow. that can serve as you move to the mid stance. running with extended knee and high inclined foot they are less likely to engage the shock absorption mechanism within knee and ankle- more higher shock , breaking forces as they land.
Mid stance: lines drawn across foot (floor- from malleouli up to epicondyle: dorsiflexion looking at line drawn from femur compare to shin line- knee flexion?
Mid stance: shock absorbed when hitting ground. Utilizing knee flexion to absorb shock.
Landing w extensio an dhigh inclined foot and has a huge range of flexion. using it to absorb shock, how it stresses tissue? Eccentric demand placed on quads in stance phase resulting to injury PFP, quads overloaded. conversely: hitting ground with small flexion, small dorsiflexion: poor ability to absorb shock- hear them on treadmill. minimal movment in knee ankle complex. suspension is not good- not absorbing shock- more forces to body- compensatory pattens on frontal plane: further injuroies. elevated shock: high impaact: global injury developmene+ s tress fracture. hear them on treadmill: poor ability to bed the knee. why they are not able to exccentrically absorb ? function prespective: gait training or strength prespective?
References[edit | edit source]
- ↑ Van Gent RN, Siem D, van Middelkoop M, Van Os AG, Bierma-Zeinstra SM, Koes BW. Incidence and determinants of lower extremity running injuries in long distance runners: a systematic review. British journal of sports medicine. 2007 Aug 1;41(8):469-80.
- ↑ Callahan LR, Sheon RP. Overview of running injuries of the lower extremity. UpToDate, Grayzel J.(Accessed on July 06, 2017). 2002.
- ↑ Fredericson M, Misra AK. Epidemiology and aetiology of marathon running injuries. Sports Medicine. 2007 Apr 1;37(4-5):437-9.
- ↑ Van der Worp MP, Ten Haaf DS, van Cingel R, de Wijer A, Nijhuis-van der Sanden MW, Staal JB. Injuries in runners; a systematic review on risk factors and sex differences. PLoS One. 2015 Feb 23;10(2):e0114937.
- ↑ How to get your running gait analysed. Available from: https://www.youtube.com/watch?v=gmBz3QC5JAg. [last access:06/10/2019]
- ↑ Bramah C, Preece SJ, Gill N, Herrington L. Is there a pathological gait associated with common soft tissue running injuries?. The American journal of sports medicine. 2018 Oct;46(12):3023-31.
- ↑ Souza RB. An evidence-based videotaped running biomechanics analysis. Physical medicine and rehabilitation clinics. 2016 Feb 1;27(1):217-36.