Rheumatoid Arthritis
Original Editors -Amanda Fetz & Katie Robertson from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Amanda Fetz, Riley Sturzebecher, Kim Jackson, Lucinda hampton, Amanda Ager, Admin, Aminat Abolade, Elaine Lonnemann, Wendy Walker, Shaimaa Eldib, Amrita Patro, 127.0.0.1, Katie Robertson, WikiSysop and Simisola Ajeyalemi
Definition/Description[edit | edit source]
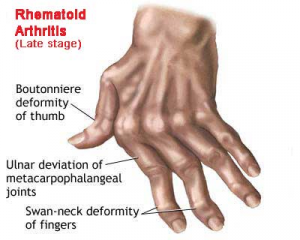
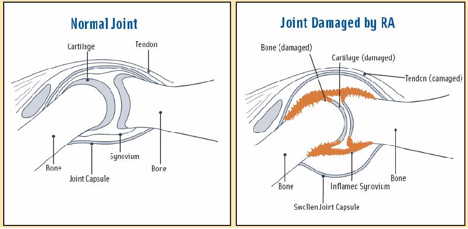
Rheumatoid arthritis (RA) is an autoimmune disease and a form of inflammatory arthritis that affects five or more joints. Autoimmune conditions occur when the body fights its own immune system. Instead of the immune system protecting the body, it attacks itself. In RA, the immune system attacks the lining of the joints, called the synovium. RA is a long-term disease that leads to inflammation of the joints and surrounding tissues and can also affect other organs. These tissues include tendon sheaths, bursa, and tendons. Symptoms may present as inflammation of joints, pain and fatigue, morning stiffness, and hot and warm joints that may be red. Furthermore, if not treated, RA can possibly lead to joint deformities in the later stages of the disease which then function of the joints could be lost permanently.
The disease course typically follows three possible paths:
a. Monocyclic: Having one episode that does not reoccur. This usually ends within 2-5 years of initial diagnosis.
b. Polycyclic: The disease severity varies over the course of the progression of the condition.
c. Progressive: Condition continues to become more severe and non-remitting.
Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Prevalence[edit | edit source]
The prevalence of Rheumatoid Arthritis is estimated between 1.5- 2.1 million US adults or 10 cases per every 1000 people. There are nearly three times as many women then men with the disease. RA is found all around the world, but does tend to be more prevalent in the Native American and white population.
The risk of RA increases with age. RA most commonly begins in women between the ages of 30 and 60. It often occurs later in life for men, but can happen at any age. When RA affects the pediatric population, it is called Juvenile Idiopathic Arthritis (JIA) and usually begins before the age of 16.
Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Characteristics/Clinical Presentation[edit | edit source]
Signs and Symptoms of RA:
- Joint Pain: warmth, redness, tenderness, swelling
- Joint Stiffness: increased in the mornings
- Fatigue throughout the body
- Fever
- Weight Loss
- Rheumatoid Nodules: small lumps of tissue felt under the skin
- Symmetrical Patterns of affected joints
- Most common joints: wrist, hand, fingers, cervical spine, shoulder, elbow, knee, hip, foot, and ankle
- Prolong symptoms
- Anemia
- Neck Pain
- Dry Eyes
- Dry Mouth
Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
| Class 1 | Completely able to perform usual activities of daily living (Self care, vocational and avocational) |
| Class 2 | Able to perform usual self care and vocational activates by limited in avocational |
| Class 3 | Able to perform usual self care activities but limited in vocational and avocational activities |
| Class 4 | Limited ability to perform usual self care, vocational, and avocational activities |
Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Associated Co-morbidities[edit | edit source]
RA has many effects on individuals including mortality, hospitalization, work disability, increase in medical cost/expenses, decreases of quality of life, and chronic pain. On average, the chronic RA patient has two or more comorbid conditions.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title This is significant because of the comorbidities effects on quality of life, functional status, prognosis and outcome.
Associated Co-morbidities:
a) Myocardial Infarction and Cardiovascular disease
b) Stroke
c) Peripheral Vascular Disease
d) Cancer (All)
e) Infection
f) Osteoporosis
g) GI disease
h) Psoriasis and other skin conditions
i) Cataract
Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Complications of RA:
Rheumatoid arthritis can affect nearly every part of the body. Even though the joints are most commonly affected, RA can also have effects on organs.
a) Damage to the lung tissue (rheumatoid lung)
b) Increased risk of hardening of the arteries
c) Spinal injury when the neck bones become damaged
d) Inflammation of the blood vessels (rheumatoid vasculitis), which can lead to skin, nerve, heart, and brain problems
e) Swelling and inflammation of the outer lining of the heart (pericarditis) and of the heart muscle (myocarditis), which can lead to congestive heart failure
f) Side effects from treatment and medication.
g) General deconditioning
h) Rheumatoid nodules
i) Vascular complications
j) Neurological complications
k) Cardiopulmonary complications
l) Ocular complications
Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Medications
[edit | edit source]
| Medication | Uses/ Effects | Side Effects |
| NSAIDs | Pain reliever | Stomach irritation Kidney function. Gastrointestinal problems |
| Acetaminophen | Pain reliever | If taken in excessive, liver damage may occur which could potentially lead to liver failure |
| Aspirin Buffered Plain | Decrease pain, swelling, inflammation | Upset stomach Tendency to bruise easily |
| Corticosteriods | Decrease inflammation, swelling, redness, itching, and allergic reactions |
Increased appetite Indigestion, Nervousness Restlessness |
| Methylprednisolone Prednisone |
Used for severe flare ups | Mood changes Easy bruising Increase risks of infections |
| Disease-modifying antirheumatic drugs (DMARDs) | Relieve painful, swollen joints and slow joint damage | May increase the risk of infection, hair loss, and kidney or liver damage |
| Azathioprine | Used for patients who have not responded to other medications | Cough or hoarseness Fatigue Abdominal issues |
| Cyclosporine | Used for patients who have not responded to other Medications | Increase Blood Pressure Kidney Problems Shaking/Trembling of hands |
| Leflunomide | Reduces signs and symptoms Slows down the process of degeneration of the joints. |
Abdominal pain, nausea, vomiting, loss of appetite, Sneezing Sore Throat |
| Methotrexate | Inhibits the metabolism of folic acid | Low white blood cell counts, abdominal pain, fever, infection |
| Sulfasalazine | Immunosuppressant | Abdominal pain, diarrhea, loss of appetite, nausea/vomiting Headache, sensitivity to light Aching joints |
| Biologic response modifiers | Block the autoimmune response that is involved in the roll with inflammation | Increase risk of infection |
| Tumor necrosis factor inhibitors | Blocks the autoimmune response that is involved in the roll with prolong inflammation as seen in RA | lymphoma, infections, congestive heart failure, and systemic side effects |
| Interleukin-1 inhibitor | Decreases inflammation in moderate-severe RA |
Abdominal Pain, Nausea, Vomiting, Headache |
| Selective costimulation modulator | Anti-inflammatory | Headache, dizziness, abdominal pain, dyspepsia, nausea, rash, flushing, urticaria, pruritus, and wheezing |
| CD20 antibody | Depletes B Cells that are associated with autoimmune response | Abdominal pain |
Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
Diagnostic Criteria
Four out of the Following Seven Must be Present
- Morning Stiffness for an hour or greater
- Arthritis of 3 or more of the following joints: right or left PIP, MCP, Wrist, Elbow, Knee, Ankle, and MTP Joint.
- Arthritis of wrist, MCP, PIP
- Symmetric involvement of a Joint
- Rheumatoid nodules over bony prominences or extensor surfaces or in juxaarticular regions
- Positive serum rheumatoid factor
- Radiographic changes including erosion or bony decalcifications localized in or adjacent to joints.
Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
| Test | Description | Purpose |
| C-reactive protein (CRP) (Lab Test) |
Blood Test | Indicates inflammation. As the level of inflammation rises, so does the level of CRP. High levels of CRP over a long period of time may indicate more severe joint damage. |
| Erythrocyte sedimentation rate, also referred to as ESR or "sed rate" (Lab Test) |
Blood Test | People with severe RA will generally have a higher ESR than one with less severe RA |
| Rheumatoid factor (RF) Lab Test |
Blood Test | Indicates the presence of RA. When the immune system attacks itself, the body produces RF. 75% of people with RA are RF positive. |
| Cyclic citrullinated peptide (CCP) Lab Test |
Blood Test | This test is usually given to people who are experiencing new symptoms of RA, in order to rule out other autoimmune diseases. |
| Bone Scans | Imaging | Detects inflammation |
| X-Ray | Imaging | Detects swelling of soft tissues and loss of bone density |
| Magnetic Resonance Imaging (MRI) | Imaging | Detects inflammation |
| Ultrasound | Imaging | Detects inflammation |
- There is no test that can determine for sure whether someone has RA. Most patients with RA will have some abnormal test results, although for some patients, all tests will be normal.
Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Etiology/Causes[edit | edit source]
Etiology
The cause of Rheumatoid Arthritis is unknown. RA occurs when the immune system attacks the synovium — the lining of the membranes that surround the joints. The resulting inflammation thickens the synovium, and can eventually invade and destroy the cartilage and bone within the joint. The tendons and ligaments that hold the joint together weaken and stretch, overtime. Gradually, the joint loses its shape and alignment.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
| Stage | Description |
| I: Early | 1. Early destructive changes on radiographic examination 2. Radiographic evidence of osteoporosis may be present |
| II: Moderate | 1. Radiographic evidence of osteoporosis, with or without slight subchondral bone destruction; slight cartilage destruction may be present 2.No joint deformities, although limitation of joint mobility may be present 3. Adjacent muscle atrophy 4. Extra-articular soft tissue lesions, such as nodules and tenosynovitis may be present |
| III. Severe | 1. Radiographic evidence of cartilage and bone destruction, in addition to osteoporosis 2. Joint deformity, such as subluxation, ulnar deviation, or hyperextension, without fibrous or bony ankylosis 3. Extensive muscle atrophy 4. Extra-articular soft tissue lesions, such as nodules and tenosynovitis may be present |
| IV. Terminal | 1. Fibrous or bony ankylosis 2. Criteria of Stage III |
Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Risk Factors:
Although there is no known cause for RA, it is believed that certain factors can increase an individual’s risk for developing RA due to the interaction between genetic factors and environmental exposures:
a) Smoking: A history of smoking is associated with a modest to moderate increased risk of RA onset.
b) Gender: The incidence of RA is two to three times higher in women than men.
c) Age: Rheumatoid arthritis can occur at any age, but it most commonly begins between the ages of 40 and 60.
d) Family History: Family history can indicate a higher risk for RA.
e) Reproductive and breastfeeding history
a. Live birth history: Women who have never had a live birth have a slight to moderately increased risk of RA.
b. Breastfeeding: Recent population based studies have found that RA is less common among women who breastfeed.
c. Menstrual history: Women with irregular menses or a shortened menstrual history have an increased risk of RA.
d. Oral contraceptives (OC): Women who had ever used OCs had a modest to moderate decrease in risk of RA.
Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Prognosis
The prognosis of RA depends on the severity of symptoms and early intervention. People with rheumatoid factor, the anti-CCP antibody, or subcutaneous nodules have a more severe form of the disease. People who develop RA at younger ages also tend to progress quicker.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
- 50% Disabled at work within 10 years
- 66% Significant trouble with ADL’s after 15 years
- Patients with severe RA may die 10-15 years earlier
Cite error: Invalid<ref>tag; name cannot be a simple integer. Use a descriptive title
Systemic Involvement[edit | edit source]
| Malignant | Hypertonic Osteoarthropathy, lymphoma, Leukemia, Carcinoma Polyarthritis |
| Hematologic | Sickle cell anemia, Thalassemia, Multiple Myeloma, Amyloidosis |
| Gastrointestinal | Whipple disease, primary biliary cirrhosis, Spondyloarthropathies, hemochromatosis |
| Endocrinopathies | DM, hypothyroidism, hyperthyroidism, hyperparathyroidism, acromegaly |
| Extra-articular Manifestations | Many of the extra-articular manifestations of RA are associated with increased disease activity and with markers of inflammation, such as high levels of rheumatoid factor (RF) and C-reactive protein (CRP). |
Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Medical Management (current best evidence)[edit | edit source]
The goal of medical management for RA is to prevent or control joint damage, prevent loss of function, and decrease pain.
Medications: See full list in <a href="http://www.physio-pedia.com/RA_(Rheumatoid_Arthritis)#Medications">medication section</a>
- Disease-modifying antirheumatic drugs (DMARDs)- Slow the progression of rheumatoid arthritis and save the joints and other tissues from permanent damage.
- Immunosuppressants- Control the immune system
- TNF-alpha inhibitors- Inhibit the inflammatory substance produced by the body and help reduce pain, morning stiffness, and tender or swollen joints.
- Other drugs- Target a variety of processes involved with inflammation in your body
<span class="fck_mw_ref" _fck_mw_customtag="true" _fck_mw_tagname="ref" name="3" />
Surgical Treatment: If medications fail to prevent joint damage, surgical intervention may be needed to repair the joints, restore ability, decrease pain, and correct deformities.
- Total Joint Replacement
- Tendon Repair
- Joint Fusion
<span class="fck_mw_ref" _fck_mw_customtag="true" _fck_mw_tagname="ref" name="4" />
Supplements: Research suggests that there are vitamins and minerals which may have an effect on RA. These effects range from reducing joint inflammation to improving bone health. Some of the vitamins and minerals are listed below. It is recommended to consult your primary care physician before consuming any of the supplements listed below.
- Calcium
- Copper
- Fluoride
- Iron
- Magnesium
- Selenium
- Vitamin A
- Vitamin B-1
- Vitamin B-12
- Vitamin B-3
- Vitamin B-6
- Vitamin D
- Vitamin K
- Zinc
[2]
Physical Therapy Management (current best evidence)[edit | edit source]
Goals and Expected Outcomes
- Decrease pain
- Decrease joint swelling or inflammation
- Increase or maintain strength
- Improve joint integrity and stability
- Improve range of motion
- Improve endurance for functional activities
- Independence for ADL’s
- Safe and efficient gait
- Improve functional mobility
- Increase in quality of life
- Self management
Interventions:
- Range of Motion/ Flexibility: Range-of-motion exercises and exercise programs can delay the loss of joint function and help keep muscles strong.
- Modalities: Heat, ice, massage, ultrasound, hydrotherapy, and electrical stimulation may be used to reduce pain and improve joint movement.
- Joint protection: Assistive devices, splints or orthotic devices to support and align joints may be very helpful.
- Energy Conservation: Frequent rest periods between activities, as well as 8 to 10 hours of sleep per night, are recommended.
- Aerobic Endurance: aerobic capacity/endurance conditioning,
- Therapeutic exercise: gait training, aquatic programs, range of motion techniques, stretching, strength, power and endurance training
- Functional Training: ADLs, task adaptation, injury prevention
- Manual Therapy: passive range of motion, soft tissue mobilization
- Patient Education
- Lifestyle changes (Physical activity, dietary, and emotional changes)
Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
| Benefit | Type | Prescription |
| CV Health | Cycling, walking, swimming, dance | 60-80% HR Max, 30-60 min/session, 3-5 days a week; Increase duration, then intensity over time |
| Muscle Mass and Strength | Free weights, weight machines, therabands | 60-80% 1RPM, 8-10 exercises (large muscle groups), 8-12 repetitions, 2-3 sets, increase intensity over time |
| ROM and Flexibility | Stretching, Tai Chi, Yoga/Pilates | 10-15 minutes, 2 days a week |
| Balance | One leg stance, stability ball, strengthening core muscles | Regular basis |
Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Adult Rheumatoid Arthritis Physical Therapy Practice Patterns
4A: Primary Prevention/Risk Reduction for Skeletal Demineralization (low bone density)
4B: Impaired Posture (cervical involvement)
4C: Impaired Muscle Performance
~4D: Impaired Joint Mobility, Motor Function, Muscle Performance, and Range of Motion Associated with Connective Tissue Dysfunction
4H: Impaired Joint Mobility, Motor Function, Muscle Performance, and Range of Motion Associated with Joint Arthroplasty
4I: Impaired Joint Mobility, Motor Function, Muscle Performance, and Range of Motion Associated with Bony or Soft Tissue Surgery ( tenosynovectomy, tendon reconstruction)
5H: Impaired Motor Function, Peripheral Nerve Integrity, and Sensory Integrity Associate with Nonprogressive Disorders of the Spinal Cord (cervical spine)
6B: Impaired Aerobic Capacity/Endurance Associated with Deconditioning
~Most Commonly used practice pattern for RA
Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Management of flare ups:
People who are diagnosed with RA also may experience a phenomenon that is called an “flare up” of the condition. Research suggests that these flare ups usually happen after experiencing a secondary illness, being involved in a high stress situation, overexerting oneself, . What triggers flare ups is currently still unknown. Current evidence suggests some strategies that can help someone who is experiencing a flare up by reducing pain, inflammation, and improve their quality of life:
- Balance is key, schedule plenty of down time to reduce the likelihood of affected joints from becoming flared up
- Educate family, staff at work, and other people who you interact with, they can help you during flare ups
- Have a backup plan, be prepared in case of a flare up and become familiar with warning signs of a flare up
- Practice relaxation and self calming strategies: Research suggests that regularly practicing these relaxation techniques can reduce stress and lead to a reduction in pain.
- Use modalities such as a cold pack or hot pack: Both of these have various effects on tissues which research suggests can be beneficial in reducing inflammation and pain during a flare up
- Lastly, corticosteroid injections can be used to reduce inflammation and reduce pain in a flared up joint
[2]
Outcome Measures
- Rheumatoid Arthritis Disease Activity Index (RADAI-5): A self-reported outcome measure that consists of 5 questions in a Likert scale format that briefly surveys the patient regarding their views of their condition (both over the past 6 months and current status).
- Disabilities of the Arm, Shoulder and Hand (DASH): The DASH is a patient-reported outcome measure that evaluates function of the upper extremities, and can be used to examine change over time.
- Short Form-36 (SF36): A patient reported outcome measure that is designed to evaluate quality of life through measures such as physical functioning, role limitations due to physical or emotional problems, and general mental health.
- Fatigue Severity Scale: A 9-item questionnaire that rates the patient’s fatigue and how it interferes with activities such as work or social life.
[14] [15]
Differential Diagnosis[edit | edit source]
A) Fibromyalgia
B) Lyme Disease
C) Myelodysplastic syndrome
D) Osteoarthritis
E) Paraneoplastic syndrome
F) Polychondritis
G) Polymyalgia Rheumatica
H) Psoriatic arthritis
I) Sarcoidosis
J) Sjogren Syndrome
K) Systemic Lupus Erythematous
L) Reiter Syndrome
M) Gout
Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Case Reports/ Case Studies
[edit | edit source]
1. Fischman A, Abeles M, Zanetti M, Weinstein A, Rothfield N. The coexistence of rheumatoid arthritis and systemic lupus erythematosus: a case report and review of the literature. The Journal Of Rheumatology [serial on the Internet. (1981, May), [cited March 3, 2013]; 8(3): 405-415. Available from: MEDLINE.]
2. McKendry R, Huebsch L, Leclair B. Progression of rheumatoid arthritis following bone marrow transplantation. A case report with a 13-year followup. Arthritis And Rheumatism [serial on the Internet. (1996, July), [cited March 3, 2013]; 39(7): 1246-1253. Available from: MEDLINE.]
3. Krishnadas R, Krishnadas R, Cavanagh J. Sustained remission of rheumatoid arthritis with a specific serotonin reuptake inhibitor antidepressant: a case report and review of the literature. Journal Of Medical Case Reports [serial on the Internet. (2011, Mar 19), [cited March 3, 2013]; 5112. Available from: MEDLINE.]
4. Stolt P, Bengtsson C, Nordmark B, Lindblad S, Lundberg I, Alfredsson L, et al. Quantification of the influence of cigarette smoking on rheumatoid arthritis: results from a population based case-control study, using incident cases. Annals Of The Rheumatic Diseases [serial on the Internet. (2003, Sep), [cited March 3, 2013]; 62(9): 835-841. Available from: MEDLINE.]
5. Ben Dhaou B, Boussema F, Aydi Z, Baili L, Kochbati S, Rokbani L. [Rheumatoid arthritis in the elderly: ten cases report. La Tunisie Médicale [serial on the Internet]. (2012, June), [cited March 3, 2013]; 90(6): 442-445. Available from: MEDLINE.]
6. Källberg H, Jacobsen S, Bengtsson C, Pedersen M, Padyukov L, Alfredsson L, et al. Alcohol consumption is associated with decreased risk of rheumatoid arthritis: results from two Scandinavian case-control studies. Annals Of The Rheumatic Diseases [serial on the Internet. (2009, Feb), [cited March 3, 2013]; 68(2): 222-227. Available from: MEDLINE.]
Resources
[edit | edit source]
1. Rheumatoid Arthritis: Help to understand Rheumatoid Arthritis:
http://www.rheumatoidarthritis.com/ra/diagnosing-ra/default.htm
2. Rheumatoid Arthritis: Frequently asked Questions:
http://www.rheumatoidarthritis.com/ra/additional-resources/faq.htm
4. Rheumatology Check List Visit
http://www.rheumatoidarthritis.com/ra/WebResources/pdf/VisitChecklist.pdf
5. The RA Symptom Tracker Sheet
http://www.rheumatoidarthritis.com/ra/WebResources/pdf/SymptomTracker.pdf
6. The Arthritis Organization
http://www.arthritis.org
7. American College of Rheumatology Patient Education
http://www.rheumatology.org/
8.Self-help
http://www.aidsforarthritis.com/
9. RA Treatment
http://www.ra.com/ra-treatment.aspx
10. American College of Rheumatology
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
References[edit | edit source]
see adding references tutorial.