Radiation Side Effects and Syndromes: Difference between revisions
No edit summary |
No edit summary |
||
| Line 22: | Line 22: | ||
# External beam radiotherapy (EBRT) where a medical linear accelerator (linac) directs ionising radiation at the tumour from outside the body eg | # External beam radiotherapy (EBRT) where a medical linear accelerator (linac) directs ionising radiation at the tumour from outside the body eg | ||
** Conventional Radiation Therapy. This refers to the old techniques of radiation therapy where treatments would be planned by defining a limited number of beams with the boundaries delineated on orthogonal x-rays of the patient. It has been largely replaced by other highly conformal external beam radiation therapies, which use CT images to plan the treatment.<ref>Radiopedia [https://radiopaedia.org/articles/conventional-radiation-therapy?lang=gb CRT] Available from:https://radiopaedia.org/articles/conventional-radiation-therapy?lang=gb (last accessed 25.8.2020)</ref> Examples of these newer techniques include: three-dimensional conformal radiation therapy (3D-CRT); intensity-modulated radiation therapy (IMRT); stereotactic radiosurgery; electron therapy; particle (hadronic) therapy.<ref name=":0" /> | ** Conventional Radiation Therapy. This refers to the old techniques of radiation therapy where treatments would be planned by defining a limited number of beams with the boundaries delineated on orthogonal x-rays of the patient. It has been largely replaced by other highly conformal external beam radiation therapies, which use CT images to plan the treatment.<ref>Radiopedia [https://radiopaedia.org/articles/conventional-radiation-therapy?lang=gb CRT] Available from:https://radiopaedia.org/articles/conventional-radiation-therapy?lang=gb (last accessed 25.8.2020)</ref> Examples of these newer techniques include: three-dimensional conformal radiation therapy (3D-CRT); intensity-modulated radiation therapy (IMRT); stereotactic radiosurgery; electron therapy; particle (hadronic) therapy.<ref name=":0" /> | ||
2. Sealed source radiotherapy (brachytherapy) where a radiation source(s) is placed, under the guidance of imaging, within or next to the area requiring treatment. | 2. Sealed source radiotherapy (brachytherapy) where a radiation source(s) is placed, under the guidance of imaging, within or next to the area requiring treatment. | ||
3. Unsealed source radiotherapy (systemic radioisotope therapy) where a radioisotope is delivered through: infusion e.g. for neuroendocrine tumours ; ingestion e.g for thyroid cancer.<ref name=":0" /> | 3. Unsealed source radiotherapy (systemic radioisotope therapy) where a radioisotope is delivered through: infusion e.g. for neuroendocrine tumours ; ingestion e.g for thyroid cancer.<ref name=":0" /> | ||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
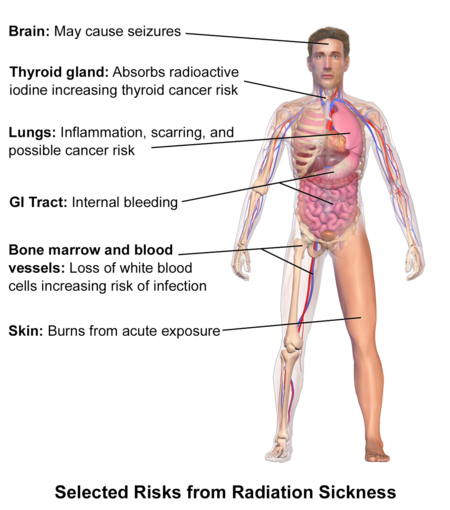
[[File:Radiation Sickness.png|right|frameless|510x510px]] | |||
'''Side Effects''' | '''Side Effects''' | ||
Revision as of 08:05, 25 August 2020
Original Editors -Alicia Dupilka & Kristin Gramling from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Kristin Gramling, Alicia Dupilka, Lucinda hampton, Vidya Acharya, Kim Jackson, Admin, Elaine Lonnemann, WikiSysop, 127.0.0.1 and Wendy Walker
Definition/Description[edit | edit source]
Radiation therapy, or radiotherapy, is a common oncologic treatment modality utilising ionising radiation to control or eliminate malignant cells. Radiotherapy may be used alone, or synergistically with chemotherapy or immunotherapy. The type of radiation therapy employed depends on the disease and the specific type of cancer being treated.
Radiotherapy plays a part in:
- Primary curative treatment (eg. head and neck cancer),
- Adjuvant therapy (e.g. reducing recurrence rate after local breast cancer surgery)
- Palliation of cancer symptoms (e.g. reducing pain from bone metastases).
- Treating non-malignant disease, e.g. Graves thyroiditis, keloid scarring.[2]
- Nearly two-thirds of all cancer patients will receive radiation therapy [3]
- There are no good estimates of how many of these patients will develop complications due to the radiation therapy [4]
Techniques[edit | edit source]
Radiotherapy is customarily divided into three main categories:
- External beam radiotherapy (EBRT) where a medical linear accelerator (linac) directs ionising radiation at the tumour from outside the body eg
- Conventional Radiation Therapy. This refers to the old techniques of radiation therapy where treatments would be planned by defining a limited number of beams with the boundaries delineated on orthogonal x-rays of the patient. It has been largely replaced by other highly conformal external beam radiation therapies, which use CT images to plan the treatment.[5] Examples of these newer techniques include: three-dimensional conformal radiation therapy (3D-CRT); intensity-modulated radiation therapy (IMRT); stereotactic radiosurgery; electron therapy; particle (hadronic) therapy.[2]
2. Sealed source radiotherapy (brachytherapy) where a radiation source(s) is placed, under the guidance of imaging, within or next to the area requiring treatment.
3. Unsealed source radiotherapy (systemic radioisotope therapy) where a radioisotope is delivered through: infusion e.g. for neuroendocrine tumours ; ingestion e.g for thyroid cancer.[2]
Characteristics/Clinical Presentation[edit | edit source]
Side Effects
Depend on the area of the body being treated, dose given per day, total dosage, general medical condition and other treatments being given.
- Acute radiation injury
- Nausea, malaise, dysphagia, vomiting immediately following irradiation
- Erythema
- Mucosal inflammation (stomatitis, esophagitis, enteritis, etc.)
- Bone marrow damage: anemia, thrombocytopenia, and/or leukocytopenia (pancytopenia)
- Infection due to immunocompromise
- Early radiation-induced lung injury (radiation pneumonitis): Dyspnea, dry cough, hemoptysis, and fever may occur several weeks following radiation.
- Partial respiratory insufficiency is an early sign.
2. Chronic radiation damage
- Late radiation-induced lung injury (radiation fibrosis)
- Bone: fractures
- Bone marrow damage: anemia, thrombocytopenia, and/or leukocytopenia (pancytopenia); Infection due to immunocompromise
- Heart: increased risk of myocardial infarction
- Gastrointestinal: impaired function
- Thyroid: impaired function (hypothyroidism)
- Impaired fertility: Fibrosis in ovaries involving amenorrhea; Azoospermia
- Radiation of the head: Leukoencephalopathy; Hormone imbalances and their outcomes, such as stunted growth due to low growth hormone levels
- Xerostomia
- Malignancies: especially leukemias, MDS, lymphoma, thyroid cancer[6]
Lymphedema[7][edit | edit source]
• Swelling that occurs when protein-rich lymph fluid accumulates in the interstitial tissue
• May contain plasma proteins, extravascular blood cells, excess water, and parenchymal products
• Often insidious
• Characteristics
o Non-pitting swelling of either the arm or leg and usually involves the digits
o Early stages: manifest pitting edema until fibrosis develops
o May predispose to recurrent skin infections
• Complaints
o Heaviness or fullness of the limb
o Tight sensation of the skin
o Decreased flexibility
o Ambulation may be affected
• Risk factors
o Undergoing axillary surgery/radiation therapy
o Extent of local surgery
o Local radiation
o Delayed wound healing
o Tumor causing lymphatic obstruction
o Scarring of the left or right subclavian lymphatic ducts
• Grades
o Grade 1: 5-10% interlimb discrepancy in volume or circumference, pitting edema
o Grade 2: >10-30% interlimb discrepancy in volume or circumference, obliteration of skin folds, readily apparent deviation from normal contour
o Grade 3: >30% interlimb discrepancy in volume; lymphorrhea; gross deviation from normal contour interfering with activities of daily living
o Grade 4: progression to malignancy, amputation indicated, disabling
Radiation Fibrosis Syndrome[4][edit | edit source]
- Progressive fibrotic tissue sclerosis resulting from radiation treatment
- It affects many different types of tissue including skin, muscle, ligaments, tendons, nerves, heart, lung, gastrointestinal and genitourinary tract, and bone; in order for a structure to be considered affected by this syndrome, it must be within the radiation field or have tendons, neurovascular innervation or lymphatic flow that travels in the field.
- The pathophysiology behind the sclerosis, fibrosis and atrophy is not well understood. Some believe there is a link between vascular endothelial damage and the progression of the fibrosis. When endothelial cells are damaged by radiation they can no longer get rid of the surrounding thrombin causing a profibrogenic effect on smooth muscle cells, fibroblasts, myofibroblasts and other cells.
- Problems may not present for several months or years after treatment
- Usually has a slow, insidious onset and is not reversible
Risk Factors:[edit | edit source]
- Hodgkin lymphoma
- Age
- Overall health
- Degenerative spine disease
- Exposure to chemotherapy treatment
- Location of radiation
Head and neck cancer, because high doses are needed and there are many vital tissues in that radiation field
- Size of radiation field
- Type of radiation and time since radiation was administered
- Neuropathic pain due to RFS is more likely to occur in those with pre-existing medical disorders involving the nervous system such as diabetes, spinal degeneration and cervical radiculopathy
Structures Affected:[edit | edit source]
Nerve[edit | edit source]
Peripheral Nervous System (PNS): Pain, sensory loss and weakness caused by external compressive fibrosis of soft tissue and ischemia from fibrosis.
Central Nervous System (CNS): Autonomic Nervous System can be affect resulting in orthostatic hypotension, bowel and bladder changes, and sexual dysfunction
Neuropathic pain involving both the PNS and CNS is common. It is due to damage of neural structures within the field of radiation.
Sensory loss is also common including loss of light touch, pain, temperature, vibration and position sensation
Weakness due to damage of neural structures, including plexopathy and mononeuropathies.
Muscle[edit | edit source]
Painful spasms are common due to myopathies, weakened and fatigability of muscles and ectopic activity of the motor nerve
Localized muscle pain due to sensitization of local pain neurons
Tendon and Ligaments[edit | edit source]
Progressive fibrosis and sclerosis causing decreased elasticity, shortening and contractures
Effects do not always have to be direct. Radiation to the upper leg can cause ankle contractures because the muscles, tendons and vascular structures of the ankle run of the length of the leg.
Bone[edit | edit source]
Decreased bone density
Osteoradionecrosis of the mandible and fractures of the pelvis, hip, long bones and ribs are common
Radiation in children may cause long bones and the spine to mature abnormally if the growth plate is affected
Common Clinical Syndromes Associated with RFS:[edit | edit source]
- Neck Extensor Weakness- severe atrophy of the cervicothoracic paraspinal and shoulder girdle musculature resulting from damage to the motor nerve and/or the muscle itself
- Shoulder Pain and Dysfunction - damage to the cervical nerve roots, brachial plexus, rotator cuff (RTC) muscles, rhomboids, and peripheral nerves innervating these muscles all contributes to this dysfunction. May result in RTC tendonitis and adhesive capsulitis
- Cervical Dystonia - usually involving the SCM, scalenes, and trapezius. If severe it can affect swallowing, phonation and activities of daily living.
- Trismus - impaired mouth opening can result from the invasion of the tumor into the masseter and pterygois muscles, the innervation of these muscles, or the TMJ. It can affect chewing, swallowing, oral hygiene and pulmonary function.
Associated Co-morbidities[edit | edit source]
- Lymphedema[8]
- Cardiac insufficiency
- Venous insufficiency
- Arthritis
- Fungal infection
- Cellulitis
- Psychosocial complications
- Lymphatic cysts
Other Co-morbidities [9]
These co-morbidities can have an effect on how radiation is tolerated:
- Diabetes
- Heart Disease
- Arthritis
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
Lymphedema[7][edit | edit source]
• Clinical assessment
• Lymphoscintigraphy: imaging of the lymphatic system
• Magnetic Resonance Imaging: complement lymphoscintigraphy, provide detail about anatomy and nodes
• Circumferential upper-extremity measurement: most widely used to diagnose upper extremity lymphedema
Radiation Fibrosis Syndrome[edit | edit source]
Diagnostic criteria is dependent on area of radiation and what structures are affected.
Etiology/Cause[3][edit | edit source]
Risk Factors:
Dependent on organ radiated, individual tolerance, tumor type, volume radiated and fraction size/dosage.
Neurotoxicity[edit | edit source]
- High total dose and fractionation dose
- Large volume radiated
- Increased edema
- Age <12 or >60 years
- Concurrent chemotherapy
- Underlying diseases affecting the vascular structures (Diabetes, HTN)
- Stereotactic radiation surgery and brachytherapy (internal radiation)
Dermatitis[edit | edit source]
- Total dose/volume and fractionation dose
- Surface area exposed
Acute Enterocolitis[edit | edit source]
- Large volume
- High total dose and fractionation dose
- Concurrent chemotherapy
Chronic Enterocolitis[edit | edit source]
- Older age
- Postoperative radiation
- Presence of collagen vascular disease
- Concurrent chemotherapy
- Poor radiation technique
Pulmonary[edit | edit source]
- Older age
- Lower performance status
- Lower pulmonary baseline function
- Large volume treated
Systemic Involvement [3][edit | edit source]
Gastrointestinal[edit | edit source]
Radiation Esophagitis: often involved in radiation treatment for lung cancer especially when a chemosensitizer is also used. Symptoms usually resolve in 1 to 3 weeks after radiation is finished.
Symptoms: abnormal peristalsis, odynophagia (pain with swallowing) and dysphagia
Radiation Enterocolitis: often results in fibrosis leading to strictures in the intestines, bowel obstruction, fistulas with abscess formation, ulceration with bleeding and malabsorption
Acute Radiation Enteritis - decreases the surface area of absorption leading to decreased nutritional uptake and possible dehydration and malnutrition. Symptoms: diarrhea, abdominal cramping, and nausea
Chronic Radiation Enteritis - symptoms don't occur for 6 months to 25 years after treatment and usually require more serious treatment
Other symptoms may include dry mouth, anorexia, and stomatitis (inflammation of mouth mucosa)
Pulmonary[edit | edit source]
Radiation Lung Disease
Radiation Pneumonitis (acute): interstitial inflammation creating a decrease in the amount of gas exchanged in the lungs. It can occur 1 to 6 months after radiation and usually resolves in 6 to 12 months. Symptoms: dry cough with dyspnea on exertion or can turn into a severe cough with dyspnea at rest
Radiation fibrosis (chronic): progressive and occurs months after radiation treatment
Other problems may include bronchopleural fistulas, pneumothorax, hemoptysis and bronchial stenosis
Cardiovascular[edit | edit source]
Radiation Heart Disease - may result in pericarditis, coronary heart disease, myocardial disease and aortic-valve disease
Musculoskeletal[edit | edit source]
Connective Tissue Involvement - late changes such as fibrosis, atrophy and contraction is common especially in collagen
- In bones and limbs it can cause weakness, limb-length discrepancies and scoliosis
- It can result in edema and decreased range of motion
- It can cause pelvic adhesions that result in painful motion and sometimes plexopathy
- In the circulatory and lymphatic system it can cause loss of elasticity on contractility of vessels. Even though the actual lymph vessels may maintain their shape, fibrosis in the surrounding tissue can inhibit growth of the vessels into tissues that need to be healed.
Nervous System [edit | edit source]
Acute symptoms: occur during treatment and include debilitating fatigue; cranial radiation may result in short-term memory loss, changes in behavior and cognition, decreased appetite, dry skin, hearing loss, hair loss and decreased salivation
Subacute symptoms: occur 1 to 4 months after treatment and are not as common. Radiation to the cervical spine may result in subacute myelopathy (Lhermitte's sign). Radiation to the brainstem may result in ataxia, nystagmus and dysarthria
Chronic symptoms: occur months to years after therapy and can include damage to the cerebral vasculature leading to coronary artery disease, transient ischemic attacks, stroke or myocardial infarction.
Radionecrosis - results from whole-brain radiotherapy. Secondary tumors may develop and the hypothalamic system may be affected. Symptoms: headache, changes in cognition and personality, focal neurological deficits and seizures.
Myelopathy - results from radiation of the spinal cord. May present as Brown-Sequard syndrome or motor neuron syndrome.
Plexopathy - results from damage to the brachial and lumbar plexuses. Symptoms may include paresthesias, motor deficits, lymphedema and pain.
Integumentary[edit | edit source]
Radiation Dermatitis - common since it is involved in most radiation therapy
Acute
Grade 1: resembles a sunburn. Hair follicles and sebaceous glands are damaged and may result in hair loss, pruritis, desquamation, depigmentation and scaling due to damage of the hair follicles
Grade 2: persistent erythema or patchy moist desquamation in creases of the skin that is usually painful with some edema
Grade 3: moist desquamation with pitting edema not confined to skin creases
Grade 4: skin necrosis or ulceration of dermis with bleeding
Consequential-late: acute changes that are persistent
Chronic: develop months to years after radiation treatment; may include skin scarring, contractures (atrophic skin susceptible to tearing and ulceration), and secondary malignancies
Other problems may include destruction of nails, delayed wound healing and epidermolysis (loose skin)
Medical Management (current best evidence)[edit | edit source]
Clinical trials to learn how to use radiation therapy more safely and effectively are being conducted by doctors and scientists. [6]
Working on improving image-guided radiation. [6]
Research is also being done on radiosensitizers and radioprotectors. [6]
The use of carbon ion beams is still being investigated and remain experimental. This type of therapy are not currently available in the US. [6]
Treatment of Common Clinical Syndromes associated with RFS[4][edit | edit source]
These treatments are usually used in conjunction with physical therapy or after conservative/rehabilitative treatments have failed
- Neck Extensor Weakness - cervical orthotics, nerve stabilizing medications such as pregabalin, gabapentin or duloxetine, and local anaesthetic injection into tender points
- Shoulder Pain and Dystonia - anti-inflammatory and/or nerve stabilizing medications and subacromial injection with steroids and anaesthetic
- Cervical Dystonia - nerve stabilizing medications, opioids and botulinum toxin injection
- Trismus - forced mouth opening under general anesthetic for short-term effects, surgical coronoidectomy, botulinum toxin injection, and jaw opening devices
Medications
- Radioactive iodine
- Ibritumomab tiuxetan (Zevalin®)
- Combined tositumomab and iodine I 131 tositumomab (Bexxar®)
- Samarium-153-lexidronam (Quadramet®)
- Strontium-89 chloride (Metastron®)
- Amifostine is the only drug approved by the FDA to protect normal tissues (radioprotector)[6]
- It can be used to reduce the frequency and/or severity of radiation-induced esophagitis[3]
Physical Therapy Management (current best evidence)[edit | edit source]
Physical therapists should always wash their hands before treating a patient who has undergone radiation therapy to protect that client from possible infection.[3]
Skin Care[3][edit | edit source]
- Avoid use of alcohol/drying agents, lotion, gel, or oil. Creams and gels can increase the dosage received on the skin and increase the likelihood of side effects
- Do not wash away markings of the targeted area
- Position the patient so they are not lying on the targeted area
- Avoid exposing the patient to sources of heat, including direct sunlight and modalities
- Monitor wound healing
Musculoskeletal [3][edit | edit source]
- If adhesions are present in the hip after radiation of the pelvis, be sure to incorporate range of motion activities; early intervention is important to prevent contractures and restrictive scarring.
- Post-radiated tissue can tear when stretching so it is important to observe for blanching of the skin during stretching and not to stretch beyond that point. Stretching should be continued 18 to 24 months after radiation therapy has been discontinued.
Nervous System [3][edit | edit source]
- Anyone with neurological signs or symptoms of an unknown cause should be asked about a previous history or cancer and radiation therapy
Infection[3][edit | edit source]
- Therapists should observe carefully for signs of infection in patients who have undergone radiation treatment. The first and only sign may be a fever because the patient may be immunosuppressed and their body cannot create a normal inflammatory response.
Exercise [3][edit | edit source]
- A successful protocol should include patient education, exercise evaluation and an individualized exercise prescription. - Therapists must monitor vital signs in patients who have undergone radiation treatment because radiation and chemotherapy can leave the lungs and heart tissue permanently scarred. Patients should be taught to monitor their own vitals including heart rate, respiration rate and rate of perceived exertion (should not exceed 15 to 17) and taught to detect signs of complications such as dyspnea, pallor, excessive perspiration, or fatigue while exercising. Patients should be told not to exercise within 2 hours of chemotherapy or radiation therapy because it increases the circulation and may increase the effects of the treatment.
- Studies have shown low to moderate intensity aerobic exercise during the same weeks of radiation treatment can help improve physical function and lower subjective levels of fatigue, anxiety, depression and sleep disturbances.
Lymphedema [7][edit | edit source]
• Exercise has a different effect on the body at lower doses than it does at higher doses
• Extreme exercise would promote inflammation and injury and should be avoided
• Slowly, progressive, carefully controlled increases in stress on a limb may actually provide protection
• Individuals at risk and with lymphedema should be evaluated by a certified lymphedema therapist
Management of Syndromes Associated with Radiation Fibrosis Syndrome[4][edit | edit source]
Physical Therapy is usually the first line of treatment for the dysfunctions listed below.
- Neck Extensor Weakness - emphasize postural retraining through core strengthening, flexibility of the shoulder musculature, and strengthening the cervicothoracic and rotator cuff muscles. This will help reduce energy demands and pain. It is also important to develop a long-term home exercise program
- Shoulder Pain and Dystonia - treated through conservative measures because shoulder surgery should be avoided in patients with RFS because damage of the neruomuscular structures often results in poor surgical outcomes. Work on core strength and posture, neck extensor and rotator cuff strength and stretching of pectoral girdle musculature in order to try to restore normal anatomical alignment of the shoulders. There is a potential long-term benefit if the patient consistently follows a home exercise program.
- Cervical Dystonia - the goal is to restore and maintain neck range of motion and a long-term home exercise program should be utilized.
- Trismus - Literature is limited but a variety of jaw-opening devices are available to help treat trismus.
Differential Diagnosis[edit | edit source]
Lymphedema[edit | edit source]
| Disorder |
Definition |
Signs and Symptoms |
| Deep Vein Thrombosis[10] |
-Blood clot in the leg. |
-Tenderness -Leg pain -Swelling (Difference of 1.4 cm in men and 1.2 cm in women) -Warmth -Subcutaneous venous distension -Discoloration |
| Hypoalbuminemia[11][12] |
-Low level of albumin (serum-binding protein). -Common problem among persons with acute and chronic medical conditions |
-Swelling -Loss of appetite -Muscle weakness, fatigue, cramps -Pleural effusion -Ascites |
| Renal Failure[13] |
-Failing of the kidneys. |
-Decreased urine output -Fluid retention, swelling -Fatigue -Confusion -Nausea |
| Lipedema[3] |
-Symmetrical swelling of both legs, extending from the hips to the ankles caused by deposits of subcutaneous adipose tissue. |
-Fatty bulges in the medial proximal thigh and the medial distal thigh just above the knee -Feet not affected -Pitting edema relieved by prolonged elevation |
| Baker Cyst[3] |
-Subtype of ganglion that often communicates with a joint space. -Most often palpated behind the knee. |
-Rupture of the cyst or hemorrhage from the joint into the cyst causes severe pain -Swelling below the lesion. |
| Idiopathic Edema[14] |
-Syndrome of real or perceived excessive weight gain. |
-Bloating and swelling -Decreased blood volume -Edema around the eyes |
| Congestive Heart Failure[10] |
-Physiologic state in which the heart is unable to pump enough blood to meet the metabolic needs of the body at rest or during exercise. -Also called cardiac decompensation or cardiac insufficiency. |
Left Ventricular Failure
-Orthopnea |
| Neurofibromatosis[3] |
-Involves the nervous system, muscles, bones, and skin. |
-Characterized by multiple soft tumors over the entire body associated with areas of pigmentation. |
| Erysipelas[3] |
-Type of cellulitis that may cause an acute infection of the skin with sharply defined borders. |
-Accompanied by fever and chills -Very red skin -Shiny skin -Swelling -Warmth -Red streaks extending from the patch indicate lymph vessels involved -Develops over a few hours -Blisters may form after 2-3 days |
| Filariasis[3] |
-Parasitic infection carried by mosquitoes. Most damaged occurs after the larva injected has died (approximately 5-10 years later). |
-Severe local inflammatory reactions leading to severe fibrosis and scarring -Massive swelling response |
| Thrombophlebitis[15] |
Blood clot causing swelling in one or more veins, typically in legs. |
-Warmth -Tenderness -Swelling -Pain -Redness |
Radiation Fibrosis Syndrome[4][edit | edit source]
When it involves localized muscle pain patients can be misdiagnosed with fibromyalgia or a rheumatic disorder.
Radiation Pneumonitis[3][edit | edit source]
Can resemble an underlying lung disease such as COPD.
Radiation-Induced Brachial Plexopathy[16][edit | edit source]
Can resemble other neurological problems and must be differentiated from brachial neuritis, carpal tunnel syndrome, cervical disc disease, cervical myofascial pain, and brachial plexopathy caused by trauma or a secondary tumor.
Case Reports/ Case Studies[edit | edit source]
Nozu T, Yoshida Y, Ohira M, Okumura T. Severe hyponatremia in association with I(131) therapy in a patient with metastatic thyroid cancer. Intern Med. 2011;50(19):2169-74. DOI: 10.2169/internalmedicine.50.5740
Abstract
Hyponatremia is a common clinical problem that results from various causes. Hypothyroidism is known to be one of the causes of this disorder. We report a case of metastatic thyroid cancer presenting with severe hyponatremia in association with hypothyroidism induced by pretreatment of I(131) therapy, such as a low-iodine diet and withdrawal of thyroid hormone. Serum arginine vasopressin (AVP) was elevated and urine osmolality was higher than that of serum. Saline infusion and thyroid hormone replacement normalized serum sodium and AVP. Inappropriate secretion of AVP in hypothyroid state was thought to be one of the causes of this hyponatremia.
Sonawane S, Gadgil N, Margam S. Therapy related myelodysplastic syndrome: a case report and review of literature. Indian J Pathol Microbiol. 2011 Apr-Jun;54(2):371-3. doi: 10.4103/0377-4929.81643.
Abstract
Therapy related myeloid neoplasm is directly related to previous cytotoxic chemotherapy or radiation therapy. We present a 47-year-old lady who developed therapy related myelodysplastic syndrome (MDS) 2.5 years after she received four cycles of chemotherapy and local radiation therapy for carcinoma breast. She presented with bicytopenia with trilineage dyspoiesis in the peripheral blood, bone marrow aspirate and biopsy. Fluorescent in-situ hybridization studies did not reveal any of the common abnormalities associated with MDS. A diagnosis of therapy related MDS was rendered. Different studies have shown that patients treated with alkylating agents and ionizing radiation present as MDS with a latent period of 3-10 years. Our patient developed MDS within 2.5 years of starting chemotherapy and radiotherapy and did not reveal any of the conventional cytogenetic abnormalities. It highlights the importance of simple tests like a complete blood count and peripheral blood smear examination in follow-up of the patients treated with chemotherapy.
Fibrosis After Proton Beam Therapy for Non-small Cell Lung Cancer. Jpn J Clin Oncol.2012 Oct;42(10):965-9. Accessed April 10, 2013.
Abstract
There have been no reports describing acute exacerbations of idiopathic pulmonary fibrosis after particle radiotherapy for non-small cell lung cancer. The present study describes the case of a 76-year-old Japanese man with squamous cell carcinoma of the lung that relapsed in the left upper lobe 1 year after right upper lobectomy. He had been treated with oral prednisolone 20 mg/day every 2 days for idiopathic pulmonary fibrosis, and the relapsed lung cancer was treated by proton beam therapy, which was expected to cause the least adverse effects on the idiopathic pulmonary fibrosis. Fifteen days after the initiation of proton beam therapy, the idiopathic pulmonary fibrosis exacerbated, centered on the left upper lobe, for which intensive steroid therapy was given. About 3 months later, the acute exacerbation of idiopathic pulmonary fibrosis had improved, and the relapsed lung cancer became undetectable. Clinicians should be aware that an acute exacerbation of idiopathic pulmonary fibrosis may occur even in proton beam therapy, although proton beam therapy appears to be an effective treatment option for patients with idiopathic pulmonary fibrosis.
Resources[edit | edit source]
Radiation Therapy and You: Support for People with Cancer
http://www.cancer.gov/cancertopics/coping/radiation-therapy-and-you/page1
American Cancer Society
Radiation Side Effects Worksheet
http://www.cancer.org/acs/groups/content/@nho/documents/document/acsq-009503.pdf
References[edit | edit source]
- ↑ Picture: http://photos2.demandstudios.com/DM-Resize/photos.demandstudios.com/60/210/fotolia_3929119_XS.jpg?h=10000&w=400&keep_ratio=1
- ↑ 2.0 2.1 2.2 Radiopedia Radiation Therapy Available from:https://radiopaedia.org/articles/radiation-therapy (last accessed 25.8.2020)
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 Goodman CC, Fuller KS. Pathology: Implications for the Physical Therapist. 3rd ed. St. Louis. Missouri: Saunders, 2009.
- ↑ 4.0 4.1 4.2 4.3 4.4 Stubblefield MD. Radiation Fibrosis Syndrome: Neuromuscular and Musculoskeletal Complications in Cancer Survivors. PM R. 2011;3:1041-1054.
- ↑ Radiopedia CRT Available from:https://radiopaedia.org/articles/conventional-radiation-therapy?lang=gb (last accessed 25.8.2020)
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 National Cancer Institute. Radiation Therapy for Cancer. National Institutes of Health. http://www.cancer.gov/cancertopics/factsheet/Therapy/radiation. Reviewed May 30, 2010. Accessed April 3, 2013.
- ↑ 7.0 7.1 7.2 National Cancer Institute. Lymphedema. National Institutes of Health. http://www.cancer.gov/cancertopics/pdq/supportivecare/lymphedema/healthprofessional/page1. Reviewed May 30, 2011. Accessed April 3, 2013.
- ↑ Zuther, J. (2010, June 3). Complications of Lympedema. Retrieved April 22, 2012, from Livestrong website: http://www.livestrong.com/article/138346-complications-lymphedema/
- ↑ Stubblefield MD. Radiation Fibrosis Syndrome: What It Is And How To Treat It [Internet]. Houston, Texas: Cancer Forward The Foundation for Cancer Survivors; 2010. Available from: http://www.cancerforward.org/survivor-resources/experts-speak/Michael-D-Stubblefield-MD/radiation-fibrosis-syndrome-what-it-is-and-how-to-treat-it.
- ↑ 10.0 10.1 Goodman C and Snyder T. Differential Diagnosis for Physical Therapy: SCREENING FOR REFERRAL. 5th edition. Missouri: Elsevier Saunders; 2013.
- ↑ Shifko R. Livestrong (Internet). Demand Media, Inc; 2010, September 24 (Cited 2013, April 22). Available from: http://www.livestrong.com/article/257967-side-effects-of-hypoalbuminemia/
- ↑ Peralta R and Rubery B. Medscape Reference (Internet). WebMD LLC; Update 2012, July 30 (Cited 2013, April 22). Available from: http://emedicine.medscape.com/article/166724-clinical#a0217
- ↑ Mayo Clinic. Mayo Foundation for Medical Education and Research (Internet); 1998 (Updated 2012, August 10; Cited 2013 April 22). Available from: http://www.mayoclinic.com/health/kidney-failure/DS00280/DSECTION=symptoms
- ↑ Cunha J. MedicineNet (Internet). 1996 (Cited 2013, April 22). Available from: http://www.medicinenet.com/edema/page6.htm
- ↑ Mayo Clinic. Mayo Foundation for Medical Education and Research (Internet); 1998 (Cited 2013 April 22). Available from: http://www.mayoclinic.com/health/thrombophlebitis/DS00223/DSECTION=symptoms
- ↑ Stephenson RO. Radiation-Induced Brachial Plexopathy Differential Diagnosis [Internet]. Medscape; Updated Mar 26, 2013. Available from: http://emedicine.medscape.com/article/316497-differential.