Patient Specific Functional Scale: Difference between revisions
mNo edit summary |
Kim Jackson (talk | contribs) No edit summary |
||
| (5 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
| Line 9: | Line 7: | ||
== Objective == | == Objective == | ||
Patient Specific Functional Scale was developed by Stratford et al 1995 as a self-report outcome measure of function that could be used in patients with varying levels of independence.<ref name=":6">Horn KK, Jennings S, Richardson G, Van Vliet D, Hefford C, Abbott JH. [https://www.ncbi.nlm.nih.gov/pubmed/22031594 The patient-specific functional scale: psychometrics, clinimetrics, and application as a clinical outcome measure. journal of orthopaedic & sports physical therapy]. 2012 Jan;42(1):30-D17.</ref> The aim of PSFS is to provide clinicians with a valid, reliable, responsive and efficient outcome measure that would be easy to use and applicable to a large number of clinical presentations.<ref>Stratford P, Gill C, Westaway M, Binkley J. [https://utpjournals.press/doi/10.3138/ptc.47.4.258 Assessing disability and change on individual patients: a report of a patient specific measure]. Physiotherapy canada. 1995 Oct;47(4):258-63.</ref | [[File:Claudio-schwarz-purzlbaum-cw2bX6cQ8Zs-unsplash.jpg|right|frameless]]Patient Specific Functional Scale was developed by Stratford et al 1995 as a self-report outcome measure of function that could be used in patients with varying levels of independence.<ref name=":6">Horn KK, Jennings S, Richardson G, Van Vliet D, Hefford C, Abbott JH. [https://www.ncbi.nlm.nih.gov/pubmed/22031594 The patient-specific functional scale: psychometrics, clinimetrics, and application as a clinical outcome measure. journal of orthopaedic & sports physical therapy]. 2012 Jan;42(1):30-D17.</ref> The aim of PSFS is to provide clinicians with a valid, reliable, responsive and efficient outcome measure that would be easy to use and applicable to a large number of clinical presentations.<ref>Stratford P, Gill C, Westaway M, Binkley J. [https://utpjournals.press/doi/10.3138/ptc.47.4.258 Assessing disability and change on individual patients: a report of a patient specific measure]. Physiotherapy canada. 1995 Oct;47(4):258-63.</ref> | ||
== Intended Population == | == Intended Population == | ||
PSFS | The PSFS is a self-reported valid, reliable, and responsive [[Outcome Measures|outcome measure]] for patients with back, neck, knee and upper extremity problems<ref name=":1">Hefford C, Abbott JH, Arnold R, Baxter GD. [http://www.jospt.org/doi/pdf/10.2519/jospt.2012.3953 The patient-specific functional scale: validity, reliability, and responsiveness in patients with upper extremity musculoskeletal problems.] journal of orthopaedic & sports physical therapy. 2012 Feb;42(2):56-65.</ref><ref name=":4">Westaway MD, Stratford PW, Binkley JM. [https://www.ncbi.nlm.nih.gov/pubmed/9580892 The patient-specific functional scale: validation of its use in persons with neck dysfunctio]n. Journal of Orthopaedic & Sports Physical Therapy. 1998 May;27(5):331-8.</ref>. It has also been shown to have a high test-retest reliability in both generic lower back pain and knee dysfunction issues.<ref name=":5">Chatman AB, Hyams SP, Neel JM, Binkley JM, Stratford PW, Schomberg A, Stabler M. [https://www.ncbi.nlm.nih.gov/pubmed/9256870 The Patient-Specific Functional Scale: measurement properties in patients with knee dysfunction]. Physical therapy. 1997 Aug 1;77(8):820-9.</ref><ref name=":6" /> It is also clinically responsive to changes over time with chronic pain patients<ref>Maughan EF, Lewis JS. [https://www.researchgate.net/publication/43161521_Outcome_measures_in_chronic_low_back_pain Outcome measures in chronic low back pain.] European Spine Journal. 2010 Sep 1;19(9):1484-94.</ref> | ||
== Method of Use == | == Method of Use == | ||
| Line 21: | Line 19: | ||
# Patients select a value that best describes their current level of ability on each activity assessed. | # Patients select a value that best describes their current level of ability on each activity assessed. | ||
[[File:PSFS score.png|center|1013x1013px|frameless]] | [[File:PSFS score.png|center|1013x1013px|frameless]] | ||
== Advantages == | == Advantages == | ||
| Line 64: | Line 26: | ||
* Relatively easy for patients to complete | * Relatively easy for patients to complete | ||
* Helpful to redirect subjective assessment to function as opposed to pain | * Helpful to redirect subjective assessment to function as opposed to pain | ||
* Can be used on a wide variety of musculoskeletal and [[Neurological Disorders|neurological]] conditions<ref name=":3" /> | * Can be used on a wide variety of musculoskeletal and [[Neurological Disorders|neurological]] conditions<ref name=":3">Maughan EF, Lewis JS. [https://www.researchgate.net/publication/43161521_Outcome_measures_in_chronic_low_back_pain Outcome measures in chronic low back pain.] European Spine Journal. 2010 Sep 1;19(9):1484-94.</ref> | ||
== Disadvantages == | == Disadvantages == | ||
| Line 71: | Line 33: | ||
* Not specific to condition | * Not specific to condition | ||
* May require further outcome measures specific to condition to be completed<ref name=":4"> | * May require further outcome measures specific to condition to be completed<ref name=":4" /> | ||
== Evidence == | |||
The PSFS is a valid, reliable, and responsive outcome measure for patients with back, neck, knee and upper extremity problems<ref name=":1" /><ref name=":4" />. It has also been shown to have a high test-retest reliability in both generic lower back pain and knee dysfunction issues.<ref name=":5" /> | |||
=== Reliability === | |||
A study into cervical radiculopathy found the test-retest reliability of the PSFS to be high (Intraclass correlation coefficient = 0.82; 95% Confidence interval= 0.54–0.93) in comparison with the [[Neck Disability Index]].<ref>Cleland JA, Fritz JM, Whitman JM, Palmer JA. [https://journals.lww.com/spinejournal/Abstract/2006/03010/The_Reliability_and_Construct_Validity_of_the_Neck.19.aspx The reliability and construct validity of the Neck Disability Index and patient specific functional scale in patients with cervical radiculopathy]. Spine. 2006 Mar 1;31(5):598-602.</ref> | |||
Moderate to good reliability for patient with upper extremity musculoskeletal problems ICC = 0,713.<ref name=":7">The Patient-Specific Functional Scale: Validity, Reliability, and Responsiveness in Patients With Upper Extremity Musculoskeletal Problems | |||
</ref> | |||
Poor reliability exhibited in patient with cervical radiculopathy.<ref name=":8">Reliability, Construct Validity, and Responsiveness of the Neck Disability Index, Patient-Specific Functional Scale, and Numeric Pain Rating Scale in Patients with Cervical Radiculopathy | |||
</ref> | |||
=== Validity === | |||
PSFS is a valid tool (p<.001) in detecting patient with upper extremity problem.<ref name=":7" /> | |||
=== Responsiveness === | |||
Adequate responsiveness in patient with cervical radiculopathy (3.3) while the clinically important difference is 2.2.<ref name=":8" /><span style="font-size: 20px; font-weight: normal;" class="Apple-style-span"></span> | |||
== Resources == | == Resources == | ||
* [http://www.tac.vic.gov.au/__data/assets/pdf_file/0020/27317/Patient-specific.pdf The Patient-Specific Functional Scale] | * [http://www.tac.vic.gov.au/__data/assets/pdf_file/0020/27317/Patient-specific.pdf The Patient-Specific Functional Scale - Questionnaire] | ||
* https://www.journalofphysiotherapy.com/article/S0004-9514(07)70066-1/pdf | * [https://www.journalofphysiotherapy.com/article/S0004-9514(07)70066-1/pdf The Patient-Specific Functional Scale - Article] | ||
== References == | == References == | ||
<references /> | |||
[[Category:Outcome Measures]] | [[Category:Outcome Measures]] | ||
[[Category:Wrist - Outcome Measures]] | [[Category:Wrist - Outcome Measures]] | ||
Latest revision as of 13:07, 13 September 2021
Original Editor -Eric Robertson Top Contributors - Kim Jackson, Abbey Wright, Hing Long Yip, Lucinda hampton, Admin, Eric Robertson, Ammar Suhail, Rachael Lowe, George Prudden and WikiSysop
Objective[edit | edit source]
Patient Specific Functional Scale was developed by Stratford et al 1995 as a self-report outcome measure of function that could be used in patients with varying levels of independence.[1] The aim of PSFS is to provide clinicians with a valid, reliable, responsive and efficient outcome measure that would be easy to use and applicable to a large number of clinical presentations.[2]
Intended Population[edit | edit source]
The PSFS is a self-reported valid, reliable, and responsive outcome measure for patients with back, neck, knee and upper extremity problems[3][4]. It has also been shown to have a high test-retest reliability in both generic lower back pain and knee dysfunction issues.[5][1] It is also clinically responsive to changes over time with chronic pain patients[6]
Method of Use[edit | edit source]
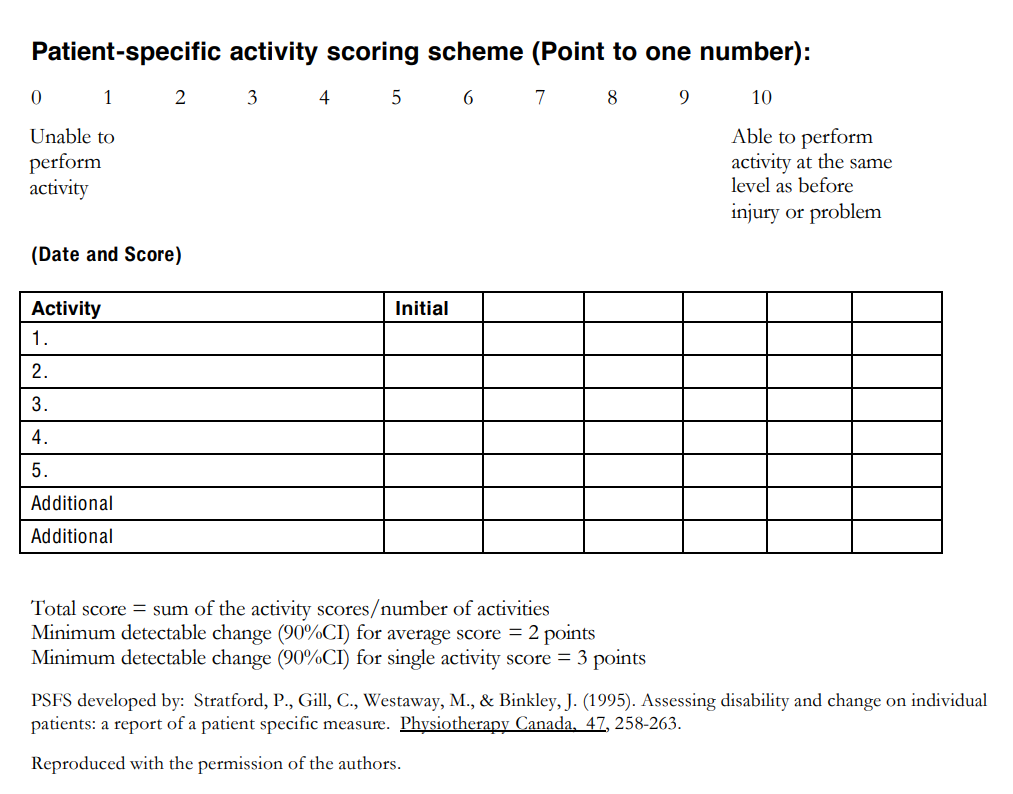
- Patients are asked to identify up to five important activities they are unable to perform or are having difficulty with as a result of their problem eg putting socks on, shopping.
- Patients are asked to rate (on an 11-point scale) the current level of difficulty associated with each activity.
- Following the intervention, patients are asked again to rate the activities previously identified (and are given the chance to nominate new problematic activities that might have arisen during that time).
- "0" represents “unable to perform” and "10" represents “able to perform at prior level”
- Patients select a value that best describes their current level of ability on each activity assessed.
Advantages[edit | edit source]
- Gives the patient positive re-enforcement that the intervention is effective[7]
- Keeps therapy goal orientated
- Quick to complete
- Relatively easy for patients to complete
- Helpful to redirect subjective assessment to function as opposed to pain
- Can be used on a wide variety of musculoskeletal and neurological conditions[8]
Disadvantages[edit | edit source]
- Not obtaining a final PSFS score. For example if a patient cancels their final appointment it is not always possible to ask for the score completion.[7]
- Some patients can find rating their activities on a numerical scale difficult
- Not specific to condition
- May require further outcome measures specific to condition to be completed[4]
Evidence[edit | edit source]
The PSFS is a valid, reliable, and responsive outcome measure for patients with back, neck, knee and upper extremity problems[3][4]. It has also been shown to have a high test-retest reliability in both generic lower back pain and knee dysfunction issues.[5]
Reliability[edit | edit source]
A study into cervical radiculopathy found the test-retest reliability of the PSFS to be high (Intraclass correlation coefficient = 0.82; 95% Confidence interval= 0.54–0.93) in comparison with the Neck Disability Index.[9]
Moderate to good reliability for patient with upper extremity musculoskeletal problems ICC = 0,713.[10]
Poor reliability exhibited in patient with cervical radiculopathy.[11]
Validity[edit | edit source]
PSFS is a valid tool (p<.001) in detecting patient with upper extremity problem.[10]
Responsiveness[edit | edit source]
Adequate responsiveness in patient with cervical radiculopathy (3.3) while the clinically important difference is 2.2.[11]
Resources[edit | edit source]
- The Patient-Specific Functional Scale - Questionnaire
- The Patient-Specific Functional Scale - Article
References[edit | edit source]
- ↑ 1.0 1.1 Horn KK, Jennings S, Richardson G, Van Vliet D, Hefford C, Abbott JH. The patient-specific functional scale: psychometrics, clinimetrics, and application as a clinical outcome measure. journal of orthopaedic & sports physical therapy. 2012 Jan;42(1):30-D17.
- ↑ Stratford P, Gill C, Westaway M, Binkley J. Assessing disability and change on individual patients: a report of a patient specific measure. Physiotherapy canada. 1995 Oct;47(4):258-63.
- ↑ 3.0 3.1 Hefford C, Abbott JH, Arnold R, Baxter GD. The patient-specific functional scale: validity, reliability, and responsiveness in patients with upper extremity musculoskeletal problems. journal of orthopaedic & sports physical therapy. 2012 Feb;42(2):56-65.
- ↑ 4.0 4.1 4.2 Westaway MD, Stratford PW, Binkley JM. The patient-specific functional scale: validation of its use in persons with neck dysfunction. Journal of Orthopaedic & Sports Physical Therapy. 1998 May;27(5):331-8.
- ↑ 5.0 5.1 Chatman AB, Hyams SP, Neel JM, Binkley JM, Stratford PW, Schomberg A, Stabler M. The Patient-Specific Functional Scale: measurement properties in patients with knee dysfunction. Physical therapy. 1997 Aug 1;77(8):820-9.
- ↑ Maughan EF, Lewis JS. Outcome measures in chronic low back pain. European Spine Journal. 2010 Sep 1;19(9):1484-94.
- ↑ 7.0 7.1 Nicholas P, Hefford C, Tumilty S. The use of the Patient-Specific Functional Scale to measure rehabilitative progress in a physiotherapy setting. Journal of Manual & Manipulative Therapy. 2012 Aug 1;20(3):147-52.
- ↑ Maughan EF, Lewis JS. Outcome measures in chronic low back pain. European Spine Journal. 2010 Sep 1;19(9):1484-94.
- ↑ Cleland JA, Fritz JM, Whitman JM, Palmer JA. The reliability and construct validity of the Neck Disability Index and patient specific functional scale in patients with cervical radiculopathy. Spine. 2006 Mar 1;31(5):598-602.
- ↑ 10.0 10.1 The Patient-Specific Functional Scale: Validity, Reliability, and Responsiveness in Patients With Upper Extremity Musculoskeletal Problems
- ↑ 11.0 11.1 Reliability, Construct Validity, and Responsiveness of the Neck Disability Index, Patient-Specific Functional Scale, and Numeric Pain Rating Scale in Patients with Cervical Radiculopathy