Paediatric Conditions of the Foot: Difference between revisions
No edit summary |
No edit summary |
||
| Line 38: | Line 38: | ||
# '''Bleck’s''' '''Heel bisector line''' is a simple measure that assesses the flexibility and severity of metatarsus adductus. It is a manual assessment and no types of equipment is needed. This method has been used for over four decades, with some modifications. Recent research has shown that this method can be unclear and has the potential for measurement errors when measuring the heel bisector line (HBL).<ref name=":2">Alonge VO. [https://www.semanticscholar.org/paper/Proposing-Transmalleolar-Axis-Bisector-%28TMAB%29-as-a-Omosemoje/94e6e9b8cb62a52ae7b2c04e9365d9f06fe3d61d?p2df Proposing Transmalleolar Axis Bisector (TMAB) as a Geometrically Accurate Alternative to the Heel Bisector Line for the Clinical Assessment of Metatarsus Adductus]. Int J Foot Ankle. 2020;4:041.</ref> Procedure: | # '''Bleck’s''' '''Heel bisector line''' is a simple measure that assesses the flexibility and severity of metatarsus adductus. It is a manual assessment and no types of equipment is needed. This method has been used for over four decades, with some modifications. Recent research has shown that this method can be unclear and has the potential for measurement errors when measuring the heel bisector line (HBL).<ref name=":2">Alonge VO. [https://www.semanticscholar.org/paper/Proposing-Transmalleolar-Axis-Bisector-%28TMAB%29-as-a-Omosemoje/94e6e9b8cb62a52ae7b2c04e9365d9f06fe3d61d?p2df Proposing Transmalleolar Axis Bisector (TMAB) as a Geometrically Accurate Alternative to the Heel Bisector Line for the Clinical Assessment of Metatarsus Adductus]. Int J Foot Ankle. 2020;4:041.</ref> Procedure: | ||
#* The shape of the weight-bearing foot is obtained. Traditionally a | #* The shape of the weight-bearing foot is obtained. Traditionally a mold of the weight-bearing foot is made, modifications include the use of footprints or photos the weight-bearing foot.<ref name=":2" /> Another option includes placing the child in prone with knees flexed to 90°, and the plantar surface of the foot parallel to the ceiling.<ref name=":1" /> | ||
#* Next, the procedure is completed by determining the longitudinal axis of the ellipse with a straight edge, independent of the forefoot.<ref name=":2" /> | #* Next, the procedure is completed by determining the longitudinal axis of the ellipse with a straight edge, independent of the forefoot.<ref name=":2" /> | ||
#* Classification of metatarsus adductus according to Bleck’s classification involves observation of where the HBL crosses the metatarsal heads.<ref name=":2" />'''''Add image from video?''''' [[File:Bleck's classification of metatarsus adductus.png|center|thumb|500x500px|Bleck's classification of metatarsus adductus<ref name=":1" />]] | #* Classification of metatarsus adductus according to Bleck’s classification involves observation of where the HBL crosses the metatarsal heads.<ref name=":2" />'''''Add image from video?''''' [[File:Bleck's classification of metatarsus adductus.png|center|thumb|500x500px|Bleck's classification of metatarsus adductus<ref name=":1" />]] | ||
| Line 111: | Line 111: | ||
* '''to a physical medicine specialist''': | * '''to a physical medicine specialist''': | ||
** if under five years of age, pain in their knees, hips and feet | ** if under five years of age, pain in their knees, hips and feet | ||
== [[Introduction to Clubfoot|Clubfoot]] (Talipes Equinovarus) == | == [[Introduction to Clubfoot|Clubfoot]] (Talipes Equinovarus) == | ||
<blockquote>Clubfoot "is one of the most common congenital malformations and is characterized across varying degrees and severity of predictable contractures manifesting with four main components: (1) midfoot cavus, (2) forefoot adductus, (3) heel/hindfoot varus and (4) hindfoot equinus."<ref name=":5">Barrie A, Varacallo M. [https://www.ncbi.nlm.nih.gov/books/NBK551574/ Clubfoot]. InStatPearls [Internet] 2022 Sep 4. StatPearls Publishing.</ref></blockquote> | <blockquote>Clubfoot "is one of the most common congenital malformations and is characterized across varying degrees and severity of predictable contractures manifesting with four main components: (1) midfoot cavus, (2) forefoot adductus, (3) heel/hindfoot varus and (4) hindfoot equinus."<ref name=":5">Barrie A, Varacallo M. [https://www.ncbi.nlm.nih.gov/books/NBK551574/ Clubfoot]. InStatPearls [Internet] 2022 Sep 4. StatPearls Publishing.</ref></blockquote> | ||
* occurs twice as often in | * occurs twice as often in males as in females<ref name=":5" /> | ||
* can be unilateral or bilateral<ref name=":1" /> | * can be unilateral or bilateral<ref name=":1" /> | ||
** approximately 50% of case involve bilateral clubfoot<ref name=":5" /> | ** approximately 50% of case involve bilateral clubfoot<ref name=":5" /> | ||
| Line 141: | Line 139: | ||
These deformities can present with a range of orthopaedic deformity and degree of stiffness.<ref name=":5" /> Several scoring systems exist<ref name=":1" /> and can be used to help in the assessment and classifying the degree of deformity present. According to the literature, there is no gold standard grading method for assessing or monitoring the degree of deformity associated with clubfoot.<ref name=":6" /> | These deformities can present with a range of orthopaedic deformity and degree of stiffness.<ref name=":5" /> Several scoring systems exist<ref name=":1" /> and can be used to help in the assessment and classifying the degree of deformity present. According to the literature, there is no gold standard grading method for assessing or monitoring the degree of deformity associated with clubfoot.<ref name=":6" /> | ||
==== Pirani Scoring System ==== | |||
[[Pirani Score|Pirani Scoring System]] is based on six well-described clinical signs of contracture characterising a severe clubfoot.<ref name=":7">Africa Clubfoot Training Project. Chapter 4 Africa Clubfoot Training Basic & Advanced Clubfoot Treatment Provider Courses - Participant Manual. University of Oxford: Africa Clubfoot Training Project, 2017.</ref> This scoring system quantifies the degree of clubfoot deformity.<ref name=":8">Jochymek J, Peterková T. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6362704/#:~:text=Dimeglio´s%20classification%20has,4%20points%2C%20and%20another%20four Are scoring systems useful for predicting results of treatment for clubfoot using the ponseti method]?. Acta Ortopédica Brasileira. 2019 Jan;27:8-11.</ref> | |||
* If the sign is severely abnormal, it scores 1 | |||
* If it is partially abnormal, it scores 0.5 | |||
* If it is normal, it scores 0 | |||
The midfoot and hindfoot are evaluated separately. The mid foot contracture score (MFCS) includes: medial crease, lateral edge convexity, and the lateral talus head position. The hindfoot contracture score (HCFS) includes: the posterior crease, empty heel, and rigid equinus.<ref name=":8" /> The six areas assessed include three signs from the midfoot and three signs from the hindfoot. The six areas as scored as described above, then the scores are summed to a Total Score, which ranges from 0-6. The higher the score, the more severe the presentation.<ref name=":7" />[[File:Pirani score.png|center|frameless|500x500px]]The assessment is performed with the examiner in sitting. The infant is on the mother’s lap. A feeding, relaxed infant allows a more precise examination. The measurements are made while the examiner is gently correcting the foot with minimal effort, and no discomfort.<ref name=":7" /> For more information on using this scoring system please read [[Pirani Score#Technique|this article]]. For a clinical example, please see [[Pirani Score Example|this article]] | |||
==== Dimeglio Classification Scoring System ==== | |||
Dimeglio Classification Scoring System is based on 8-rated areas characterising clubfoot. It focuses on assessing the degree of rigidity of the foot.<ref name=":8" /><ref name=":9">Andriesse H, Roos EM, Hägglund G, Jarnlo GB. [https://www.researchgate.net/publication/7238380_Validity_and_responsiveness_of_the_Clubfoot_Assessment_Protocol_CAP_A_methodological_study Validity and responsiveness of the Clubfoot Assessment Protocol (CAP)]. A methodological study. BMC Musculoskeletal Disorders. 2006 Dec;7(1):1-9.</ref> This scoring system distinguishes four basic parameters: (1) equinosity in the sagittal plane, (2) varus deviation in the frontal plane, (3) deformation of the block calcaneus and forefoot, and (4) adduction of the forefoot in the horizontal plane), evaluated on a scale from 0 to 4 points.<ref name=":8" /> I. st. soft-soft; II. st. soft-stiff; III. st. stiff-soft; and IV. st. stiff-stiff deformity. Next, an additional four adverse symptoms: (1) posterior crease, (2) medial crease, (3) cavus deformity, and (4) calf hypotrophy (deviant muscle function) are rated 1-point each.<ref name=":8" />[[File:Dimeglio classification scoring system.png|center|thumb|500x500px|Abbreviations for above: pltf = plantarflexion; dorsx = dorsalflexion; var = varus; vlg = valgus; sup = supination; pron = pronation; add = adduction; abd = abduction.]]Total score ranges between 0-20. The higher the score, the more severe the presentation.<ref name=":9" /> | |||
* most severe: 16–20 | |||
* severe 11–15 | |||
* moderate 6–10 | |||
* postural 0–5 | |||
=== Interventions === | |||
<blockquote>"The purposes of clubfoot therapy are to achieve and maintain clubfoot correction, so that the patients have functional, painless, plantigrade feet with good mobility" -Ponseti & Campos, 2009 <ref name=":6" /></blockquote>The [[Ponseti method|Ponseti Method]] is the gold standard treatment for clubfoot deformity. This treatment method was developed in response to the complications and poor outcomes which came with surgical management of clubfoot.<ref>Gerlach, D.J., Gurnett, CA.,Limpaphayom, N.,Alaee, Farhang.,Zhang, Z.,Porter, K.,Smyth, M. D Dobbs, Matthew B 2009. Early results of the Ponseti method for the treatment of clubfoot associated with myelomeningocele. The Journal of bone and joint surgery. American volume, 91, pp.1350–1359</ref> | |||
* Occurs over two phases: treatment phase and maintenance phase | |||
** '''Treatment (Corrective) Phase''' is when the deformity is physically corrected by gentle mobilisations and serial casting<ref name=":1" /> | |||
*** begins as early in the infant's life as possible, typically within the first week | |||
*** mobilisations and casting occur on a weekly basis | |||
*** typically requires 6<ref name=":1" /> to 8<ref name=":7" /> rounds of casting to correct deformity | |||
*** majority of infants will still require minor surgery | |||
** '''Maintenance Phase''' involves strict and scheduled bracing protocol to prevent deformity reoccurrence as the infant continues to grow<ref name=":1" /> | |||
*** orthotic brace must be worn for 23-hours per day for three months | |||
*** wearing schedule decreases to nightly for multiple years | |||
*** adherence and carryover can be challenging for families to complete | |||
*** inability to carryover properly and correctly in this phase in its entirety can result in recurrence of the clubfoot deformity | |||
** [[Achilles Tenotomy|Percutaneous Achilles Tenotomy]] surgery is indicated in 90% of cases<ref name=":7" /> | |||
*** corrects remaining rigid equinus | |||
*** involves a complete cut through of the Achilles tendon, ''not'' a tendon lengthening | |||
*** the tendon heals sufficiently in approximately 3-weeks. | |||
'''''The above listed procedures require advanced in-person training to safely perform. It is not recommended for a rehabilitation professional to perform serial casting without proper training due to risk of pressure injury and wound formation. For a general overview of casting for clubfoot, please read this [[Casting for Clubfoot|article]].''''' | |||
==== Role of the Rehabilitation Professional in Clubfoot Interventions ==== | |||
Monitoring for deformity reoccurrence | |||
== Resources == | == Resources == | ||
video of HBL? | video of HBL? | ||
Revision as of 05:40, 28 November 2023
This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! (28/11/2023)
Top Contributors - Stacy Schiurring, Jess Bell and Kim Jackson
Introduction[edit | edit source]
Optional reading: for an in-depth review of foot structure and functional anatomy, please read this article.
Metatarsus Adductus (Metatarsus Varus)[edit | edit source]
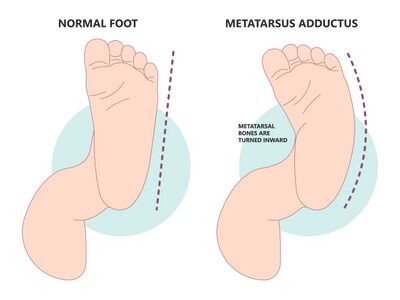
"Metatarsus adductus primarily involves medial deviation of the forefoot on the hindfoot." - Pediatric Orthopedic Society of North America (POSAN)[1]
Secondary characteristics include:
- prominence of the 5th metatarsal base [1]
- neutral[2] to slightly valgus hindfoot [1]
- slightly supinated forefoot [1]
- a possible widening of the space between the 1st and 2nd toes [1]
- many patients also have internal tibial torsion [1]
- no ankle range of motion (ROM) restrictions [2]
Metatarsus Adductus can be divided into two types:
- Flexible: Presents with adduction of the 5 metatarsal bones at the tarsometatarsal joint.
- Rigid: Presents with medial subluxation of the tarsometatarsal joints. There is valgus of the hindfoot and the navicular is later to the head of the talus.
Incidence: 1/1,000 live births [1][2]
Aetiology:
- In utero compression
- Embryologic or congenital abnormalities [2]
Assessment[edit | edit source]
- Bleck’s Heel bisector line is a simple measure that assesses the flexibility and severity of metatarsus adductus. It is a manual assessment and no types of equipment is needed. This method has been used for over four decades, with some modifications. Recent research has shown that this method can be unclear and has the potential for measurement errors when measuring the heel bisector line (HBL).[3] Procedure:
- The shape of the weight-bearing foot is obtained. Traditionally a mold of the weight-bearing foot is made, modifications include the use of footprints or photos the weight-bearing foot.[3] Another option includes placing the child in prone with knees flexed to 90°, and the plantar surface of the foot parallel to the ceiling.[2]
- Next, the procedure is completed by determining the longitudinal axis of the ellipse with a straight edge, independent of the forefoot.[3]
- Classification of metatarsus adductus according to Bleck’s classification involves observation of where the HBL crosses the metatarsal heads.[3]Add image from video?
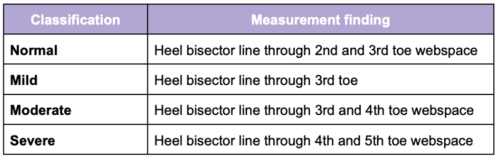 Bleck's classification of metatarsus adductus[2]
Bleck's classification of metatarsus adductus[2]
- Transmalleolar Axis Bisector (TMAB) is an newly proposed alternative assessment technique for measuring the severity of metatarsus adductus. [3] Procedure:[3]
- The child in prone with knees flexed to 90° and the plantar surface of the foot parallel to the ceiling. Weight-bearing of the foot is approximated by maintaining the ankle in a plantigrade position.
- Using a pair of vernier calipers, a line is drawn across the heel connecting the most medial point of the medial malleolus to the most lateral point of the lateral malleolus. The midpoint of this line is marked.
- A goniometer is then placed on the foot, with the axis on the marked midpoint, the stationary arm aligned on the drawn line. The moveable arm is placed at 90° to the stationary arm. The moveable arm delineates the TMAB.
- Classification of metatarsus adductus is based off the location of where the TMAB cross the metatarsal heads. There are currently no classification norms using this method as research is ongoing. Researchers recommend recording outcomes as TMAB at the second interdigital web space, third digit, third interdigital web space, etc. Create an image?
Intervention[edit | edit source]
- Mild cases: typically resolves without intervention[2]
- Moderate cases: [2]
- Stretching exercises
- Corrective shoe ware
- straight last
- reverse last
- Severe cases:[2]
- Manipulation
- Serial casting followed by corrective shoe ware
- Surgery should not considered before ages of four to allow for spontaneous resolution
Pes Planus (pes planovalgus or flat foot)[edit | edit source]
Pes Planus is "defined by the loss of the medial longitudinal arch of the foot where it contacts or nearly contacts the ground."[4]It can occur with or without further deformities of the foot and ankle.[5]
Pes planus can be divided into two types:
- Flexible: where the longitudinal arches of the foot are present on heel elevation (tiptoe standing) and non-bearing but disappear with full weight bearing on the foot.[6]
- Rigid: where the longitudinal arches of the foot are absent in both heel elevation (tiptoe standing) and weight bearing. This is normally associated with underlying pathology[8] such as vertical talus or tarsal coalition.[5]
Incidence: 7 to 22% of the general population[2]
Aetiology:
- Congenital: most infants have flat feet due to ligamentous laxity and developing neuromuscular control. Only a small percentage of children fail to develop normal arches. Children with Down Syndrome, Marfan Syndrome, or Ehlers-Danos Syndrome can be prone to congenital ligamentous laxity.[4]
- Aquired: most commonly associated with posterior tibial tendon dysfunction
Factors that can contribute to an increased flat foot:
- Little time spent barefoot resulting in weak foot intrinsic muscles and poor foot arch development[2]
- Childhood obesity[2][4]
Assessment[edit | edit source]
- Significant malalignment with or without associated pain:
- Presence of an accessory navicular bone
- Lack of mobility:
- Need to rule out tarsal coalition with rigid or limited subtalar motion
- A full-body postural assessment can also be useful to rule out issue further up the kinetic chain
- Neuro screen[2]
Intervention[edit | edit source]
"... we don't need to correct if they don't have pain, if there's no problem with their gait, or their ability to participate in activities of interest. " -Krista Eskay, PT[2]
Rehabilitation Interventions:
- Pain management
- Stretching/increasing ankle flexibility
- Strengthening foot intrinsics and ankle muscles
- Proprioceptive training
- Family education and reassurance
Providing additional support:
- Shoes with an arch support. This will not correct the deformity but will provide additional stability and can result in improved mobility and gait.
- Orthotics
When to refer:
- to an orthopedist:
- if the longitudinal arch of the foot are absent on heel elevation, or is asymmetrical
- significant pain affecting activities of daily living or mobility
- to a neurologist:
- abnormal neuro screen
- if under five years of age, pain in their knees, hips and feet
- to a physical medicine specialist:
- if under five years of age, pain in their knees, hips and feet
Clubfoot (Talipes Equinovarus)[edit | edit source]
Clubfoot "is one of the most common congenital malformations and is characterized across varying degrees and severity of predictable contractures manifesting with four main components: (1) midfoot cavus, (2) forefoot adductus, (3) heel/hindfoot varus and (4) hindfoot equinus."[9]
- occurs twice as often in males as in females[9]
- can be unilateral or bilateral[2]
- involved foot can be smaller and shorter in size[2]
- clubfoot will have an empty heel pad[2]
- transverse plantar crease present[2]
Incidence: 1/1,000 live births[2][10]
Aetiology:
- Idiopathic: approximately 80% of cases
- Other cases tend to be associated with disorders such as Spina Bifida, Cerebral Palsy and Arthrogryposis[11]
Assessment[edit | edit source]
When assessing the foot, there are several distinctive deformities associated with clubfoot:[9][12]
- midfoot cavus
- forefoot adductus
- hindfoot varus
- hindfoot equinus.
These deformities can present with a range of orthopaedic deformity and degree of stiffness.[9] Several scoring systems exist[2] and can be used to help in the assessment and classifying the degree of deformity present. According to the literature, there is no gold standard grading method for assessing or monitoring the degree of deformity associated with clubfoot.[12]
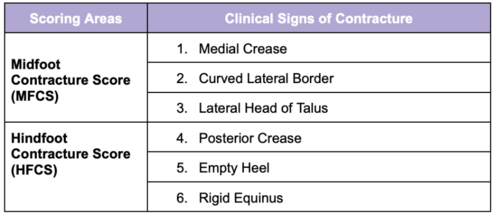
Pirani Scoring System[edit | edit source]
Pirani Scoring System is based on six well-described clinical signs of contracture characterising a severe clubfoot.[13] This scoring system quantifies the degree of clubfoot deformity.[14]
- If the sign is severely abnormal, it scores 1
- If it is partially abnormal, it scores 0.5
- If it is normal, it scores 0
The midfoot and hindfoot are evaluated separately. The mid foot contracture score (MFCS) includes: medial crease, lateral edge convexity, and the lateral talus head position. The hindfoot contracture score (HCFS) includes: the posterior crease, empty heel, and rigid equinus.[14] The six areas assessed include three signs from the midfoot and three signs from the hindfoot. The six areas as scored as described above, then the scores are summed to a Total Score, which ranges from 0-6. The higher the score, the more severe the presentation.[13]
The assessment is performed with the examiner in sitting. The infant is on the mother’s lap. A feeding, relaxed infant allows a more precise examination. The measurements are made while the examiner is gently correcting the foot with minimal effort, and no discomfort.[13] For more information on using this scoring system please read this article. For a clinical example, please see this article
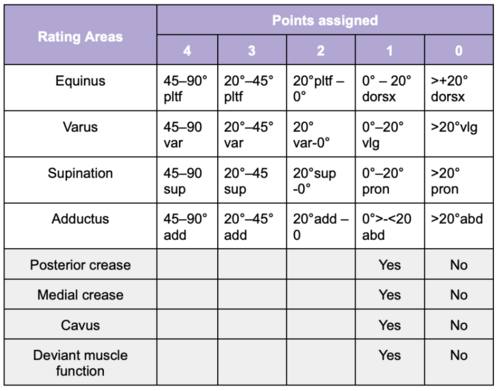
Dimeglio Classification Scoring System[edit | edit source]
Dimeglio Classification Scoring System is based on 8-rated areas characterising clubfoot. It focuses on assessing the degree of rigidity of the foot.[14][15] This scoring system distinguishes four basic parameters: (1) equinosity in the sagittal plane, (2) varus deviation in the frontal plane, (3) deformation of the block calcaneus and forefoot, and (4) adduction of the forefoot in the horizontal plane), evaluated on a scale from 0 to 4 points.[14] I. st. soft-soft; II. st. soft-stiff; III. st. stiff-soft; and IV. st. stiff-stiff deformity. Next, an additional four adverse symptoms: (1) posterior crease, (2) medial crease, (3) cavus deformity, and (4) calf hypotrophy (deviant muscle function) are rated 1-point each.[14]
Total score ranges between 0-20. The higher the score, the more severe the presentation.[15]
- most severe: 16–20
- severe 11–15
- moderate 6–10
- postural 0–5
Interventions[edit | edit source]
"The purposes of clubfoot therapy are to achieve and maintain clubfoot correction, so that the patients have functional, painless, plantigrade feet with good mobility" -Ponseti & Campos, 2009 [12]
The Ponseti Method is the gold standard treatment for clubfoot deformity. This treatment method was developed in response to the complications and poor outcomes which came with surgical management of clubfoot.[16]
- Occurs over two phases: treatment phase and maintenance phase
- Treatment (Corrective) Phase is when the deformity is physically corrected by gentle mobilisations and serial casting[2]
- Maintenance Phase involves strict and scheduled bracing protocol to prevent deformity reoccurrence as the infant continues to grow[2]
- orthotic brace must be worn for 23-hours per day for three months
- wearing schedule decreases to nightly for multiple years
- adherence and carryover can be challenging for families to complete
- inability to carryover properly and correctly in this phase in its entirety can result in recurrence of the clubfoot deformity
- Percutaneous Achilles Tenotomy surgery is indicated in 90% of cases[13]
- corrects remaining rigid equinus
- involves a complete cut through of the Achilles tendon, not a tendon lengthening
- the tendon heals sufficiently in approximately 3-weeks.
The above listed procedures require advanced in-person training to safely perform. It is not recommended for a rehabilitation professional to perform serial casting without proper training due to risk of pressure injury and wound formation. For a general overview of casting for clubfoot, please read this article.
Role of the Rehabilitation Professional in Clubfoot Interventions[edit | edit source]
Monitoring for deformity reoccurrence
Resources[edit | edit source]
video of HBL?
- bulleted list
- x
or
- numbered list
- x
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Pediatric Orthopaedic Society of North America (POSNA). Metatarsus Adductus. Available from: https://posna.org/physician-education/study-guide/metatarsus-adductus (accessed 29 October 2023).
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 2.19 2.20 2.21 2.22 Eskay, K. Paediatric Physiotherapy Programme. Paediatric Conditions of the Foot. Physioplus. 2023.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Alonge VO. Proposing Transmalleolar Axis Bisector (TMAB) as a Geometrically Accurate Alternative to the Heel Bisector Line for the Clinical Assessment of Metatarsus Adductus. Int J Foot Ankle. 2020;4:041.
- ↑ 4.0 4.1 4.2 4.3 National Institute of Health, National Library of Medicine. StatPearls | Pes Planus. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430802/#:~:text=Pes%20planus%20commonly%20referred%20to,fascia%20between%20the%20forefoot%20and (accessed 14 November 2023).
- ↑ 5.0 5.1 KAYMAZ B. Pediatric Pes Planus (flatfoot). Family Practice and Palliative Care. 2022 Oct 19;7(4):118-23.
- ↑ Kothari A, Bhuva S, Stebbins J, Zavatsky AB, Theologis T. An investigation into the aetiology of flexible flat feet: the role of subtalar joint morphology. A The Bone & Joint Journal. 2016 Apr;98(4):564-8
- ↑ Squibb M, Sheerin K, Francis P. Measurement of the Developing Foot in Shod and Barefoot Paediatric Populations: A Narrative Review. Children. 2022 May 19;9(5):750.
- ↑ Halabchi F, Mazaheri R, Mirshahi M, Abbasian L. Pediatric flexible flatfoot; clinical aspects and algorithmic approach. Iranian journal of pediatrics. 2013 Jun;23(3):247.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 Barrie A, Varacallo M. Clubfoot. InStatPearls [Internet] 2022 Sep 4. StatPearls Publishing.
- ↑ Dibello D, Di Carlo V, Colin G, Barbi E, Galimberti A. What a paediatrician should know about congenital clubfoot. Italian Journal of Pediatrics. 2020 Dec;46(1):1-6.
- ↑ Bridgens J, Kiely N. Current management of clubfoot (congenital talipes equinovarus). BmJ. 2010 Feb 2;340(6):c355.
- ↑ 12.0 12.1 12.2 Martanto TW, Dominica H, Irianto KA, Bayusentono S, Utomo DN. The pirani score evaluation on patients with clubfoot treated with the ponsety method in public hospital. EurAsian Journal of BioSciences. 2020;14(2):3419-22.
- ↑ 13.0 13.1 13.2 13.3 13.4 Africa Clubfoot Training Project. Chapter 4 Africa Clubfoot Training Basic & Advanced Clubfoot Treatment Provider Courses - Participant Manual. University of Oxford: Africa Clubfoot Training Project, 2017.
- ↑ 14.0 14.1 14.2 14.3 14.4 Jochymek J, Peterková T. Are scoring systems useful for predicting results of treatment for clubfoot using the ponseti method?. Acta Ortopédica Brasileira. 2019 Jan;27:8-11.
- ↑ 15.0 15.1 Andriesse H, Roos EM, Hägglund G, Jarnlo GB. Validity and responsiveness of the Clubfoot Assessment Protocol (CAP). A methodological study. BMC Musculoskeletal Disorders. 2006 Dec;7(1):1-9.
- ↑ Gerlach, D.J., Gurnett, CA.,Limpaphayom, N.,Alaee, Farhang.,Zhang, Z.,Porter, K.,Smyth, M. D Dobbs, Matthew B 2009. Early results of the Ponseti method for the treatment of clubfoot associated with myelomeningocele. The Journal of bone and joint surgery. American volume, 91, pp.1350–1359