Lumbar Spinal Stenosis
Original Editors
Top Contributors - Donald John Auson, Astrid Lahousse, Stefanie Van De Vijver, Roxane Roosens, Kim Jackson, Pauline Bouten, George Prudden, Laure Lievens, Rosie Swift, Manisha Shrestha, Shreya Pavaskar, Ahmed M Diab, Mariam Hashem, Lucinda hampton and Sai Kripa
Definition/Description[edit | edit source]
Lumbar spinal stenosis (LSS) is a degenerative condition in which there is diminished space available for the neural and vascular elements in the lumbar spine secondary to degenerative changes in the spinal canal. [41] This compression can also cause radiating pain and numbness to the buttock, thigh, or leg particularly during walking or standing for a long time. The pain reduces usually when a patient is in resting, sits down or bends forward. Spinal stenosis is related to aging, affecting mostly individuals over the age of 60 years. [12] Not all patients with spinal narrowing develop symptoms, so the term "spinal stenosis" refers to the symptoms of pain and not to the narrowing itself. [5]
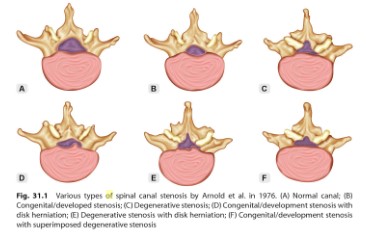
There are various types of spinal canal stenosis (Fig 1).
Fig. 1: Various types of spinal canal stenosis [51]
Clinically Relevant Anatomy[edit | edit source]
Lumbar spinal stenosis refers to an anatomic and pathologic condition that includes the narrowing of the lower spinal canal (central stenosis) or one or more lumbar vertebral foramina (foraminal/lateral stenosis).
There are 33 spinal cord nerve segments in a human spinal cord, and 5 lumbar segments that form 5 pairs of lumbar nerves. [8]
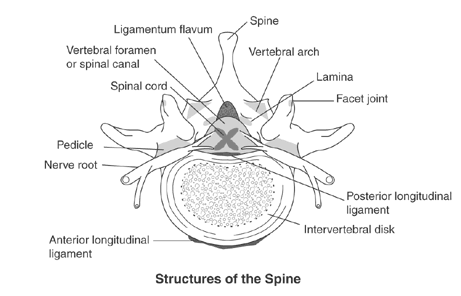
Following structures of the spine are most involved in lumbar spinal stenosis:
- Disci intervertebrales (intervertebral discs): There is one disc between each pair of vertebrae, except for the first cervical segment, the atlas. The center is called the nucleus pulposus. This nucleus is surrounded by the annulus fibrosus, which contains several layers of fibrocartilage. the intervertebral disc acts as shock absorbers.
- Facet joints: Synovial joints located on the back of the main part of the vertebra. They are formed by the superior articular process of the underlying vertebra and the inferior articular process of the vertebra lying above it. They connect the vertebrae to each other and permit backward motion. Facet joints
- Foramen intervertebrale (intervertebral foramen): An opening between vertebrae through which nerves leave the spine and extend to other parts of the body.
- Ligaments: Fibrous bands of connective tissue that connect two or more bones together and help stabilize joints They support the spine by preventing the vertebrae from slipping out of line as the spine moves. A large ligament often involved in spinal stenosis is the ligamentum flavum, which runs as a continuous band from lamina to lamina in the spine.
- Medulla spinalis (Spinal cord/nerve roots): Throughout the entire spine there is a central spinal canal which contains the spinal cord. It is a long, thin, tubular bundle of nervous tissue which is surrounded by the vertebrae. The spinal cord is part of the central nervous system providing a means of communication between the brain and the rest of the body.
- Cauda equina: A sack of nerve roots that continues from the lumbar region, where the spinal cord ends, and continues down to provide neurologic function to the lower part of the body. [4]
Fig. 2: Anatomy of the spine [6]
Epidemiology /Etiology[edit | edit source]
The prevalence of relative and absolute LSS increased respectively from 16.0% to 38.8% and from 4.0% to 14.3% between age <40 years and 60+ years. If we take a closer look at the 60-69 year-old group, the prevalence of acquired stenosis increases with age to relative 47.2% and absolute 19.4%. [32], [49]
It is an extensive problem in the elderly, presenting with pain, disability, fall risk and depression. [44] (level of evidence 2A)
Some people are born with a small spinal canal. This is called "congenital stenosis”. However, spinal canal narrowing is most often due to age-related changes that take place over time. This condition is called "acquired spinal stenosis." Spinal stenosis is most common in people over 50 years of age. [14]
Acquired forms of LSS are further classified as degenerative, spondylolisthetic, iatrogenic (postsurgical), posttraumatic, or combined. [14]
Lumbar spinal stenosis can be caused by:
- osteoarthritis
- inflammatory spondyloarthritis
- bulging of the disc
- thickening of the vertebral ligament
- tumor
- infection
- various metabolic bone disorders that cause bone growth, such as Paget's disease [1,12,14]
Characteristics/Clinical Presentation[edit | edit source]
The symptom most commonly attributed to LSS is neurogenic claudication, also referred to as pseudo-claudication. [42]
Symptoms of spinal stenosis often start slowly and get worse over time. Pain in the legs may become so severe that walking, even short distances, is unbearable. Frequently, patients must sit or lean forward to temporarily ease pain. [1,12,15]
Neurogenic claudication refers to leg symptoms encompassing the buttock, groin and anterior thigh, as well as radiation down the posterior part of the leg to the feet. In addition to pain, leg symptoms can include fatigue, heaviness, weakness and/or paraesthesia. Patients with LSS also can report nocturnal leg cramps and neurogenic bladder symptoms. Symptoms can be unilateral or more commonly bilateral and symmetrical. A key feature of neurogenic claudication is its relationship to the patient’s posture where lumbar extension increases and flexion decreases pain. Symptoms progressively worsen when standing or walking and are relieved by sitting.
Relief with sitting in LSS contrasts with most nonspecific low back pain, which is commonly exacerbated by prolonged sitting. Patients with neurogenic claudication report that laying flat is often associated with less relief while lying on the side (permitting lumbar flexion) is more comfortable. [42]
Some patients may report symptoms that are difficult to definitively attribute to LSS. For example, they may only report low back pain (without leg symptoms), which are typical of neurogenic claudication (e.g., characteristic positional nature of symptoms). [42]
Differential Diagnosis[edit | edit source]
Pathologies/diseases that mimic lumbar spinal stenosis are:
- disc herniation
- spinal cord primary or secondary tumor
- peripheral neuropathy
- osteoarthritis of hips or knees
- osteoporotic/lumbar compression fracture
- myofascial pain
- rheumatoid arthritis
- lumbar degenerative disk disease
- lumbar facet arthropathy
- lumbar spondylolysis, spondylolisthesis and spondylodiscitis
- mechanical low back pain
- cauda equina syndrome = red flag
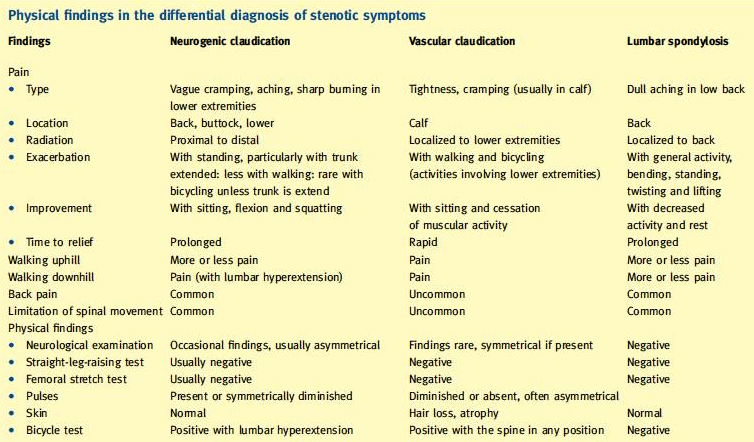
A difference must be made between neurogenic claudication caused by LSS, lumbar spondylosis, or vascular claudication. You can find all the differences between Lumbar spondylosis, neurogenic and vascular claudication in table 1.
Table 1: Physical finding in the differential diagnosis of stenotic symptoms [42]
Older patients (>60-65 years) with back or leg pain, diagnostic possibilities differ from younger patients: non-mechanical causes of back pain, such as malignancy, infection or abdominal aortic aneurysm are common in elderly patients. [8]
Diagnostic Procedures[edit | edit source]
First the clinical diagnosis of LSS, and exclusion of other competing diagnoses: the history and medical history of the patient should be questioned. Ask for a description of symptoms and for any injury, condition, or general health problem that might be causing the symptoms.
The therapist checks for pain or symptoms when the patient hyper-extends the spine (bends backwards), and checks for normal neurologic function (for instance, sensation, muscle strength, and reflexes) in the arms and legs.
Furthermore, a variety of measurements can be used to assess treatment of patients with LSS. The underlying cause of LSS is identified by imaging techniques such as [32] (level of evidence 1A):
- Radiography is usually the first step to identify a degenerative process (disc degeneration, osteophytes, facet hypertrophy).
- MRI (Magnetic Resonance Imaging) (T2 weighted) is used for determining the degree of stenosis and the thickness of Ligamentum Flavum.
o Diameter of 10 mm of the spinal canal equals absolute stenosis;
o Diameter of 12 mm indicates severe stenosis.
- By means of a CT scan a cross-section of the spinal canal may reveal the effects of disk pathology, facet hypertrophy and buckled Ligamentum Flavum. Nonetheless a CT scan has poor soft-tissue contrast, which is why a myelography is usually conducted simultaneously.
- Triple sequence [44] (level of evidence 2A)
- Ultrasound (US) [44] (level of evidence 2A)
- Myelography [44] (level of evidence 2A)
To date, we are unaware of an identified association between patient report of symptoms, functional outcomes (Oswestry), Visual Analog Scale (VAS), and anatomical impairment in patients with LSS . [44] (level of evidence 2A)
The severity of the structural pathology has a poor correlate with the severity of symptoms and limitation. [14]
In fact, examination of asymptomatic subjects showed that >30% had canal narrowing that would be classified as consistent with LSS. Imaging therefore cannot be considered a gold-standard in diagnosis of LSS, and must only be considered as an adjunct to a thorough physical examination. [44] (level of evidence 2A)
Outcome Measures[edit | edit source]
- The Modified Oswestry Disability Index (MOSW). [13, 17, 50]
- The Satisfaction Subscale of the Spinal Stenosis Scale (SSS); this is a test for psychological well-being.
- A numerical Pain Rating Scale (NRPS) for average thigh/leg pain [10]
- The Swiss Spinal Stenosis Questionnaire [13]
- The Oxford Spinal Stenosis Score [13]
- Visual analogue scale [50,17]
- Roland-Morris Disability Questionnaire [50]
- A self-administered, self-reported history questionnaire (SSHQ) [43]
Examination[edit | edit source]
The physical examination for patients with LSS is usually normal or demonstrates nonspecific findings. Patients with stenosis often have lumbar, paraspinal, or gluteal tenderness, which is usually related to underlying degenerative changes, muscle spasms, and poor posture.
The neurologic examination is usually normal or reveals only subtle abnormalities such as mild weakness, sensory changes, and reflex abnormalities. The achilles tendon reflexes (Fig. 3) are often diminished, while abnormal knee reflexes are less common. The straight leg-raise test and other neural tension signs are usually negative unless there is accompanying disc herniation. Hamstring tightness is often present and may produce a false-positive straight leg-raise test. [9] (level of evidence 3B) ,[12] (level of evidence 3B)
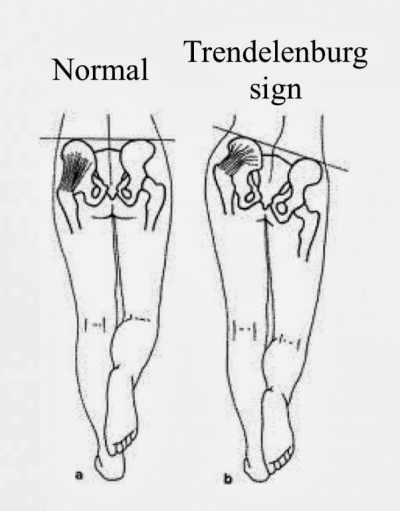
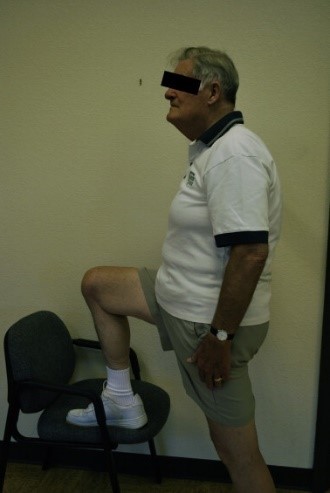
A careful motor examination should be performed. Leg weakness is generally mild and in the distribution of the L4, L5, or S1 nerve roots. Weakness of the muscles innervated by L5 is the most common finding. If the physiotherapist wants to demonstrate the spinal level truly responsible for the symptoms of LSS, it is recommended to use the gait-loading test which is a provocation test (level of evidence 3B). The lumbar extension-loading test (Fig. 4) is useful for assessment of lumbar spinal stenosis pathology and is capable of accurately determining the involved spinal level. In this test, you have to maintain the lumbar region in moderate (angle of 10°-30°)extension while standing as long as you can. After the patient has performed this test, changes in subjective symptoms and objective neurological findings can be evaluated [33](level of evidence 3B). The examiner should test for weakness of great toe extensors and hip abductors as well. The Trendelenburg test (Fig. 5) is used to observe for hip abductor weakness. Difficulty with walking on the toes suggests S1 root involvement. Difficulty with heel walking suggests L4 or L5 nerve dysfunction. [12] (level of evidence 3B)
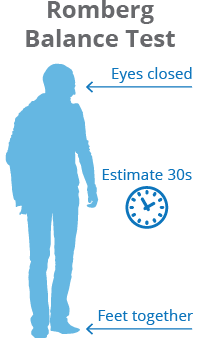
Katz et al report physical examination findings most strongly associated with lumbar spinal stenosis (LSS) include wide-based gait, abnormal Romberg test, (Fig. 6) thigh pain following 30 seconds of lumbar extension, and neuromuscular abnormalities [46]; however, Fritz et al state physical examination findings do not seem helpful in determining the presence or absence of LSS. [47]
The classic presentation of LSS is radiating leg pain associated with walking that is relieved by rest (neurogenic claudication). When patients bend forward, the pain diminishes.
Physical examination findings are frequently normal in patients with LSS. Nevertheless, review of the literature suggests diminished lumbar extension appears most consistently, varies less, and constitutes the most significant finding in LSS. Other positive findings include loss of lumbar lordosis and forward-flexed gait. [7]
Fig. 3: Achilles tendon reflexes [2]
Fig. 4: Lumbar extension loading test [3]
Fig. 5: Trendelenbrug sign [3] Fig. 6: Romberg balance test [3]
Medical Management
[edit | edit source]
1) Medication
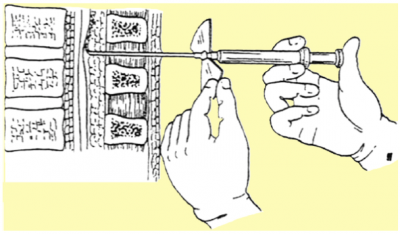
Steroid injections:
Nerve roots may become irritated and swollen at the area where they are pinched. Injecting a corticosteroid into the space around the compression can help reduce the inflammation and relieve some of the pressure. It is suggested that epidural steroid injections help to control severe radicular symptoms in patients with spinal stenosis. However, repeated steroid injections can weaken nearby bones and connective tissue.[12] (level of evidence 3B)
fig. 7: Infusion method of the anaesthetic into the epidural space to treat the radicular symptoms is illustrated. [42] (Level of evidence 5)
Non-steroidal Anti-Inflammatory Medications:
Non-steroidal anti-inflammatory medications (NSAIDs) are commonly prescribed for patients with LSS, and often help relieve pain associated with spinal stenosis. By reducing inflammation, these medications can relieve some of the pressure on compressed nerves. [21] (Level of evidence 2B)
Epidural injections with steroids or with local anesthetic alone provide significant pain relief and functional improvement in managing chronic low back pain secondary to lumbar spinal stenosis, and the inclusion of steroids confers no advantage compared to local anesthetic alone. [45] (Level of evidence 1A)
2) Surgical management
The primary goal of surgery is to decompress the affected roots. According to the individual differences in severity, chronicity and the location, the appropriate type of decompression should be selected. No one procedure can solve all types of stenosis. The principle of surgery is to achieve neural decompression. It is easy to underestimate the extent of the decompression required. [42] (Level of evidence 5)
Over time, surgical treatment has become progressively less invasive.
The following prognostic indicators help to provide the surgeon with realistic expectations of the results of decompression so that the patient can be counselled appropriately. [42] (Level of evidence 5)
Good prognostic factors include:
- Adequate decompression is achieved,
- Facet joint stability is maintained.
- Early decompression surgery is performed,
- Postoperative corset is worn and exercises can be performed.
Poor prognostic factors include:
- Persistence of back pain as a predominating symptom,
- Multi-level decompression,
- Prolonged delay to surgery after onset of symptoms, and
- Preoperative presence of significant neurological deficits including urinary symptoms
Operative techniques:
Decompression by interspinous process distraction devices
This procedure is best indicated for extension dynamic stenosis. The patient should have evidence of relief of symptoms with flexion and worsening of symptoms with extension. [42] (Level of evidence 5)
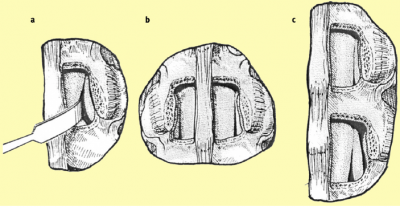
Decompression
The ultimate surgical goal is adequate decompression of the neural structures, including both the cauda equina and exiting nerve roots (Figures 8 and 9). [42] (Level of evidence 5)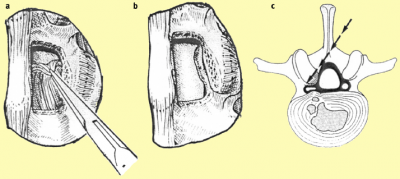
a. After removing the ligamentum flavum bony overgrowth is visualized and can be removed carefully
b. After removal of the medial third of the inferior facet laterally, the superior facet osteophyte can be seen intruding into the lateral recess of the spinal cana
c. The osteophyte can be removed using an osteotome or sharp curette
a. The nerve root previously trapped deep to the superior facet osteophyte will become visible following removal of this osteophyte.
b. The selective decompression can be repeated on the other side of the canal preserving the important midline ligamento-osseous to maintain stability structures
c. The level above can be decompressed if necessary
Fenestration
This is the procedure in which a small bony window is made through which to decompress: the procedure consists of laminectomy and resection of the medial portion (1/3) of the articular facet joints, preserving the joints as much as possible, and complete removal of the ligamentum flavum. It is the method of choice for the majority of patients with LSS, because it preserves spinal stability better than total laminectomy.
Fenestration should always be converted to laminectomy when the procedure does not provide adequate decompression of the central canal. [42] (Level of evidence 5)
Laminectomy
Laminectomy is a more extensive form of decompression surgery, which sacrifices a part or whole of the laminae and facets in one or more segments, more often indicated in the elderly. [42] (Level of evidence 5)
Laminoplastie
En-bloc expansive laminoplasty was introduced by Tsuji, but it is rarely indicated. This procedure is similar to cervical laminoplasty as used to treat cervical myelopathy. [42] (Level of evidence 5)
Physical Therapy Management
[edit | edit source]
LSS patients frequently receive early surgical treatment, although conservative treatment can be a viable option. Not only because of the complications that can arise from surgery, but also because mild symptoms of radicular pain often can be lightened with physical therapy. [39] (level of evidence 3B)
Its specific content and effectiveness relative to other nonsurgical strategies has not been clarified yet. [38] (level of evidence 1A) Postoperative care after spinal surgery is variable, with major differences reported between surgeons in the type and intensity of rehabilitation provided and in restrictions imposed and advice offered to participants. Postoperative management may include education, rehabilitation, exercise, behavioral graded training, neuromuscular training and stabilization training. [40] (level of evidence 1A)
Low quality evidence suggests an improvement in walking ability wearing a lumbar corset in comparison with an elastic woolen corset or no corset. [37] (level of evidence 1A) It can be worn during daily activities that require walking, but only worn for only a limited number of hours each day, otherwise the paraspinal muscles can atrophy [32] (level of evidence 1A).
Furthermore, low quality evidence indicates that modalities such as ultrasound, TENS, heat packs and manual therapy in addition to an exercise program, do not upgrade the active exercises. [37] (level of evidence 1A)
In general, two recent level 1A reviews on literature [38][37] (level of evidence 1A) concluded that there was no consistent evidence for the effectiveness of physical exercise therapy. The specific elements of physical therapy that may benefit should further be examined, as well as the optimal dosage. Cycling and other exercises performed during flexion of the spine, are usually better tolerated than walking. [15]
Steps for therapy:
Patient education:
Patient education is inherent to physical therapy practice and valued by those with clinical experience in the treatment of patients with LSS.
The patient education package comprise:
- the intent of the manual therapy and exercise interventions
- the course of physical therapy
- the purpose of the home exercise program (HEP)
- self-management strategies
- pain sciences information
- prognosis
An anatomical explanation for the patients symptoms may contribute to a fear avoidance of activity and an over medicalization of the problem [26] (level of evidence 2B).
Helpful advice may include items such as:
- temporary avoidance of prolonged overhead activities
- temporary avoidance of prolonged axial loading (standing, use of backpacks, prolonged overhead working postures),
- methods of self lumbo-pelvic flexion and/or rotational stretching techniques for pain control in standing, sitting, and lying.
Basic body mechanics are taught to the patient with LSS, and they should be advised:
- to change positions frequently,
- know and respect their current limits,
- to pace activities such as housework and yard work [44] (level of evidence 2A); [11] (level of evidence 3A).
Finally, patients should be aware of the natural course of this condition and patients should know that the majority of those with LSS do quite well over time, their condition either remaining the same or improving over time with no intervention at all [25] (level of evidence 2B) and that long term results are often no different when comparing those who received surgery for LSS and those who were treated non-surgically [24] (level of evidence 3B), [23] (level of evidence 1B), [22] (level of evidence 4) [44] (level of evidence 2A)
Manual therapy:
A recent systematic review [20] (level of evidence 1A) concluded that the use of manual therapy in conjunction with exercise is of potential benefit for the LSS population. In a randomized controlled trial [34] (level of evidence 1B) they explained that a utilization of manual therapy in a management program is associated with improvements in pain and disability.
Successful results were reported with following techniques:
- flexion–distraction manipulations,
- sidelying lumbar rotation thrust,
- posterior-to-anterior mobilizations,
- sidelying translatoric side bending manipulations,
- thoracic thrusts,
- neural mobilizations [19] (level of evidence 3B), [24] (level of evidence 3B), [23] (level of evidence 1B), [22] (level of evidence 4), [44] (level of evidence 2A) [18] (level of evidence 3B), [35](level of evidence 3A), [30] (level of evidence 4), [27] (level of evidence 2B)
Manual therapy interventions provided in RCT by Whitman et al.
The combined use of manual therapy appears to be an effective intervention. Manual therapy appropriately used involves the lumbar region and thoracic region, pelvis, hips and lower extremities.
The manual therapy approach is impairment-based on thrust and non-thrust mobilization/manipulations to the lumbar and pelvic regions. These interventions frequently emphasize rotation, flexion and distraction, but may involve other techniques dependent upon the individual patient presentation.
Normalization of hip motion appears to be a key element for the successful treatment of patients with LSS. Distraction manipulation of the hip is a valuable intervention technique for restoration of hip motion and function [16] (level of evidence 1B).
Aerobic training and exercise intervention:
Evidenced based guideline from the North American Spine Society concluded through work group consensus that treatment by a physical therapist and exercise may be beneficial for those with LSS and neurogenic claudication [48] (level of evidence 1A).
Exercise prescription based on expert consensus is done with the purposes of providing improved:
- Overall fitness and function (gains in mobility and strength),
- An adjunct to manual therapy techniques
- Increased available cross-sectional area of the spinal canal
- Vascular changes (Helping in treatment of any concomitant peripheral arterial disease)
- Self-management (decreasing fear avoidance issues related to walking).
- Improved pain modulation through stimulation of large motor pathways.
The hemodynamic changes that occur with movement provide a theoretical basis for the positive, symptom-reducing effects of exercise [28] (level of evidence 3B)
Individualized exercises specific to patients with LSS often include components of:
- Unweighted walking or cycling
- Spinal mobility and lumbar flexion exercises
- Hip mobility exercises
- Hip strengthening
- And core strengthening
Unweighted walking or cycling:
Unweighted treadmill walking has been part of a physical therapy plan of care in several studies for patients with LSS [36] (level of evidence 3B);[35] (level of evidence 3A), [34] (level of evidence 1B).
Patients are unweighted to the extent that pain is relieved in order that they can ambulate with good quality movement and pain-free for 30 min [36] (level of evidence 3B). The amount of unweighting is lessened over time as per the patient's response. Fig. 11 shows a patient on the unweighted treadmill. For those who do have unweighting systems available in their clinics, our experience is that patients will have a fairly dramatic response to the unweighting within the first couple of sessions of using the equipment for their aerobic exercise.
If a patient does not have a substantial positive response within the first couple of sessions, we recommend cycling, walking on an inclined treadmill, or other forms of “unloading” such as pool walking. [44] (level of evidence 2A)
In an RCT demonstrated that cycling was just as effective as unweighted treadmill walking; therefore cycling is a viable alternative for use as an in-clinic exercise for those without unweighting equipment. [50] (level of evidence 1b)
Fig. 10. Unweighted treadmill walking.
Spinal mobility and lumbar flexion exercises:
Improved flexibility is frequently a key to intervention, as the presentation of the patient with LSS is often one of overall stiffness. Flexibility impairments can be addressed through manual therapy and self-stretching taught as a home exercise program.
Several case studies and one RCT have used flexion exercises successfully in the treatment of LSS [31] (level of evidence 4); [35] (level of evidence 3A), [34] (level of evidence 1B); [30] (level of evidence 4) and [27] (level of evidence 2B).
Other spinal flexibility exercises typically given to the patient include:
- Thoracic extension
- Self-mobilization
- Stretching exercises
- And lumbar rotation exercises.
Patients often experience immediate relief of lower extremity symptoms with the sidelying lumbar rotation exercise.
One of the first exercises taught to patients is that therapeutic interventions targeted at maximizing thoracic extension. Those are important because, more flexibility in this region should lessen the extension range of motion required of the lumbar spine during standing and with walking. Extension, without concomitant lumbar extension is frequently necessary for pain free ambulation [36] (level of evidence 3B), [44] (level of evidence 2A), [35] (level of evidence 3A), [34] (level of evidence 1B); [29] (level of evidence 5) and [11] (level of evidence 3A).
Hip mobility exercises:
Other muscles around the hip, such as: the hamstrings, rectus femoris, piriformis and tensor fascia latae can become shortened and the patient may respond positively to manual and self-stretching of these muscles. [44] (level of evidence 2A)
Hip strengthening:
Weakness in the hip extensors and abductors complete the picture of typical muscle imbalances in the hip region of the patient with LSS, and should be addressed through a progressive resistive exercise program that is vigorous enough to affect strength change [36] (level of evidence 3B) and [44] (level of evidence 2A)
Core strengthening:
Core strengthening/stabilization is a mainstay of most treatment programs for LBP. Therefore, most patients with LSS are appropriate for some level of core strengthening, especially those with impaired strength or motor control of the abdominal and lumbar musculature. It is expected that most core strengthening will be done with a flexion bias and will attempt to allow the patient to control pelvic position and motion to minimize symptoms while standing and walking [36] (level of evidence 3B); [44] (level of evidence 2A), [35] (level of evidence 3A), [34] (level of evidence 1B); [29] (level of evidence 5) and [11] (level of evidence 3A).
Specifically, patients can be taught to temporarily use a PPT to relieve symptoms, or even to maintain a slight PPT to lessen or avoid symptoms entirely while standing and/or walking.
Specific evidence directing dosage of exercise prescription is lacking in the patient population with LSS.
Exercise is essential to the treatment of the patient with LSS. Therapists must have a wide range of exercises available as patients with LSS present with a wide range of functional levels and frailty.
Key Research[edit | edit source]
Mobbs, R. J., Phan, K., Malham, G., Seex, K., & Rao, P. J. (2015). Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. Journal of Spine Surgery, 1(1), 2-18.
Backstrom, K. M., Whitman, J. M., & Flynn, T. W. (2011). Lumbar spinal stenosis-diagnosis and management of the aging spine. Manual therapy, 16(4), 308-317.
Resources
[edit | edit source]
[1] http://www.rheumatology.org/Practice/Clinical/Patients/Diseases_And_Conditions/Spinal_Stenosis/
[2] http://privyinfo.org/achilles.html
[3] https://www.youtube.com/watch?v=eUJw9pxcV-g
[4] David G. Borenstein, James S. Panagis, Peter C. Gerszten, and James N. Weinstein, Questions and answers about spinal stenosis, National institute of health: http://www.niams.nih.gov/Health_Info/Spinal_Stenosis/#spine_c (level of evidence: 5)
[5] Swiss Spinal Stenosis Questionnaire: http://www.scientificspine.com/spine-scores/swiss-spinal-stenosis-questionnaire.html
[6] http://www.niams.nih.gov/Health_Info/Spinal_Stenosis/#spine_c
[7] http://emedicine.medscape.com/article/1913265-clinical#b3
Clinical Bottom Line[edit | edit source]
Lumbar spinal stenosis is a condition where the spinal canal (central stenosis) or one or more of the lumbar vertebral foramina (foraminal/lateral stenosis) becomes narrowed. If the narrowing is substantial, it can cause compression of the spinal cord or spinal nerves. Symptoms of spinal stenosis include low back pain, buttock pain, leg pain and numbness. These symptoms are typically aggravated by walking and relieved by resting. Interventions that may help relieve symptoms of spinal stenosis and prevent progression of the condition include: patient education, manual therapy, aerobic training and excercise intervention (strenghtening, stretching, mobilization, pelvic tilts and lower back stabilization). If non-operative treatment does not relieve symptoms, surgical treatment may be appropriate. Decompressive posterior laminectomy is the most common type of surgery.
References[edit | edit source]
[8] Cohen et al., The anatomy of the cauda equina on CT scans and MRI, University of California, San Diego (level of evidence: 3B)
[9] Jeffrey N. Katz, et al., Degenerative Lumbar Spinal Stenosis: Diagnostic Value of the History and Physical Examination, 1995, American College of Rheumatology (level of evidence: 3B)
[10] Whitman JM, Flynn TW, Childs JD et al. A Comparison Between Two Physical Therapy Treatment Programs for Patients With Lumbar Spinal Stenosis. SPINE. 2006; 31(22): 2541-49, Department of Physical Therapy, Regis University (level of evidence: 1B)
[11] Vo A, Kamen L, Shih V, Bitar A, Stiti K. Rehabilitation of orthopedic and rheumatologic disorders. 5. Lumbar spinal stenosis. Archives of Physical Medicine and Rehabilitation 2005;86:S69-77.(level of evidence 3A)
[12] Mazanec, D. J., Podichetty, V. K., & Hsia, A. (2002). Lumbar canal stenosis: start with nonsurgical therapy. Cleveland Clinic journal of medicine, 69(11), 909-917. (level of evidence 3B)
[13] Pratt, The Reliability of the Shuttle Walking Test, the Swiss Spinal Stenosis Questionnaire, the Oxford Spinal Stenosis Score, and the Oswestry Disability Index in the Assessment of Patients With Lumbar Spinal Stenosis, 2002 (level of evidence: 2B)
[14] Julie M Fritz, et al., A Nonsurgical Treatment Approach for Patients With Lumbar Spinal Stenosis, 1997, Journal of the American Physical Therapy Association
(level of evidence: 3B)
[15] Katz, J. N., & Harris, M. B. (2008). Lumbar spinal stenosis. New England Journal of Medicine, 358(8), 818-825. ( level of evidence 3B)
[16] Hoeksma H, Dekker J, Ronday H, Heering A, Van Der Lubbe N, Cees V. Comparison of manual therapy and exercise therapy in osteoarthritis of the hip; a randomized clinical trial. Arthritis and Rheumatism 2004;51:722-9 (level of evidence 1B)
[17] SANNA SINIKALLIO, Lumbar spinal stenosis patients are satisfied with short-term results of surgery – younger age, symptom severity, disability and depression decrease satisfaction, 2007, Disability and Rehabilitation (level of evidence: 2B)
[18] Snow G. Chiropractic management of a patient with lumbar spinal stenosis. Journal of Manipulative and Physiologic Therapeutics 2001;24(4):300-4. (level of evidence 3B)
[19] DuPriest C. Nonoperative management of lumbar spinal stenosis. Journal of Manipulative and Physiological Therapeutics 1993;16:411-4. (level of evidence: 3B)
[20] Reiman M, Harris J, Cleland J. Manual therapy interventions for patients with lumbar spinal stenosis: a systematic review. New Zealand Journal of Physiotherapy 2009;37:17-28. (level of evidence: 1A)
[21] Weinstein et al., Surgical versus Nonsurgical Therapy for Lumbar Spinal Stenosis, 2008, The New England Journal of Medicine (level of evidence: 2B)
[22] Atlas S, Keller R, Yen W, Deyo R, Singer D. Long-term outcome of surgical and nonsurgical management of lumbar spinal stenosis: 8- 10 year results form the Maine lumbar spine study. Spine 2005;30:936-43. (level of evidence: 4)
[23] Atlas S, Keller R, Robson D, Deyo R, Singer D. Surgical and nonsurgical management of lumbar spinal stenosis. Spine 2000;25:556-62. (level of evidence: 1B)
[24] Atlas S, Deyo R, Keller R, Chapin A, Patrick D, Long J, et al. The Maine lumbar spine study, part III: 1-year outcome of surgical and nonsurgical management of lumbar spinal stenosis. Spine 1996;21:1787-94. (level of evidence 3B)
[25] Johnsson K, Uden A, Rosen I. The effect of decompression on the natural course of spinal stenosis. A comparison of surgically treated and untreated patients. Spine 1991;16:615-9. (level of evidence 2B)
[26] Breslau J, Seidenwurm D. Socioeconomic aspects of spinal imaging: impact of radiological diagnosis on lumbar spine-related disability. Topics in Magnetic Resonance Imaging: TMRI 2000;11(4):218-23. (level of evidence: 2B )
[27] Murphy D, Hurwitz E, Gregory A, Clary R. A non-surgical approach to the management of lumbar spinal stenosis: a prospective observational cohort study. BMC Musculoskeletal Disorders 2006;7(16). (level of evidence 2B)
[28] Takahashi K, Miyazaki T, Takino T, Matsui T, Tomita K. Epidural pressure measurement. Relationship between epidural pressure and posture in patient with lumbar spinal stenosis. Spine 1995;20:650-3. (level of evidence 3B)
[29] Yuan P, Albert T. Nonsurgical and surgical management of lumbar spinal stenosis. Journal of Bone and Joint Surgery 2004;86-A:2320-8 (level of evidence 5)
[30] Creighton D, Krass J, Marcoux B. Management of lumbar spinal stenosis through the use of translatoric manipulation and lumbar flexion exercises: a case series. Journal of Manual and Manipulative Therapy 2006;14:-1-10 (level of evidence 4)
[31] Fritz J, Erhard R, Vignovic M. A nonsurgical treatment approach for patients with lumbar spinal stenosis. Physical Therapy 1997b;77:962-73. (level of evidence 4)
[32] Costandi et al. Lumbar Spinal Stenosis: Therapeutic Options Review. Pain practice: World Institute of Pain. 2014 (level of evidence: 1A)
[33] Takahashi, Naoto, et al. "Diagnostic value of the lumbar extension-loading test in patients with lumbar spinal stenosis: a cross-sectional study." BMC musculoskeletal disorders 15.1 (2014): 1. (Level of evidence: 3B)
[34] Whitman J, Flynn T, Childs J, Wainner R, Gill H, Ryder M, et al. A comparison between two physical therapy treatment programs for patients with lumbar spinal stenosis. A randomized clinical trial. Spine 2006;31:2541-9. (level of evidence 1B)
[35] Whitman J, Flynn T, Fritz J. Nonsurgical management of patients with lumbar spinal stenosis: a literature review and a case series of three patients managed with physical therapy. Physical Medicine and Rehabilitation Clinics of North America 2003;14:77-101.(level of evidence 3A)
[36] Fritz J, Erhard R, Delitto A, Welch W, Nowakowski P. Prelimary results of the use of a two-stage treadmill test as a clinical diagnostic tool in the differential diagnosis of lumbar spinal stenosis. Journal of Spinal Disorders 1997a;10(5):410-6.(level of evidence 3B)
[37] Macedo, L. et al. Physical Therapy Interventions for Degenerative Lumbar Spinal Stenosis: A Systematic Review. Physical Therapy, 2014, 93(12), 1646-1660. (Level of Evidence 1A )
[38] May, S., & Comer, C. (2013). Is surgery more effective than non-surgical treatment for spinal stenosis, and which non-surgical treatment is more effective? A systematic review. Physiotherapy, 99(1), 12-20. (level of evidence 1A)
[39] Minamide, A., Yoshida, M., & Maio, K. (2013). The natural clinical course of lumbar spinal stenosis: a longitudinal cohort study over a minimum of 10 years. Journal of Orthopaedic Science, 18(5), 693-698. (level of evidence 3B)
[40] McGregor, A. H., Probyn, K., Cro, S., Doré, C. J., Burton, A. K., Balagué, F., ... & Fairbank, J. (2014). Rehabilitation following surgery for lumbar spinal stenosis: a Cochrane review. Spine, 39(13), 1044-1054. (level of evidence 1A)
[41] Kreiner, S., et al. "Evidence-based clinical guidelines for multidisciplinary spine care diagnosis and treatment of degenerative lumbar spinal stenosis. North Am." Spine Soc (2014). (level of evidence: 1A)
[42] Moon, M. S., Kim, S. S., & Sihn, J. C. (2014). Lumbar spinal stenosis–a current view. Orthopaedics and Trauma, 28(6), 396-408. (level of evidence 5 → boek)
[43] Konno, S. I., Kikuchi, S. I., Tanaka, Y., Yamazaki, K., Shimada, Y. I., Takei, H., ... & Kokubun, S. I. (2007). A diagnostic support tool for lumbar spinal stenosis: a self-administered, self-reported history questionnaire. BMC musculoskeletal disorders, 8(1), 1. (level of evidence 2A)
[44] Backstrom, K. M., Whitman, J. M., & Flynn, T. W. (2011). Lumbar spinal stenosis-diagnosis and management of the aging spine. Manual therapy, 16(4), 308-317. (level of evidence 2A)
[45] Meng, H., Fei, Q., Wang, B., Yang, Y., Li, D., Li, J., & Su, N. (2015). Epidural injections with or without steroids in managing chronic low back pain secondary to lumbar spinal stenosis: a meta-analysis of 13 randomized controlled trials. Drug design, development and therapy, 9, 4657. (level of evidence 1A)
[46] Katz, Jeffrey N., et al. "Degenerative lumbar spinal stenosis Diagnostic value of the history and physical examination." Arthritis & Rheumatism 38.9 (1995): 1236-1241. (Level of evidence: 5)
[47] Fritz, Julie M., et al. "Lumbar spinal stenosis: a review of current concepts in evaluation, management, and outcome measurements." Archives of physical medicine and rehabilitation 79.6 (1998): 700-708. (Level of evidence: 3B)
[48] Watters W, Baisden J, Gilbert T, Kreiner S, Resnick D. Degenerative lumbar spinal
stenosis: an evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis. The Spine Journal 2008;8:305-10. (level of evidence: 1A)
[49] Kalichma L. et al, Spinal stenosis prevalence and association with symptoms: The Framingham Study, The Spine Journal, 2009 Jul; 9(7): 545–550. (level of evidence 2B)
[50] Pua YH et al.,"Treadmill walking with body weight support is no more effective than cycling when added to an exercise program for lumbar spinal stenosis: a randomised controlled trial."Aust J Physiother. 2007;53(2):83-9. (level of evidence 1B)
[51] Bhave, Arvind. Modern Techniques in Spine Surgery. JP Medical Ltd, 2014: 317. (Level of evidence: 5)