Low Back Pain and Pregnancy: Difference between revisions
Aiko Deckers (talk | contribs) No edit summary |
Aiko Deckers (talk | contribs) |
||
| Line 21: | Line 21: | ||
<br> | <br> | ||
</div></div></div> | </div></div></div> | ||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
Revision as of 12:31, 7 January 2014
Original Editors - Timothy Assi
Top Contributors - Lynse Brichau, Aiko Deckers, Admin, Brenda Walk, Corin Arundale, Timothy Assi, Christine Utskot, Joanne Garvey, Kim Jackson, Lauren Lopez, Nicole Hills, Chris Slininger, Rachael Lowe, Temitope Olowoyeye, Joshua Samuel, Uchechukwu Chukwuemeka, Evan Thomas, 127.0.0.1, Jeremy Brady, Laura Ritchie and George Prudden
Search Strategy[edit | edit source]
Pubmed, Medline, Web of knowledge, books.
Definition/Description
[edit | edit source]
Pregnancy related low back pain is a common complaint that occurs in 60-70% of pregnancies [21] and can be defined as pain between the 12th rib and the gluteal folds/pubic symphysis during the course of pregnancy. This pain is not the result of a known pathology
such as disc herniation[25] and can begin at any point during pregnancy. Although most cases are mild, approximately one third of women experience severe pain.[11] Pregnancy related low back has been coined multiple times and can be referred to as one of the following patters: Low Back Pain (LBP), Peripartum Posterior Pelvic Pain (PPPP), Pregnancy-related low back pain (PLBP) or pregnancy-related pelvic girdle pain (PPGP). The last two patterns can occur separately or combined.[21]
Unfortunately, there is limited research available regarding physical therapy intervention for pregnant women experiencing Low Back Pain, so a homogenous approach tends to be used. However, back pain is not homogenous; therefore special considerations and precautions should be taken when treating this population.
Figure A: (4)
Clinically Relevant Anatomy[edit | edit source]
The lumbar region is constituted of five unique vertebrae that are designed to withstand increased weight and retain a lordotic curve. The vertebral canal of the lumbar region houses the tail end of the spinal cord and the Cauda Equina.
To maintain stability and provide support, the lumbar region is connected and held secure by an intricate web of ligaments: ligamentum longitudinale anterior and superior, ligamentum flava, ligamentum interspinata, ligamentum intertransversarium and the ligamentum supraspinale. All the mentioned ligaments will provide stability, whereas the longitudinal ligament will also be attached to the intervertebral disc in order to keep the discs in position. Additionally, the lumbar region is supported by strong low back muscles, pelvic muscles and abdominal muscles.
Epidemiology /Etiology[edit | edit source]
A number of reviews investigated the prevalence of low-back pain during pregnancy in different populations. The results are inconsistent, ranging from 8% to more than 89% of women who complain of low back pain during pregnancy.[10][19][20][21][22][23][24]
The exact etiology and pathogenesis of pregnancy related LBP is unknown, but it seems to be the consequence of circulations changes, hormonal and mechanical factors. In addition, previous back pain history, multiple abortions (evidence level 2C) and smoking are considered contributing risk factors that may increase the symptoms.[5][9][22][21][26][17] Some contradictory studies suggest that age, weight and height of the mother, fetal weight, and the number of pregnancies are not risk factors. [23][20]
The prevalence of pregnancy related low-back pain is the highest during the third trimester.[9][24] One of the more common reasons is a condition called Diastasis Rectus Abominis, which is the separation of the Rectus Abdominal at the Linea Alba, leading to poor posture and LBP.[25]
Characteristics/Clinical Presentation[edit | edit source]
There are several possible mechanisms of injury which could be causing pregnancy related LBP. During pregnancy, changes occur in the facet joints, in the back muscles, and in ligaments. This is mainly caused by the increased release of the hormone Relaxin,[11] which causes ligament laxity, and therefore can affect the stability of the spine and lead to back pain.[12]
Another contributor is the increase in weight. On average, about 11-15 kilograms are gained during pregnancy.[12] The weight gain increases the amount of force placed across joints, changes the center of gravity, and forces the patient into an anterior pelvic tilt. The anterior displacement of the center of gravity will cause women to shift their heads and upper body posteriorly over the pelvis, causing hyperlordosis of the lumbar spine. This in turn, places additional stress on the intervertebral discs, ligaments, and facet joints and can lead to joint inflammation.[14][15] In addition, abdominal muscles are stretched and weakened, and the added weight can compress on the lumbosacral plexus.[13]
The most common onset tends to be during the 5th and 6th month of pregnancy, and the pain is usually worse in the evening. About 67% of women experience pain at night. Factors that aggravate the pain include: standing, sitting, coughing or sneezing, walking, and straining during a bowel movement.[15] However pain and a disability of the lumbopelvic region are usually proven to be experienced as mild to moderate, except for a minor part (20%) of the pregnant women that will describe the pain as severe. [28]
Differential Diagnosis[edit | edit source]
Some other diagnoses that can be commonly mistaken for pregnancy related low back pain are: Sciatica, Meralgia Paresthetica, thoracic/rib pain, hip pain, coccygodynia, spontaneous abortions, osteomyelitis, osteoarthritis of spine or hip, Cauda Equina Syndrome, Osteitis Condensans Ilii, metastatic cancers, and Diastasis Rectus Abdominis. Other more common differential diagnoses are: disc disease, facet joint involvement and sacroiliac joint involvement. It is important to be able to recognize the subtle differences and differentiate between the comorbidities.(6)(30)
“Disc Disease - Morning pain and stiffness, pain when weight bearing, pain with increased abdominal pressure, history of repeated micro trauma, pain when going uphill, pain with prolonged sitting, pain with sit to stand activity. Sleep is usually undisturbed, pain eases as day progresses and then gets worse again, movement eases pain but not for long (e.g. fidgets).”(6)
“Facet Joint Involvement - Non weight bearing pain, pain with related to movement (specifically rotation), pain increased by lateral compression, history of minor injury, pain is not usually referred to an extremity, pain eases with rest, not affected by coughing or sneezing”(6)
“Sacroiliac Involvement - Pain is usually unilateral and does not midline, can refer to lower extremities, turning while in supine provokes pain, getting out of the car provokes pain, pain is referred to the groin or genitals, pain is related to menstruation prior to pregnancy because of the effects of cyclic hormones on pre-pregnant SIJ ligaments.”(6)
Diagnostic Procedures[edit | edit source]
In order to formulate the correct diagnosis, the patient should be questioned about her past medical history. It is important to concentrate on experienced symptoms, limitations in activities, and movement possibilities. Questions about past pregnancies such as – "Have you experienced any complications with prior pregnancy(s)?" are appropriate. This will help the therapist understand the patient’s health problems and needs. Knowledge of the anatomical and functional disorders, activity limitations and restriction of participation will help the therapist determine her/his role and the need for appropriate interventions. It is important to recognize red flags complaints and contact a doctor if they are present.[9]
Outcome Measures[edit | edit source]
Different measure instruments can be used in the diagnosis to estimate the complaints more objectively: Visual Analogue Scale (VAS)[10], Roland Disability Questionnaire (RDQ), Impact on Participation and Autonomy (IPA), Photograph series Of Daily Activities (PHODA), and Pain Behavior Scale (PBS).
Examination
[edit | edit source]
Physical Exam
Examination should include observation of the posture and gait, neurologic screen to rule out underlying pathology, range of motion, muscle tests, palpation, muscle length tests, and assessment of joint mobility. Even though theActive Straight Leg Raise test seems accurate, the sensitivity will be elevated when combined with the Posterior Pelvic Pain Provocation (PPPP) test. [27] Special tests can includeFABER and Trendelenberg. The following findings are commonly revealed: Paravertebral muscles are tender to palpation, back muscles weakness, decreased ROM in flexion. The description of the pain is often not localized and may be intermittent. It is possible for the pain to radiate down as far as the calf.[5]
SI Joint Examination: If the patient is unable to stand, instruct the patient to lie in supine and perform a pelvic bridge. The bridge will place the pelvis in neutral - the ASIS’ can be palpated for symmetry.
Medical Management[edit | edit source]
It is important to encourage the patient to receive regular checkups by her obstetrician. During the therapy session, continually check on pain levels and any aches radiating from the low back or stomach. Some patients tolerate pain and discomfort better than others and will therefore mask their distress – Use a chart for Rate of Perceived Exertion to determine the patient's true status and take note of any changes that occur between the begging and end of the session.
Although there are numerous interventions promoted for low back pain during pregnancy, the most common and widely used is a specific exercise program designed by a physical/physiotherapist (see below)[1][2]. Another intervention that is getting tractions and shows prominent research is acupuncture. Recent studies show that a week of continuous acupuncture at specific auricular points can decrease pain and increase the capacity for some physical activity which can help diminish the need for drugs. [3]
Other Interventions:
- side lying while sleeping or resting using a wedge shaped pillow to support stomach
- use of pillow between the legs while side lying (squeeze the pillow/legs together while rolling)
- compression socks to promote venous return and decrease edema
- support belt (The Love Comfort support belt is covered by Medicaid) [6]
- soft tissue massage
- acetaminophen as proscribed by physician
- yoga [7]
- aerobic therapy
- aquatherapy[18 (Level of evidence:1B)]
Physical Therapy Management
[edit | edit source]
“Red flags”(4)
Vaginal bleeding, dizziness/feeling faint, shortness of breath, chest pain, headache, muscles weakness, calf pain or swelling, uterine contractions, decreased fetal movement, vaginal fluid leakage, neurological involvement.
Physical therapy goals:[16]
• Restore biomechanics during daily activities
• Lumbo- Pelvic stabilization
• Advise and prevention
Physical therapy should be focused on the following Strategies:[29]
1) Patient instructions[edit | edit source]
It’s important to communicate with the patient and provide information about the relevant anatomy, ergonomics, back education (to prevent unnecessary mechanical stress on the back), and how to manage ADL activities (walking, standing, sitting, lying, and work position, learning how to control pain). Research shows that when the symptoms are explained, patients can feel more at ease and their anxiety may decrease. [36]
- Using a small pillow between the legs while sitting and rolling in order to stabilize the back.[35]
- Postural correction by standing upright with a neutral posture, avoiding hyperlordosis
- Do not sit or stand for a long time, alternate it with walking or stretching
- Taking breaks and resting in a comfortable position, with the back supported to relieve tired muscles[35]
- Sleeping lying on one side with the top leg on a pillow
- “Use of a small footstool for one foot in sitting or standing, alternate feet”[29]
- Avoiding spine twisting while lifting
2) Physical therapy[edit | edit source]
Stability, coordination and functional preservation should be trained with active back exercises – endurance training for back muscles stabilization.[17] Pelvic tilts, knee pull, straight leg raising, curl up, lateral straight leg raising and water aerobics are recommended because these exercises could relieves lumbar pain in pregnancy.[20] Relaxation exercises while paying close attention to proper respiration also show to be beneficial.(30)
Management includes specific interventions to address pain, weakness, and mobility in the low back region. The Ottawa Panel also recommends massage therapy in order to treat subacute and chronic low back pain. [34]
Manual therapy techniques
| Posterior/Anterior mobilizations in side lying position | Addresses pain and mobility (Grades 1-4). |
Figure C: Walk B. Texas State University's Evidence-based Practice |
| Muscle Energy Technique by resisting hip flexion in side laying while stabilizing the sacrum | Corrects anterior innominate rotation. |
Figure D: Walk B. Texas State University's Evidence-based Practice |
| Spinal manipulation [35] | Are used to relax soft tissues |
Active Exercises
| Strengthening Gluteus Medius |
Position the patient in a side lying and place an elastic around both legs above the knees. Ask the patient to perform an external rotation of her leg in order to strengthen the Gluteus Medius. Perform this exercise on both sides. Feet need to be kept together during the whole exercise. Also, prevent the pelvis from externally rotating. |
Figure E: Walk B. Texas State University's Evidence-based Practice |
| Abdominal Drawing in Maneuver with Physioball (ADIM). |
Ask the patient to sit on a physioball and simulate a walk movement with the lower extremities. This will encourage the back muscle memory to stabilize back during ADL's.
|
Figure F: Walk B. Texas State University's Evidence-based Practice |
| Latissimus dorsi pull-downs |
The patient will be positioned on a physioball, which will force the pelvic, abdomen and back muscles to stay active in order to find a balanced sitting position. This part of the exercise will provoke a contraction of the glutei to increase the strength of the posterior oblique sling muscles which compress the SIJ. Keep the back straight during the whole exercise. |
Figure G: Walk B. Texas State University's Evidence-based Practice |
| Angry Cat [12] | Starting from the hands-and knees-position the patient will move her back up and down. During this exercise it is important to keep the arms stretched out with the hands positioned right under the shoulders and to keep the stomach muscles tight throughout the entire exercise. |
Figure H: [12] |
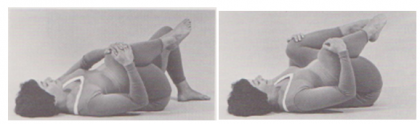
| Pelvic Tilt [12] | Lay down with flexed knees and move the pelvic in an anterior and posterior position. |
Figure I: Women health clinic. Post Natal Exercises. Available at: http://www.pregnancyandchildcare. info/pregnancy_articles/ postnatalexer.html |
Even though most pregnant patients will be advised to exercises within their safe and pain free range, studies show that less than 50% will actually do so. [33] Furthermore it has also been proven that training the rectus abdominus muscles will be useless due to his weakness during the pregnancy.
TENS
There is no strong evidence on the benefits of Tens on Low back pain in pregnancy but it can be used as a supplementary therapy. It’s important to use a low intensity and avoid the acupuncture points which may induce throes. Precautions and contra-indications must be respected.[30][(31 (Evidence level: 1A)]
Patients should take caution when using ultrasound and electrical stimulation and avoid placing those modalities anywhere near the stomach or low back.
Stretching (Level of evidence:1B)
1. Lower Back Stretch: it is plausible that stretching lower back and hip extensor muscles can lead to increased lower back and pelvic flexibility.(12)
Figure J + K: (12) Stahmann Dilfer C.; Your Baby, Your Body (Fitness during pregnancy); Crown publishers, inc., New York, 1977'
Instructions:(12)
a) Clasp your fingers around your right knee.
b) Gently pull your knee as close to your chest as possible. Relax your lower back and try to let your gluts (butt) roll of the floor as you pull.
c) Hold for a slow count of 3.
d) Release.
e) Repeat steps b-d 12-15 times.
f) Now, grasp your left knee, put the right foot flat on the floor and repeat steps b-e
g) Finally, grasp both knees with your hands, and pull both knees close to your chest (or outside your stomach).
h) Repeat steps b-e.
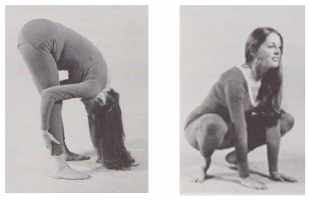
2. Combined squat stretch, back and hamstrings stretch: strengthens thighs (upper legs) and gluts, stretches hamstrings, inner thighs, pelvic floor muscles and back. (12)
Figure L + M: (12) Stahmann Dilfer C.; Your Baby, Your Body (Fitness during pregnancy); Crown publishers, inc., New York, 1977
Instructions:(12)
a) Squat down on your feet, feet pointing at a 45° angle to the sides, heels on the floor.
b) Open your knees wide using thigh muscles and push them apart until they are directly over your feet.
c) Keep your knees back over your feet, and slowly raise your gluts – keep on extending your knees – until your legs are as straight as possible (do not lock out your knees).
d) Relax your head, neck and shoulders.
e) Hold position for 10 counts.
f) Try to keep your knees over your feet and slowly lower your gluts until you return to starting position.
3) Aerobic exercises (Level of evidence: 1B)[edit | edit source]
Walking, swimming1B,Tai chi, recumbent bicycle (or nu-step), are plausible to be beneficial at a low to moderate intensity. The stress on the back should be minimal.(32)
4) Home exercises[edit | edit source]
The exercises explained above could also be performed at home if both the patient and therapist feel confident that the exercises will be performed correctly without supervision.
Back tuck arch [12]: Lean with the back against the wall and alternate between anterior and posterior pelvic tilt.
Figure N: Hughston clinic. Excercising during pregnancy. Available at : http://www.hughston.com/a-11-3-4.aspx
Prognosis (30)
Patients recover from LBP in pregnancy within a few weeks or a few months after childbirth, but symptoms may return during a future pregnancy. Between 8% and 10% of women will continue to experience pain for up to 2 years post-delivery.(30)
Key Research[edit | edit source]
Low back pain pregnancy/pregnant, LBP pregnancy, pregnancy back pain, maternal low back pain, gestation low back pain, pregnancy exercise(s), low back pain causes, low back pain physical therapy.
Resources
[edit | edit source]
Clinical Bottom Line[edit | edit source]
The majority of pregnant women experience low back pain. Appropriate examination, interventions and follow up, can help in managing the pain. Key questions must be asked and special modifications must be made for more complex patient experiencing pregnancy related back pain. As patient centered practitioners, it is our job to research and implement evidence based practice to increase outcomes with minimal number of treatments.
Recent Related Research (from Pubmed)
[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=14MpKbWO9zvFebubT4UTZKZm_0Q0VJ_VKdfcgw_JcJ0AWU29XI|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
(1) Stuge B, Hilde G, Vollestad N. Physical therapy for pregnancy related low back and pelvic pain: a systematic review. Acta Obstet Gynecol Scand. 2003;82:983–990. [PubMed] (Evidence level: 2A)
(2) Mens JM, Snijders CJ, Stam HJ. Diagonal trunk muscle exercises in peripartum pelvic pain: a randomized clinical trial. Phys Ther. 2000;80:1164–1173. [PubMed] (Evidence level: 1B)
(3) Wang SM, Dezinno P, Lin EC, Lin H, Yue JJ, Berman MR, et al. Auricular acupuncture as a treatment for pregnant women who have low back and posterior pelvic pain: a pilot study. Am J Obstet Gynecol. 2009;201:271–e271. [PMC free article] [PubMed] (Evidence level: 3B)
(4) Perkins J, Hammer RL, Loubert PV. Identification and management of pregnancy-related low back pain. J Nurse Midwifery. 1998;43:331–340. [PubMed] (Evidence level: 2A)
(5) Sneag D, Bendo J. Pregnancy-related low back pain. Orthopedics. 2007; 30: 839-845. (Evidence level: 1A)
(6) Sandler SE. The Management of Low Back Pain in Pregnancy. Manual Therapy. 1996; 1(4):178-1857 Diagnostic Procedures15 Recent Related Research [PubMed] (Evidence level: 3A)
(7) Ehrlich G., Low Back pain. Bulletin of the World Health Organization 2003, 81 (9) (Evidence level: 2C)
(8) Cullaty M. Suspected Sacroiliac Joint Dysfunction: Modifying Examination and Intervention During Pregnancy. Journal of Women's Health Physical Therapy. 2006; 30(2): 18-24 (Evidence level: 2C)
(9) GE Bekkering PT MSc, HJM Hendriks PT PhD, BW Koes PhD, RAB Oostendorp PT MT PhD, RWJG Ostelo PT MSc, JMC Thomassen PT, MW van Tulder PhD.; National practice guidelines for physical therapy in patients with low back pain (Evidence level: 2C)
(10) M. Ronald, J.R. Jenner. Back pain New approaches to rehabilitation and education. Manchester university press. 1989;258 pages (Evidence level: 2B)
(11) Hall J, Cleland J, Palmer J. The Effects of Manual Physical Therapy and Therapeutic Exercise on Peripartum Posterior Pelvic Pain: Two Case Reports. Journal of Manual and Manipulative Therapy. 2005;13(2): 94-102 (Evidence level: 3B)
(12) Stahmann Dilfer C.; Your Baby, Your Body (Fitness during pregnancy); Crown publishers, inc., New York, 1977 (Evidence level: 5 )
(13) Gilleard W. L., Brow J.M. Structure and function of the abdominal muscles in primigravid subjects during pregnancy and the immediate postbirth period. Physical Therapy, 1996; 750-62 (Evidence level: 2B)
(14) Russell R.,Reynolds F. Back pain, pregnancy, and childbirth. British medical journal. 1997;1059-1064. (Evidence level: 5)
(15) To W. W. K., Wong M. W. N. . Factors associated with back pain symptoms in pregnancy and the persistence of pain 2 years after pregnancy. Acta Obstetricia et Gynecologica Scandinavica. 2003; 1086-91.(Evidence level: 2B)
(16) Stuge B., Hilde G., Vollestad N. . Physical therapy for pregnancy-related low back and pelvic pain: a systematic review. Acta Obstet Gynecol Scand 2003: 82: 983—990 (Evidence level: 1A)
(17) Horst Eggen M., Stuge B., Mowinckel P. , Smee Jensen K., Hagen K.B. . Can Supervised Group Exercises Including Ergonomic Advice Reduce the Prevalence and Severity of Low Back Pain and Pelvic Girdle Pain in Pregnancy? A Randomized Controlled Trial. PHYS THER. 2012; 92:781-790. (Evidence level: 1B)
(18) Granath AB, Hellgren MS, Gunnarsson RK, Water aerobics reduces sick leave due to low back pain during pregnancy. J Obstet Gynecol Neonatal Nurs. 2006 Jul-Aug;35(4):465-71 (Evidence level: 1B)
(19) Endresen EH. Pelvic pain and low back pain in pregnant women – an epidemiological study. Scan J Rheumatol. 1995; 24: 135–41. (Evidence level: 3A)
(20) Bastiaanssen JM, de Bie RA, Bastiaenen CH, Essed GG, van den Brandt PA. A historical perspective on pregnancy-related low back and/or pelvic girdle pain. Eur J Obstet Gynecol Reprod Biol. Maastricht. 2005 (Evidence level: 2C)
(21) Mogren IM, Pohjanen AI. Low back pain and pelvic pain during pregnancy: prevalence and risk factors. Spine . 2005 Apr 15;30(8);983-91. (Evidence level: 2C)
(22) Ostgaard HC, Andersson GBJ, Karlsson K. Prevalence of back pain in pregnancy. Spine 1991; 16: 549–52. (Evidence level: 2C)
(23) Orvieto R, Achiron A, Ben-Rafael Z, Gelernter I, Achiron R. Low back pain of pregnancy. Acta Obstet Gynaecol Scand. 1994; 73: 209–14. (Evidence level: 4)
(24) Ansari NN, Hasson S, Naghdi S, Keyhani S, Jalaie S. Low back pain during pregnancy in Iranian women: Prevalence and risk factors. Physiotherapy Theory and Practice, 26(1):40–48, 2010 (Evidence level: 2C)
(25) Jeffcoat H. Exercises for low back pain in pregnancy. Int J Childbirth Educ. 2008; 23: 9-12. (Evidence level: 5)
(26) Ostgaard HC, Andersson GBJ. Previous back pain and risk of developing back pain in a future pregnancy. Spine 1991; 16: 433–6. (Evidence level: 2C)
(27) Mens JM, Huis YH, et al. Technical and measurement report: The Active Straight Leg Raise test in lumbopelvic pain during pregnancy. Manual Therapy 17 (2012) 364e368 (Evidence level: 2C)
(28) Mens JM, Huis YH, et al. Severity of signs and symptoms in lumbopelvic pain during pregnancy. Manual Therapy 17 (2012) 175e179 (Evidence level: 2C)
(29) Haugland K. S. , Rasmussen S., Daltveit A. K. .Group intervention for women with pelvic girdle pain in pregnancy. A randomized controlled trial, Acta Obstetricia et Gynecologica. 2006; 85: 1320 1326 (Evidence level: 1B)
(30) Vermani E., FRCA*; Mittal R, FRCS†; Weeks A., MRCO Pelvic Girdle Pain and Low Back Pain in Pregnancy: A Review, Pain Practice, Volume 10, Issue 1, 2010 60–71 (Evidence level: 3A)
(31) Khadilkar A, Odebiyi DO, Brosseau L, Wells GA. Transcutaneous electrical nerve stimulation (TENS) versus placebo for chronic low-back pain. Cochrane Database Syst Rev. 2007;3:CD003008. (Evidence level: 1A)
(32) Field T., Prenatal exercise research, Infant Behavior & Development 35 (2012) 397– 407 (Evidence level: 2A)
(33) George JW, Skaggs CD, Thompson PA, Nelson DM, Gavard JA, Gross GA. A randomized controlled trial comparing a multimodal intervention and standard obstetrics care for low back and pelvic pain in pregnancy. Am J Obstet Gynecol 2013;208(4):295.e1-7. Epub 2012 Oct 23. (Evidence level: 1B)
(34) Brosseau L., Wells G., et al. Ottawa Panel evidence-based clinical practice guidelines on therapeutic massage for low back pain. Journal of Bodywork and Movement Therapies
Volume 16, Issue 4 , Pages 424-455, October 2012 (Evidence level: 1B)
(35) Katonis P., Review article: Pregnancy-related low back pain. Hippokratia 2011, 15, 3: 205-210 (Evidence level: 2A)
(36) Oswald C, Higgins C. eta al. , Optimizing pain relief during pregnancy using manual therapy. Canadian Family Physician August 2013 vol. 59 no. 8 841-842. [PubMed] (Evidence level: 3A)