Legg-Calve-Perthes Disease: Difference between revisions
Fien Wijnant (talk | contribs) No edit summary |
Fien Wijnant (talk | contribs) No edit summary |
||
| Line 67: | Line 67: | ||
A MRI is usually obtained to confirm the diagnosis; however x-rays can also be of use to determine femoral head positioning. | A MRI is usually obtained to confirm the diagnosis; however x-rays can also be of use to determine femoral head positioning. | ||
== Outcome Measures | == Outcome Measures == | ||
The Lower Extremity Functional Scale is one that measures how | <u>Questionnaires</u><br>The questionnaires below can be used to assess the initial function of a person and progress and outcome of operative as well as non-operative treatments. The surveys test the patient on a functional level are useful to provide a baseline and monitor functional progress in the patient’s activities. | ||
<u></u><u>The lower extremity functional scale (LEFS)</u><br>The Lower Extremity Functional Scale (LEFS) is one that measures initial function, ongoing progress and outcome for a wide range of lower-extremity conditions but can be used to evaluate LCPD in children. In other words it evaluates how the disease is affecting the child in a functional way. The LEFS is a self-report questionnaire about having difficulties with everyday activities (i.e. running, hopping, etc). The maximum score is 80 points, the minimum is 0 for which 80 stands for high functionality and 0 for very low functionality.<br>For more information about this questionnaire, click on the link below.<references /><br> <br>http://www.physio-pedia.com/Lower_Extremity_Functional_Scale_(LEFS) | |||
<u>8.2 The Harris Hip Score </u><br>The Harris Hip score is another questionnaire that’s intended to evaluate all kinds of hip disabilities and methods of treatment but is mostly used in an adult population but can easily be used for children. <references />The Harris hip score covers various domains listed below:<br>- Pain: measuring pain severity and the adverse effect on activities and necessity of pain medication<br>- Function: Covers the ability of the person to partake in daily activities such as stair walking, taking public transportation, sitting and being able to get dressed. <br>- Absence of deformity: hip flexion, adduction, internal rotation and extremity length discrepancy.<br>- Range of motion: measures hip flexion, ab- and adduction and in- and external rotation. | |||
The questionnaire consists of questions using a unique numerical scale. The Harris Hip score has a total of 100 points. The higher the HHS the less dysfunction.<br>A total score of:<br> <70: poor<br> 70 – 80: fair<br> 80-90: good<br> 90-100: excellent | |||
The questionnaire takes 5 minutes to complete and an example is shown in the link below: http://www.orthopaedicscore.com/scorepages/harris_hip_score.html | |||
For more info about the Harrison Hip score on Physiopedia click on the link <br>http://www.physio-pedia.com/Harris_Hip_Score | |||
8.3 Hip Disability and osteoarthritis outcome score (HOOS)<br>HOOS is an instrument developed to assess the patient’s opinion about their hip and associated problems. The HOOS consists of 5 subscales: pain, other symptoms, function in activities of daily living (ADL), function in sport and recreation and hip-related quality of life (QOL). The questionnaire covers 40 items divided over the 5 subscales. Standardized answer options are given (5 Likert boxes). Each question has a score from 0 to 4. Scores are summarized for each subscale: from 0 to 100. 0 indicates extreme problems and 100 indicates no problems at all. The HOOS is suggested to be valuable for younger and more active people due to the subscales. [40,41] | |||
As for the difference in outcome for nonoperative and operative treatments a meta-analysis performed in 2012 suggests that operative treatment is more likely to yield a spherical congruent femoral head than non-operative methods among six year olds or older. For patients who are younger than the age of six, operative and non-operative methods have the same likelihood to yield a good outcome. Children who were six years or older who were treated operatively had the same likelihood of a good radiographic outcome regardless of surgical intervention with a femoral or pelvic procedure. Patients younger than six had a greater benefit from pelvic procedures than femoral procedures.[42]<br> | |||
== Examination == | == Examination == | ||
Revision as of 15:21, 10 January 2017
Original Editor - Pamela Gonzalez, Bahire Evelyne
Lead Editors - Sarah Haerinck, Admin, Evelyne Bahire, Pamela Gonzalez, Lucinda hampton, Fien Wijnant, Samuel Adedigba, Lauren Kwant, Abbey Wright, Rachael Lowe, Olajumoke Ogunleye, Simisola Ajeyalemi, Kim Jackson, 127.0.0.1, Benjamin Desmedt, Rucha Gadgil, Wanda van Niekerk, Eric Robertson, Blessed Denzel Vhudzijena, Vidya Acharya, Meaghan Rieke, Jess Bell and Glenn Demeyer
Definition/Description[edit | edit source]
Legg-Calvé-Perthes disease (LCPD) is an idiopathic juvenile avascular necrosis of the femoral head in a skeletally immature patient, i.e. children. Legg-Calvé and Perthes discovered this disease approximately 100 years ago. [1]The disease affects children from ages of two to fourteen.
The disease can lead to permanent deformity and premature osteoarthritis. The hip disorder is initiated by an interruption in blood supply to the femoral head. As the blood vessels around the femoral head disappear and cells die, the bone also dies and stops growing. When the healing process begins new blood vessels begin to remove dead bone (the bone gets absorbed by the body) This leads to a decrease in bone mass and a weaker femoral head. It can also lead to deformity of the bone because new tissue and bone replace the necrotic bone.. [2]
The bone death appears in the femoral head due to an interruption in blood supply. As bone death appears, the ball develops a fracture of the supporting bone. This fracture indicates the outset of bone reabsorption by the body. As bone is slowly absorbed, it is replaced by new tissue and bone.[3] [4]
Other names are: ischemic necrosis of the hip, coxa plana, osteochondritis and avascular necrosis of the femoral head. [3]
Many aspects of the disease remain unknown or are unclear, including etiology but many factors may be involved including gender, genetics, socioeconomic status and environment. Also the pathophysiology of best methods for treatment of patients in different age groups affected with the disease is unclear. [5][6]
Clinically Relevant Anatomy[edit | edit source]
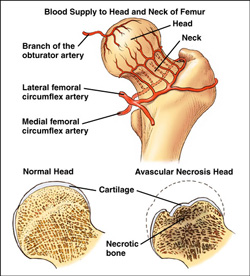
The femoral head is supplied with blood from the medial circumflex femoral and lateral circumflex femoral arteries, which are branches of the profunda femoris artery.
- The medial femoral circumflex artery: extends posteriorly and ascends proximally deep to the quadratus femorus muscle.
At the level of the hip it joins an arterial ring at the base of the femoral neck. - The lateral femoral circumflex artery: extends anteriorly and gives off an ascending branch,
which also joins the arterial ring at the base of the femoral neck.
This vasculare ring gives rise to a group of vessels which run in the retinacular tissue inside the capsule to enter the femoral head at the base of the articular surface.
There is also a small contribution from a small artery in the ligamentum teres to the top of the femoral head which is a branch of the posterior division of the obturator artery.
Epidemiology /Etiology[edit | edit source]
The origin of Perthes’ disease is unknown, there is consensus however concerning the pathology.
First, there is interrupted blood supply to the capital femoral epiphysis. After this, an infraction of the subchondral bone occurs. Next, revascularization of the area occurs and new bone ossification begins. This is the turning point where a percentage of patients will have normal bone growth and development; while others will develop Legg Calve Perthes Disease. (LCPD). This disease is present when a subchondral fracture occurs. Usually, there is no trauma to cause this scenario. LCPD is most commonly the result of normal physical activity. Because of the subchondral fracture, changes occur to the epiphyseal growth plate.
Classification:
Severity and prognosis of the disease is determined by using a variety of classification systems.
Two of the classification systems are listed here.
- The Catteral Classification specifies four different groups to define radiographic appearance during the period of greatest bone loss. These four groups are reduced down to two by the Salter-Thomson Classification. The first group, which is Group A (Catteral I,II) shows less than 50% of the ball is involved. Group B (Catteral III, IV) shows that more than 50% of the ball is involved. If there is less than 50% involvement the prognosis is good; if there is more than 50% there is usually a poor prognosis.
- The Herring Classification is based on the integrity of the lateral pillar of the caput femoris. Group A of this classification shows no loss of height in the lateral 1/3 of the head and little density change. In Lateral Pillar Group B, there is less than 50% loss of lateral height and lucency is present in the joint. In some cases, the ball is beginning to extrude the socket. In Lateral Pillar Group C, there is more than 50% loss of lateral height.
There are four phases of Legg-Calve Perthes Disease which are as follows:
- Increased density of femoral head possibly leading to fractures
- Bone undergoes fragmentation and reabsorption
- Growth of new bone
- Reshaping of new bone
Characteristics/Clinical Presentation[edit | edit source]
LCP disease is present in children 2-13 years of age and there is a four times greater incidence in males compared to females. The average age of occurrence is six years.
- The limp: A psoatic limp is typically present in these children secondary to weakness of the psoas major. The limp:[7] is worse after physical activities and improves following periods of rest. The limp becomes more noticeable: late in the day, after prolonged walking.
- The pain: [7] The child is often in pain during the acute [2]. The pain is usually worse late in the day and with greater activity.[7] Night pains is frequent.[7]
- ROM: The child will show a decrease in extension and abduction active ranges of motion. There is also a limited internal rotation in both flexion and extension in the early phase of the disease [8]
- Unusual high activity level: [9] Children with Legg-Calvé-Perthes disease are usually, physically very active, and a significant percentage has true hyperactivity or attention deficit disorder.
- Abnormal growth patterns: [10] General pattern: The forearms and hands are relative short compared to the upper arm. [11] The feet are relatively short compared to the tibia. [11]Differential Diagnosis
Listed are some other disorders that should be included in the differential diagnosis for LCPD:
- Septic arthritis-This is an infection in the joint
- Sickle cell-Osteonecrosis of the hip can be a result of this disease
- Spondyloepiphyseal Dysplasia Tarda-This disease typically affects the spine and the larger more proximal joints
- Gaucher’s Disease- This is a genetic disorder that often times includes bone pathology
- Transient Synovitis-This is an acute inflammatory process and is the most common cause of hip pain in childhood
Diagnostic Procedures[edit | edit source]
A MRI is usually obtained to confirm the diagnosis; however x-rays can also be of use to determine femoral head positioning.
Outcome Measures[edit | edit source]
Questionnaires
The questionnaires below can be used to assess the initial function of a person and progress and outcome of operative as well as non-operative treatments. The surveys test the patient on a functional level are useful to provide a baseline and monitor functional progress in the patient’s activities.
The lower extremity functional scale (LEFS)
The Lower Extremity Functional Scale (LEFS) is one that measures initial function, ongoing progress and outcome for a wide range of lower-extremity conditions but can be used to evaluate LCPD in children. In other words it evaluates how the disease is affecting the child in a functional way. The LEFS is a self-report questionnaire about having difficulties with everyday activities (i.e. running, hopping, etc). The maximum score is 80 points, the minimum is 0 for which 80 stands for high functionality and 0 for very low functionality.
For more information about this questionnaire, click on the link below.
- ↑ Lynn T. Staheli. Practice of Pediatric Orthopedics. 2nd ed. Philadelphia: Lippincott Williams &amp;amp;amp;amp; Wilkins, 2006 p.182-183
- ↑ 2.0 2.1 Lynn T. Staheli. Practice of Pediatric Orthopedics. 2nd ed. Philadelphia: Lippincott Williams &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Wilkins, 2006 p.182-183 Cite error: Invalid
<ref>tag; name "Lynn T. Staheli" defined multiple times with different content - ↑ 3.0 3.1 http://www.nonf.org/perthesbrochure/perthes-brochure.htm
- ↑ http://www.nonf.org/perthesbrochure/perthes-brochure.htm
- ↑ Torsten Johansson, Maria Lindblad, Marie Bladh, Ann Josefsson & Gunilla Sydsjö (2016): Incidence of Perthes’ disease in children born between 1973 and 1993, Acta Orthopaedica
- ↑ Kim, H. K. (2012). Pathophysiology and new strategies for the treatment of Legg-Calvé-Perthes disease. J Bone Joint Surg Am, 94(7), 659-669.
- ↑ 7.0 7.1 7.2 7.3 John Anthony Herring, MD, editors. Legg-Calvé-Perthes Disease. Rosemont; American Academy of Orthopaedic Surgeons; 1996 p. 6-16
- ↑ Dennis R. Wenger, MD, W. Timothy Ward, MD, John A. Herring, MD. Current Concepts Review Legg-Calvé-Perthes Disease. The Journal of Bone and Joint Surgery; 1991 73:778-788
- ↑ Loder, Randall T. M.D.; Schwartz, Edward M. Ph.D. *; Hensinger, Robert N. M.D. Behavioral Characteristics of Children with Legg-Calve-Perthes Disease J of Pediatric J of Pediatric Orthopeadics: September/October 1993 13(5):676-700
- ↑ Burwell RG. Perthes' disease: growth and aetiology. Arch Dis Child 1988 ; 63(11): 1408-1412
- ↑ 11.0 11.1 Burwell RG, Dangerfield PH, Hall DJ, Vernon CL, Harrison MHM. Perthes' disease. An anthropometric study revealing impaired and disproportionate growth. J Bone Joint Surg [Br] November 1978;60-B(4) :461-477
http://www.physio-pedia.com/Lower_Extremity_Functional_Scale_(LEFS)
8.2 The Harris Hip Score
The Harris Hip score is another questionnaire that’s intended to evaluate all kinds of hip disabilities and methods of treatment but is mostly used in an adult population but can easily be used for children. The Harris hip score covers various domains listed below:
- Pain: measuring pain severity and the adverse effect on activities and necessity of pain medication
- Function: Covers the ability of the person to partake in daily activities such as stair walking, taking public transportation, sitting and being able to get dressed.
- Absence of deformity: hip flexion, adduction, internal rotation and extremity length discrepancy.
- Range of motion: measures hip flexion, ab- and adduction and in- and external rotation.
The questionnaire consists of questions using a unique numerical scale. The Harris Hip score has a total of 100 points. The higher the HHS the less dysfunction.
A total score of:
<70: poor
70 – 80: fair
80-90: good
90-100: excellent
The questionnaire takes 5 minutes to complete and an example is shown in the link below: http://www.orthopaedicscore.com/scorepages/harris_hip_score.html
For more info about the Harrison Hip score on Physiopedia click on the link
http://www.physio-pedia.com/Harris_Hip_Score
8.3 Hip Disability and osteoarthritis outcome score (HOOS)
HOOS is an instrument developed to assess the patient’s opinion about their hip and associated problems. The HOOS consists of 5 subscales: pain, other symptoms, function in activities of daily living (ADL), function in sport and recreation and hip-related quality of life (QOL). The questionnaire covers 40 items divided over the 5 subscales. Standardized answer options are given (5 Likert boxes). Each question has a score from 0 to 4. Scores are summarized for each subscale: from 0 to 100. 0 indicates extreme problems and 100 indicates no problems at all. The HOOS is suggested to be valuable for younger and more active people due to the subscales. [40,41]
As for the difference in outcome for nonoperative and operative treatments a meta-analysis performed in 2012 suggests that operative treatment is more likely to yield a spherical congruent femoral head than non-operative methods among six year olds or older. For patients who are younger than the age of six, operative and non-operative methods have the same likelihood to yield a good outcome. Children who were six years or older who were treated operatively had the same likelihood of a good radiographic outcome regardless of surgical intervention with a femoral or pelvic procedure. Patients younger than six had a greater benefit from pelvic procedures than femoral procedures.[42]
Examination[edit | edit source]
1. The limp:
The limp is usually antalgic.[1]
It is possible that the child has a Trendelenburg gait (a positive Trendelenburg test on the affected side) which is marked by a pelvic drop on the unloaded side during single stance. [2]
The child can also have a Duchenne gait, which is marked by a trunk lean toward the stance limb with the pelvis level or elevated on the unloaded side. [2]
2. Range of motion: [1]
The restriction of hip motion is variable in the early stages of the disease;
Many patients, may only have a minimal loss of motion at the extremes of internal rotation and abduction.
At this stage there usually is no flexion contracture.
Loss of hip ROM in patients with early Perthes’ disease without intra-articular incongruity is due to pain and muscle spasm. [3]
This is why, if the child is examined for instance after a night of bed rest, the range will be much better then later in the day.
Further into the disease process;
Children with mild disease may maintain a minimal loss of motion at the extremes only and thereafter regain full mobility.
Those with more severe disease will progressively lose motion, in particular abduction and internal rotation.
Late cases may have adduction contractures and very limited rotation, but the range of flexion and extension is only seldom compromised.
3. Pain: [1] Pain occurs during the acute disease.[4] The pain may be located in the groin, anterior hip area, or around the greater trochanter. Referral of pain to the knee is common.
4. Atrophy: [1]
In most cases there is atrophy of the gluteus, quadriceps[5] and hamstring muscles, depending upon the severity and duration of the disorder.
Medical Management
[edit | edit source]
Medications include nonsteroidal anti-inflammatory medication (NSAIDs) for pain and/or inflammation.
Physical Therapy Management
[edit | edit source]
There is no consensus concerning the possible benefits of physiotherapy in LCP disease, or in which phase of the development of the health problem it should be used.
Some studies mention physiotherapy as a pre- and/or postoperative intervention, while others consider it a form of conservative treatment associated with other treatments, such as skeletal traction, orthesis, and plaster cast.
In studies comparing different treatments[6], physiotherapy was applied in children with a mild course of the disease. The characteristics of the patients were:
- Children with less than 50% femoral head necrosis (Catterall groups 1 or 2) [6]
- Children with more than 50% femoral head necrosis, under six years, whose femoral head cover is good (>80%)[6]
- Herring type A or B[7]
- Salter Thompson type A[7]
For patients with a mild course, physiotherapy can produce improvement in articular range of motion, muscular strength and articular dysfunction[7]. The physiotherapeutic treatment included:
- Passive mobilisations for musculature stretching of the involved hip.
- Straight leg raise exercises, to strengthen the musculature of the hip involved for the flexion, extension, abduction, and adduction of muscles of the hip.
- They started with isometric exercises and after eight session, isometric exercises.
- A balance training initially on stable terrain, and later on unstable terrain.
For children over 6years at diagnosis with more than 50% of femoral head necrosis, proximal femoral varus osteomy gave a significantly better outcome than orthosis and physiotherapy[6].
Recent Related Research (from Pubmed)[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 John Anthony Herring, MD, editors. Legg-Calvé-Perthes Disease. Rosemont; American Academy of Orthopaedic Surgeons; 1996 p. 6-16
- ↑ 2.0 2.1 Bettina Westhoff, Andrea Petermann, Mark A. Hirsch, Reinhart Willers, Rudiger Krauspe. Computerized gait analysis in Legg Calve Perthes disease - Analysis of the frontal plane. Gait &amp;amp;amp;amp;amp;amp;amp; Posture October 2006; 24 (2):196-202
- ↑ Carl L. Stanitski. Hip range of motion in Perthes’ disease: comparison of pre-operative and intra-operative values. J Child Orthop March 2007; 1(1):33-35
- ↑ Lynn T. Staheli. Practice of Pediatric Orthopedics. 2nd ed. Philadelphia: Lippincott Williams &amp;amp;amp;amp;amp;amp;amp; Wilkins, 2006 p.182-183
- ↑ Simon G. F. Robben, Maarten H. Lequin, Morteza Meradji, Ad F. M. Diepstraten,Wim C. J. Hop. Atrophy of the quadriceps muscle in children with a painful hip. Clinical physiology 1999; 19(5):385-393
- ↑ 6.0 6.1 6.2 6.3 O. Wiig, T. Terjesen, S. Svenningsen. Prognostic factors and outcome of treatment in Perthes’ disease. The Journal Of Bone And Joint Surgery October 2008; 90-B(10):1364-1371 (level of the evidence 2B)
- ↑ 7.0 7.1 7.2 Brecht GC, Guarnieiro R. Evaluation of physiotherapy in the treatment of Legg-Calvé-Perthes disaese. Clinics 2006;61(6):521-528 (level of the evidence 2B)