Introduction to Vestibular Rehabilitation: Difference between revisions
m (Protected "Introduction to Vestibular Rehabilitation" ([Edit=Allow only autoconfirmed users] (indefinite) [Move=Allow only autoconfirmed users] (indefinite))) |
No edit summary |
||
| Line 13: | Line 13: | ||
Vestibular disturbance is a significant issue globally. It is estimated that 35.4 percent of North Americans aged over 40 have experienced some form of vestibular dysfunction. The likelihood of experiencing vestibular dysfunction increases with age.<ref name=":1">Agrawal Y, Carey JP, Della Santina CC, Schubert MC, Minor LB. [https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/773517 Disorders of balance and vestibular function in US adults: data from the National Health and Nutrition Examination Survey, 2001-2004]. Arch Intern Med. 2009;169(10):938-44. </ref> | Vestibular disturbance is a significant issue globally. It is estimated that 35.4 percent of North Americans aged over 40 have experienced some form of vestibular dysfunction. The likelihood of experiencing vestibular dysfunction increases with age.<ref name=":1">Agrawal Y, Carey JP, Della Santina CC, Schubert MC, Minor LB. [https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/773517 Disorders of balance and vestibular function in US adults: data from the National Health and Nutrition Examination Survey, 2001-2004]. Arch Intern Med. 2009;169(10):938-44. </ref> | ||
* 80 percent of people aged over 65 years experience dizziness - in 50 percent of cases this dizziness is caused by benign paroxysmal positional vertigo (BPPV)<ref name=":1" /> | * 80 percent of people aged over 65 years experience dizziness - in 50 percent of cases this dizziness is caused by [[Benign Positional Paroxysmal Vertigo (BPPV)|benign paroxysmal positional vertigo (BPPV)]]<ref name=":1" /> | ||
* 75 percent of adults aged over 70 years have a balance impairment (often associated with vestibular dysfunction and sensory loss in the feet)<ref name=":2">Hall CD, Herdman SJ, Whitney SL, Cass SP, Clendaniel RA, Fife TD et al. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4795094/ Vestibular rehabilitation for peripheral vestibular hypofunction: An evidence-based clinical practice guideline: FROM THE AMERICAN PHYSICAL THERAPY ASSOCIATION NEUROLOGY SECTION]. J Neurol Phys Ther. 2016;40(2):124-55.</ref> | * 75 percent of adults aged over 70 years have a balance impairment (often associated with vestibular dysfunction and sensory loss in the feet)<ref name=":2">Hall CD, Herdman SJ, Whitney SL, Cass SP, Clendaniel RA, Fife TD et al. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4795094/ Vestibular rehabilitation for peripheral vestibular hypofunction: An evidence-based clinical practice guideline: FROM THE AMERICAN PHYSICAL THERAPY ASSOCIATION NEUROLOGY SECTION]. J Neurol Phys Ther. 2016;40(2):124-55.</ref> | ||
* Nearly 85 percent of adults aged over 80 years have vestibular dysfunction<ref name=":2" /> | * Nearly 85 percent of adults aged over 80 years have vestibular dysfunction<ref name=":2" /> | ||
| Line 31: | Line 31: | ||
Dizziness and vertigo are both purely subjective phenomena. There is no objective means of measuring them, so the patient’s subjective history is key.<ref name=":0" /> | Dizziness and vertigo are both purely subjective phenomena. There is no objective means of measuring them, so the patient’s subjective history is key.<ref name=":0" /> | ||
== Causes of Dizziness == | |||
There are many causes of dizziness including: | |||
* Cardiovascular dysfunction<ref name=":0" /> | |||
** Strokes are a rare cause of dizziness. The figures vary, but recent reports suggest strokes are the underlying cause of symptoms in around 3 to 5 percent of patients visiting emergency departments with dizziness and vertigo<ref name=":3">Saber Tehrani AS, Kattah JC, Kerber KA, Gold DR, Zee DS, Urrutia VC et al. [https://www.ahajournals.org/doi/full/10.1161/STROKEAHA.117.016979 Diagnosing stroke in acute dizziness and vertigo: pitfalls and pearls]. Stroke. 2018;49(3):788-795. </ref> | |||
** Orthostatic hypotension | |||
** Arrhythmias | |||
* Neurological dysfunction<ref name=":0" /> | |||
** Dizziness is a common symptom associated with [[MS Multiple Sclerosis|multiple sclerosis]] (MS)<ref name=":4">[https://www.sciencedirect.com/science/article/abs/pii/S2211034812000971 Marrie] RA, Cutter GR, Tyry T. Substantial burden of dizziness in multiple sclerosis. Mult Scler Relat Disord. 2013;2(1):21-8.</ref> and it can mimic a peripheral vestibular disorder and cause vertigo | |||
* Vision dysfunctions<ref name=":0" /><ref name=":5">Armstrong D, Charlesworth E, Alderson AJ, Elliott DB. [https://onlinelibrary.wiley.com/doi/full/10.1111/opo.12299 Is there a link between dizziness and vision? A systematic review]. Ophthalmic Physiol Opt. 2016;36(4):477-86. </ref> | |||
** Any issues resulting in degradation of visual input can cause dizziness. These might occur in the eye (e.g. macular degeneration, cataracts), be related to the optic nerve, or be due to problems with visual processing | |||
* Psychogenic dizziness<ref name=":0" /> | |||
** It is not common to see purely psychogenic dizziness and vertigo. However, dizziness can trigger anxiety and anxiety can cause dizziness<ref name=":5" /> | |||
* [[Cervicogenic dizziness: screening|Cervicogenic dizziness]] | |||
** Dizziness associated with neck pain (a diagnosis of exclusion)<ref>Reiley AS, Vickory FM, Funderburg SE, Cesario RA, Clendaniel RA. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5759906/ How to diagnose cervicogenic dizziness]. Arch Physiother. 2017;7:12. </ref> | |||
** NB musculoskeletal structures of the cervical spine (e.g. golgi tendon organs, joint receptors, muscle spindles) cannot typically cause sensations of vertigo<ref name=":0" /> | |||
* Vestibular system disorders<ref name=":0" /><ref>VEDA. Types of vestibular disorders. Available from: https://vestibular.org/article/diagnosis-treatment/types-of-vestibular-disorders/ (accessed 14 May 2021).</ref> | |||
** Head trauma such as [[Whiplash Associated Disorders|whiplash]] or [[concussion]] | |||
** Vestibular system degeneration (age related) | |||
** Vestibular neuritis / labyrinthitis | |||
** BPPV | |||
** Endolymphatic hydrops (e.g. [[Ménière's disease|Meniere’s disease]]) | |||
** Ototoxicity, barotrauma, acoustic neuroma | |||
== Signs and Symptoms of Vestibular Disorders == | |||
* Nystagmus (involuntary eye movement) | |||
* Vertigo | |||
* Dizziness | |||
* Imbalance or ataxia | |||
* Compromised gaze stability (decreased visual acuity with head movement - i.e. the vestibular ocular reflex (VOR) is affected) | |||
== Anatomy of the Peripheral Vestibular System == | |||
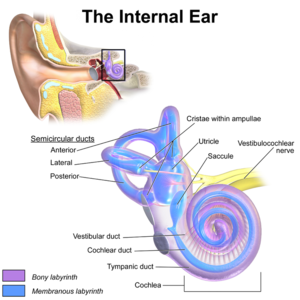
[[File:EarAnatomy InternalEar.png|thumb|Figure 1. Anatomy of the Inner Ear]] | |||
The outer ear consists of the external acoustic meatus. The tympanic membrane (i.e. eardrum) separates the outer ear from the middle ear. The inner ear contains the vestibular system and the cochlear.<ref name=":0" /> | |||
As is shown in figure 1, the vestibular apparatus consists of three semicircular canals, the utricle and the saccule (which together form the otoliths).<ref name=":3" /> | |||
The semicircular canals are specialised mechanoreceptors that enable us to access information about angular velocity.<ref name=":4" /> | |||
There are three canals: | |||
* Anterior | |||
* Posterior | |||
* Horizontal (or lateral) | |||
The anterior and posterior canals have a conjoint canal, called the common crus. | |||
The otoliths (i.e. utricle and saccule) are positioned in the central chamber known as the vestibule. They provide information about linear acceleration KNIEP. | |||
The cochlear is also positioned in the inner ear and it is responsible for hearing. | |||
== References == | == References == | ||
Revision as of 02:07, 14 May 2021
Introduction[edit | edit source]
Vestibular rehabilitation is an evidence-based approach to managing dizziness, vertigo, motion sensitivity, balance and postural control issues that occur due to vestibular dysfunction.[1]
Patients with vestibular impairment typically experience issues with gaze stability, motion stability, and balance and postural control. Vestibular rehabilitation, therefore, includes exercises that are focused towards these areas of pathology or dysfunction. However, the specific treatment approach will depend on the patient’s presentation.[1]
This page introduces vestibular dysfunction in general in order to provide background information and specific context for vestibular rehabilitation.
Epidemiology[edit | edit source]
Vestibular disturbance is a significant issue globally. It is estimated that 35.4 percent of North Americans aged over 40 have experienced some form of vestibular dysfunction. The likelihood of experiencing vestibular dysfunction increases with age.[2]
- 80 percent of people aged over 65 years experience dizziness - in 50 percent of cases this dizziness is caused by benign paroxysmal positional vertigo (BPPV)[2]
- 75 percent of adults aged over 70 years have a balance impairment (often associated with vestibular dysfunction and sensory loss in the feet)[3]
- Nearly 85 percent of adults aged over 80 years have vestibular dysfunction[3]
These numbers are significant as having vestibular dysfunction makes an individual eight times more likely to experience a fall[3] and falls are associated with significant morbidity, mortality[3] and economic cost.[4]
Moreover, the number of people experiencing vestibular dysfunction is expected to grow due to our ageing populations.[1]
Defining Dizziness and Vertigo[edit | edit source]
Dizziness and vertigo are not interchangeable terms.[1]
Dizziness is a non-specific term used to describe a variety of sensations such as light-headedness, swaying, disorientation and presyncope.[5]
Vertigo is a specific type of dizziness which is defined as the illusion of movement that occurs in the environment. Dizziness is not associated with this illusion of movement.[1]
Vertigo is caused by both peripheral and central vestibular diseases.[6] It is often rotational (i.e. the room spins around the patient), but there can also be linear disruptions or, less commonly, the patient might feel that his / her body is moving relative to the environment.[1]
Dizziness and vertigo are both purely subjective phenomena. There is no objective means of measuring them, so the patient’s subjective history is key.[1]
Causes of Dizziness[edit | edit source]
There are many causes of dizziness including:
- Cardiovascular dysfunction[1]
- Strokes are a rare cause of dizziness. The figures vary, but recent reports suggest strokes are the underlying cause of symptoms in around 3 to 5 percent of patients visiting emergency departments with dizziness and vertigo[7]
- Orthostatic hypotension
- Arrhythmias
- Neurological dysfunction[1]
- Dizziness is a common symptom associated with multiple sclerosis (MS)[8] and it can mimic a peripheral vestibular disorder and cause vertigo
- Vision dysfunctions[1][9]
- Any issues resulting in degradation of visual input can cause dizziness. These might occur in the eye (e.g. macular degeneration, cataracts), be related to the optic nerve, or be due to problems with visual processing
- Psychogenic dizziness[1]
- It is not common to see purely psychogenic dizziness and vertigo. However, dizziness can trigger anxiety and anxiety can cause dizziness[9]
- Cervicogenic dizziness
- Vestibular system disorders[1][11]
- Head trauma such as whiplash or concussion
- Vestibular system degeneration (age related)
- Vestibular neuritis / labyrinthitis
- BPPV
- Endolymphatic hydrops (e.g. Meniere’s disease)
- Ototoxicity, barotrauma, acoustic neuroma
Signs and Symptoms of Vestibular Disorders[edit | edit source]
- Nystagmus (involuntary eye movement)
- Vertigo
- Dizziness
- Imbalance or ataxia
- Compromised gaze stability (decreased visual acuity with head movement - i.e. the vestibular ocular reflex (VOR) is affected)
Anatomy of the Peripheral Vestibular System[edit | edit source]
The outer ear consists of the external acoustic meatus. The tympanic membrane (i.e. eardrum) separates the outer ear from the middle ear. The inner ear contains the vestibular system and the cochlear.[1]
As is shown in figure 1, the vestibular apparatus consists of three semicircular canals, the utricle and the saccule (which together form the otoliths).[7]
The semicircular canals are specialised mechanoreceptors that enable us to access information about angular velocity.[8]
There are three canals:
- Anterior
- Posterior
- Horizontal (or lateral)
The anterior and posterior canals have a conjoint canal, called the common crus.
The otoliths (i.e. utricle and saccule) are positioned in the central chamber known as the vestibule. They provide information about linear acceleration KNIEP.
The cochlear is also positioned in the inner ear and it is responsible for hearing.
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 Tonks B. Introduction to Vestibular Rehabilitation Course. Physioplus. 2021.
- ↑ 2.0 2.1 Agrawal Y, Carey JP, Della Santina CC, Schubert MC, Minor LB. Disorders of balance and vestibular function in US adults: data from the National Health and Nutrition Examination Survey, 2001-2004. Arch Intern Med. 2009;169(10):938-44.
- ↑ 3.0 3.1 3.2 3.3 Hall CD, Herdman SJ, Whitney SL, Cass SP, Clendaniel RA, Fife TD et al. Vestibular rehabilitation for peripheral vestibular hypofunction: An evidence-based clinical practice guideline: FROM THE AMERICAN PHYSICAL THERAPY ASSOCIATION NEUROLOGY SECTION. J Neurol Phys Ther. 2016;40(2):124-55.
- ↑ Haddad YK, Bergen G, Florence CS. Estimating the economic burden related to older adult falls by state. J Public Health Manag Pract. 2019;25(2):E17-E24.
- ↑ Kerber KA, Brown DL, Lisabeth LD, Smith MA, Morgenstern LB. Stroke among patients with dizziness, vertigo, and imbalance in the emergency department: a population-based study. Stroke. 2006;37(10):2484-2487.
- ↑ Kovacs E, Wang X, Grill E. Economic burden of vertigo: a systematic review. Health Econ Rev. 2019;9(1):37.
- ↑ 7.0 7.1 Saber Tehrani AS, Kattah JC, Kerber KA, Gold DR, Zee DS, Urrutia VC et al. Diagnosing stroke in acute dizziness and vertigo: pitfalls and pearls. Stroke. 2018;49(3):788-795.
- ↑ 8.0 8.1 Marrie RA, Cutter GR, Tyry T. Substantial burden of dizziness in multiple sclerosis. Mult Scler Relat Disord. 2013;2(1):21-8.
- ↑ 9.0 9.1 Armstrong D, Charlesworth E, Alderson AJ, Elliott DB. Is there a link between dizziness and vision? A systematic review. Ophthalmic Physiol Opt. 2016;36(4):477-86.
- ↑ Reiley AS, Vickory FM, Funderburg SE, Cesario RA, Clendaniel RA. How to diagnose cervicogenic dizziness. Arch Physiother. 2017;7:12.
- ↑ VEDA. Types of vestibular disorders. Available from: https://vestibular.org/article/diagnosis-treatment/types-of-vestibular-disorders/ (accessed 14 May 2021).