Infantile Brachial Plexus Injury: Difference between revisions
No edit summary |
No edit summary |
||
| Line 32: | Line 32: | ||
== Classification == | == Classification == | ||
There are several ways to classify NBPP. One classification system is based on which portion of the [[brachial plexus]] is injured. The "upper trunk" refers to nerves C5-C6 and is referred to as Duchenne-Erb syndrome. The lower trunk affects nerves C7-T1 and know as Dejerine-Klumpke syndrome. If there is a complete severing of the brachial plexus, then all nerve roots between C5-T1 would be disturbed.<ref name=":2" />[[File:Seddon's - Classification of Nerve Injuries - Wikimedia Commons.jpg|thumb|450x450px|Classification of Nerve Injuries]]Another classification system is based on the degree of lesion of the nerve. For example: | There are several ways to classify NBPP. One classification system is based on which portion of the [[brachial plexus]] is injured. The "upper trunk" refers to nerves C5-C6 and is referred to as Duchenne-Erb syndrome. The lower trunk affects nerves C7-T1 and know as Klumpke paralysis (or Klumpke palsy / Dejerine-Klumpke syndrome). If there is a complete severing of the brachial plexus, then all nerve roots between C5-T1 would be disturbed - individuals with a global plexus injury may also present with [[Horner's Syndrome|Horner's syndrome]].<ref name=":2" />[[File:Seddon's - Classification of Nerve Injuries - Wikimedia Commons.jpg|thumb|450x450px|Classification of Nerve Injuries]]Another classification system is based on the degree of lesion of the nerve. For example: | ||
* neurotmesis: complete tear of the [[Axons|axon]] and connective tissue with no chance of recovery | * neurotmesis: complete tear of the [[Axons|axon]] and connective tissue with no chance of recovery | ||
| Line 125: | Line 125: | ||
== Surgery == | == Surgery == | ||
Children are considered suitable candidates for surgery if conservative management has failed.<ref name=":6" /> Surgery for children aged less than 12 months is controversial - an infant must be significantly impacted to consider early surgery (e.g. they should have had no anti-gravity muscle control for at least three to nine months).<ref name=":6" /> | Children are considered suitable candidates for surgery if conservative management has failed.<ref name=":6" /> Surgery for children aged less than 12 months is controversial - an infant must be significantly impacted to consider early surgery (e.g. they should have had no anti-gravity muscle control for at least three to nine months).<ref name=":6" /> However, Meena et al. note that infants with Horner's syndrome should have surgery within 2-3 months of birth.<ref name=":3" /> | ||
There are two types of surgery for NBPP: primary and secondary.<ref name=":3" /> | There are two types of surgery for NBPP: primary and secondary.<ref name=":3" /> | ||
Revision as of 11:17, 9 May 2023
Top Contributors - Robin Tacchetti, Jess Bell and Kim Jackson
Introduction[edit | edit source]
Neonatal brachial plexus palsy (NBPP) is a closed nerve traction injury of the brachial plexus (C5-T1). It predominately occurs during labour and it can limit arm function.[1] [2] [3] NBPP causes flaccid paralysis or weakness in the upper extremity and is diagnosed soon after birth. The global incidence of NBPP is reported to be between 1-4 cases per 1000 live births with rates varying depending on study setting and availability of foetal and maternal care.[4] The overall incidence of NBPP is decreasing.[2]
Mechanism of Injury[edit | edit source]
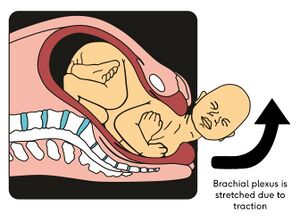
In neonatal brachial plexus injury, obstetric, maternal and infant factors cause traction to be applied to the brachial plexus.[2] The most common cause of NBPP is shoulder dystocia - i.e. the "delivery of the anterior shoulder of the baby is hampered by mother’s pubic symphysis".[5] This traction force widens the angle between the baby's shoulder and neck, resulting in an overstretched ipsilateral brachial plexus.[5]
Many infants spontaneously recover or gain close to normal upper extremity function. For those whose motor recovery is incomplete, close monitoring and expert interventions are essential to optimising outcomes.[4] Prognosis depends on the level of nerve root involvement and the severity of injury.[3] Within the first year of life, 80-96% of individuals with NBPP will recover completely.[5]
Risk factors[edit | edit source]
The risk factors for NBPP include neonatal, maternal and labour-related issues.
1. Neonatal
- Large birth weight
- Breech presentation (caesarean section may be a protective factor)[2]
- Congenital anomalies
2. Maternal
- Age > 35 years
- Cephalopelvic disproportion
- Obesity
- Gestational diabetes mellitus (macrosomia - i.e. babies who are large for their gestational age[6])
- Previous child with NBPP
3. Labour-related factors
- Shoulder dystocia
- Increased duration of second stage of labour (>60 minutes)
- Operative vaginal deliveries
- Vacuum extraction
- Direct compression of the foetal neck during delivery by forceps[5][2][4]
Classification[edit | edit source]
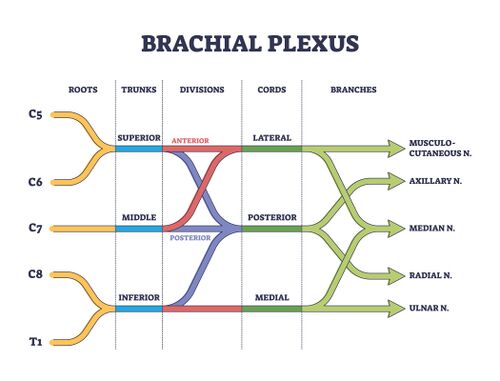
There are several ways to classify NBPP. One classification system is based on which portion of the brachial plexus is injured. The "upper trunk" refers to nerves C5-C6 and is referred to as Duchenne-Erb syndrome. The lower trunk affects nerves C7-T1 and know as Klumpke paralysis (or Klumpke palsy / Dejerine-Klumpke syndrome). If there is a complete severing of the brachial plexus, then all nerve roots between C5-T1 would be disturbed - individuals with a global plexus injury may also present with Horner's syndrome.[3]
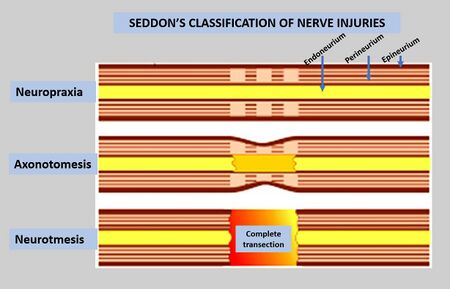
Another classification system is based on the degree of lesion of the nerve. For example:
- neurotmesis: complete tear of the axon and connective tissue with no chance of recovery
- axonotmesis: axon interruption with no, or only partial, interruption to myelin and connective tissue with gradual recovery
- neuropraxic: transient physiological blockage with spontaneous recovery; no nerve rupture with full recovery
- neuroma: blocking of nerve impulse to muscle by injured nerve scar tissue[3][5]
Mallet Classification[edit | edit source]
The Mallet classification system is an assessment tool used with children who have brachial plexus birth injuries. The examination assesses the performance of six upper extremity functional movements. Administrators score the test based on observation of the movement on a scale from V (full function) to I (no function). This test is easy to administer in a clinical setting and has been found to have good internal consistency, inter-observer reliability and intra-observer reliability.[7]
Clinical Presentation[edit | edit source]
Infantile brachial plexus injury is generally detected by parents or healthcare workers in the immediate neonatal period - they generally observe an absence of motor function in the arm or hand.[3] These motor deficits should be painless. If there is pain during passive range of motion, a fracture should be suspected.[4]
The table below highlights common presentations based on which nerve root is injured.
| Segment Involved | Muscular Deficits | Arm Position |
|---|---|---|
| C5 - deltoid | Abduction of shoulder | Adducted |
| C5 - supra and infraspinatus | External rotation of shoulder | Internally rotated |
| C5 C6 - bracioradialis | Flexion of elbow | Extended |
| C5 C6 - supinators | Supination of forearm | Pronated |
| C6 C7 - extensors of wrist | Wrist extensors | Flexed |
| C6 C7 - extensors of fingers | Finger extensors | Flexed |
NBPP may occur with other conditions, including:
- humeral and clavicular fractures
- flexion contracture of the elbow
- progressive glenohumeral dysplasia
- torticollis[4]
Assessment[edit | edit source]
The assessment of an individual with infantile brachial plexus injury should include the following:[1][8]
- detailed maternal and delivery history
- musculoskeletal examination
- observation
- check posture
- palpation
- muscle activation / strength
- active and passive range of motion
- check for age-appropriate activities of daily living (e.g. holding a toy / bottle, reaching for feet)
- neurological examination
- reflex testing and righting reactions: (if the entire brachial plexus is impacted, the Moro reflex, asymmetrical tonic neck reflex and grasp reflex will not be present[8])
- sensory examination
- wrinkle test can be used
- serial EMGs may be performed (starting at 2 weeks, and repeated in 6-8 week intervals)
- functional assessment
- respiratory status
- symmetry of chest movements
- determine if there is a need for an x-ray to rule out bony injury
- check for secondary impairments (e.g. soft tissue contractures, scapula winging)
Rehabilitation[edit | edit source]
Conservative treatment is always initiated as early as possible. Treatment will depend on each child's presentation and their specific impairments. Conservative treatment for infantile brachial plexus injury could include the following interventions:[3][8]
- active movement of the upper extremity
- stretches and passive range of motion
- support of upper limb for activities in sitting, prone, or when reaching, grasping (e.g. kinesiotaping, table for support); provide proximal support to help ensure success during activities (e.g. use a semi-reclined, supported chair)
- sensory stimulation
- tactile stimulation with varying textures
- brushing and vibration techniques
- bimanual activities
- electrical stimulation to increase muscle strength and inhibit atrophy (may be better to wait until at least 18 months of age when much of the nerve regeneration has already occurred[8])
- botulinum toxin injections into healthy antagonist muscles
- splints for infants with impaired wrist function to facilitate increased hand function - other adaptive equipment like kinesiotaping, de-rotation straps may also be used
- constraint induced movement therapy
Ideally, therapy would occur several times a week, and a home programme should be prescribed to achieve the best outcome.[3]
Surgery[edit | edit source]
Children are considered suitable candidates for surgery if conservative management has failed.[8] Surgery for children aged less than 12 months is controversial - an infant must be significantly impacted to consider early surgery (e.g. they should have had no anti-gravity muscle control for at least three to nine months).[8] However, Meena et al. note that infants with Horner's syndrome should have surgery within 2-3 months of birth.[5]
There are two types of surgery for NBPP: primary and secondary.[5]
- Primary reconstruction: for children who do not have spontaneous recovery. This type of surgical management may include nerve grafting, nerve transfers, direct repair and/or soft tissue procedures.
- Secondary reconstruction: recommended for children who have had some spontaneous recovery but continue to have significant functional deficit or children who have undergone a primary surgery but continue to have limitations in limb function. Secondary surgery may include osseous procedures and soft tissue reconstructions.[5]
Post-surgical management: the infant is placed in a prefabricated cast to limit movement of the neck and affected arm for 1-2 weeks. After 2-3 weeks, gentle range of motion can be initiated. Regular follow-up by a rehabilitation team for a minimum of 5 years is recommended for assessment of recovery and to identify if any secondary reconstructions may be needed to improve function.[5]
** Due to the rate of nerve regeneration (i.e. 1 mm/day or 1 inch/month), clinical changes may not be evident for 1-2 years after surgery. Regular physiotherapy should be provided while waiting for reinnervation to prevent contractures.[5]
Resources[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 Shah V, Coroneos CJ, Ng E. The evaluation and management of neonatal brachial plexus palsy. Paediatrics & Child Health. 2021 Dec;26(8):493-7.
- ↑ 2.0 2.1 2.2 2.3 2.4 Van der Looven R, Le Roy L, Tanghe E, Samijn B, Roets E, Pauwels N, Deschepper E, De Muynck M, Vingerhoets G, Van den Broeck C. Risk factors for neonatal brachial plexus palsy: a systematic review and meta‐analysis. Developmental Medicine & Child Neurology. 2020 Jun;62(6):673-83.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 Frade F, Gómez-Salgado J, Jacobsohn L, Florindo-Silva F. Rehabilitation of neonatal brachial plexus palsy: integrative literature review. Journal of clinical medicine. 2019 Jul 5;8(7):980.
- ↑ 4.0 4.1 4.2 4.3 4.4 Heyworth BE, Fabricant PD. BRACHIAL PLEXUS BIRTH PALSY. Rockwood and Matsen's The Shoulder E-Book. 2021 Jun 12:39.
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 Meena R, Doddamani RS, Sawarkar DP, Agrawal D. Current Management Strategies in Neonatal Brachial Plexus Palsy. Journal of Peripheral Nerve Surgery Vol. 2021;5(1).
- ↑ Akanmode AM, Mahdy H. Macrosomia. [Updated 2022 Sep 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557577/
- ↑ Russo SA, Topley MT, Richardson RT, Richards JG, Chafetz RS, van Roden EA, Zlotolow DA, Mulcahey MJ, Kozin SH. Assessment of the relationship between Brachial Plexus Profile activity short form scores and modified Mallet scores. Journal of Hand Therapy. 2022 Jan 1;35(1):51-7.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 Eskay K. Infantile Brachial Plexus Injury Course. Plus, 2023.