Hypokalemia
Original Editors - Kara Lawless from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Kara Lawless, Elaine Lonnemann, Lucinda hampton, Admin, Kim Jackson, Wendy Walker and WikiSysop
Definition/Description[edit | edit source]
One of the most common electrolyte disturbances seen in clinical practice is hypokalemia. Hypokalemia is known as a electrolyte imbalance that is lower than normal level of potassium in your bloodstream.[1]
- A normal blood potassium is 3.6 to 5.2 mmol/L.
- Severe and life threatening hypokalemia level is known as <2.5mmol/L. [2]
Potassium helps control how our muscles, heart, and digestive system work. Hypokalemia occurs when your body loses too much potassium or does not absorb enough from food[3].
Etiology[edit | edit source]
Hypokalemia has many causes. The most common cause is excessive potassium loss in urine due to prescription medications that increase urination. Vomiting, diarrhea or both also can result in excessive potassium loss from the digestive tract. Occasionally, low potassium is caused by not getting enough potassium in the diet.
Causes of potassium loss include:
- Alcohol use (excessive)
- Chronic kidney disease
- Diabetic ketoacidosis
- Diarrhea
- Diuretics
- Excessive laxative use
- Excessive sweating
- Folic acid deficiency
- Primary aldosteronism
- Some antibiotic use
- Vomiting
Epidemiology[edit | edit source]
In general, hypokalemia is associated with diagnoses of cardiac disease, renal failure, malnutrition, and shock. Hypothermia and increased blood cell production (for example, leukemia) are additional risk factors for developing hypokalemia[1].
- Hypokalemia is more common in hospitalized patients, up to 15%, as a result of other pathologies.
- Only 3% of the outpatient population is found to have Hypokalemia.
- There has been no significant difference in prevalence between gender and race. [4]
Characteristics/Clinical[edit | edit source]
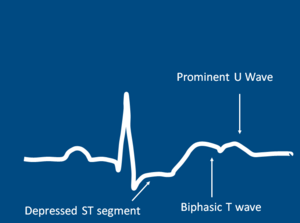
Image 1: ECG Pattern Of Hypokalemia
In most cases, low potassium is found by a blood test that is done because of an illness, or because of diuretics use. It is rare for low potassium to cause isolated symptoms eg muscle cramps if person is feeling well in other respects.
Hypokalemia symptoms may include:
- Weakness
- Fatigue
- Muscle cramps
- Constipation
Abnormal heart rhythms (arrhythmias) are the most worrisome complication of very low potassium levels, particularly in people with underlying heart disease[5].
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
Hypokalemia is commonly found in a blood test, with <3.5mmol/L as mild hypokalemia and <2.5mmol/L as severe hypokalmia.[2]
In severe cases, a 12-lead electrocardiogram may be necessary if to check for cardiac arrythymias. Findings such as T-wave flattening or prominent U waves will result in hospital admission.[4] Other tests may include:
- arterial blood gas
- basic or comprehensive metabolic panel
Blood tests will also be administered to check the following:
- glucose
- magnesium
- calcium
- sodium
- phosphorus
- thyroxine
- aldosterone levels.[6]
Management[edit | edit source]
The overarching goals of therapy for hypokalemia are to prevent or treat life-threatening complications, replace the potassium deficit, and to diagnose and correct the underlying cause.[1]
Management of the underlying disease or contributing factors constitutes the cornerstone of therapeutic approach. Potassium should be gradually replaced, preferably by oral administration if clinically feasible. In cases of severe/symptomatic hypokalemia and cardiac complications, i.v. administration with continuous ECG monitoring is recommended. In some patients, such as in endocrine related hypokalemia cases, multidisciplinary diagnostic and therapeutic approach is needed.[7]
The majority of patients who are treated for hypokalemia have a good outcome but those who remain untreated are at a risk for arrhythmias which may be fatal.[6]
Physical Therapy Management[edit | edit source]
Hypokalemia is not managed primarily by a physical therapist. Physical therapists should be mindful of common signs of symptoms of hypokalemia when working with patients.
- Potassium levels < 3.2 mEq/L is contraindicated for physical therapy intervention due to the potential for arrhythmia . Due to muscle weakness and cramping, exercise is not effective during the state of hypokalemia.
- Patients should be monitored for potassium levels in order to determine the appropriate time to participate in Physical Therapy.[8]
Differential Diagnosis[edit | edit source]
- Bartter syndrome
- Hyperthyroidism and thyrotoxicosis
- Hypocalcemia
- Hypochloremic alkalosis
- Hypomagnesemia
- Iatrogenic Cushing syndrome
- Metabolic alkalosis
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Castro D, Sharma S. Hypokalemia. 2018 Available: https://www.ncbi.nlm.nih.gov/books/NBK482465/(accessed 18.9.2021)
- ↑ 2.0 2.1 Low Potassium(hypokalemia)[Internet]. 2012 August 10 [cited 2013 March 27] Available from:http://www.mayoclinic.com/health/low-potassium/MY00760
- ↑ Drugs.com Hypokalemia Avaulable: https://www.drugs.com/cg/hypokalemia.html(accessed 18.9.2021)
- ↑ 4.0 4.1 Hypokalemia [Internet]. 2012 [cited 2013 March 27] Available from:https://www.clinicalkey.com/topics/nephrology/hypokalemia.html#720089
- ↑ Mayo Clinic Hypokalemia Available: https://www.mayoclinic.org/symptoms/low-potassium/basics/when-to-see-doctor/sym-20050632 (accessed 19.9.2021)
- ↑ 6.0 6.1 Hypokalemia [Internet]. 2013 March 22 [cited 2013 March 27] Available from: http://www.nlm.nih.gov/medlineplus/ency/article/000479.htm
- ↑ Kardalas E, Paschou SA, Anagnostis P, Muscogiuri G, Siasos G, Vryonidou A. Hypokalemia: a clinical update. Endocrine connections. 2018 Apr 1;7(4):R135-46. Available:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5881435/ (accessed 18.9.2021)
- ↑ Goodman CC. Fuller KS. In K Falk editor. Pathology: Implications for the Physical Therapist. St. Louis: Saunders Elsevier; 2009. pp.150, 157, 187-189, 480, 558, 927, 1243, 1640-1641
see adding references tutorial.