Gluteus Medius: Difference between revisions
No edit summary |
No edit summary |
||
| Line 45: | Line 45: | ||
As mentioned by Vladmir Janda, Gluteus Medius is one of the phasic muscles that tends to be inhibited in our body by many causes. For example: | As mentioned by Vladmir Janda, Gluteus Medius is one of the phasic muscles that tends to be inhibited in our body by many causes. For example: | ||
# Standing for a prolong period of time with more body weight shifted on any one lower limb with the pelvis swayed sideways and hip joint adducted.<ref name=":2" /> | # Standing for a prolong period of time with more body weight shifted on any one lower limb with the pelvis swayed sideways and hip joint adducted.<ref name=":2" /> | ||
# Sleeping in a side lying position with no pillow in between two lower extremities will lead to | # Sleeping in a side lying position with no pillow in between two lower extremities will lead to top leg flexion and adduction of the upper leg over the bottom leg.<ref name=":2" /> | ||
# Sitting with crossed legs for a long period of time will potentially weaken the hip abductor muscles | # Sitting with crossed legs for a long period of time will potentially weaken the hip abductor muscles as this position will elongate the gluteus medius muscle beyond resting physiological length. | ||
# Tight hip adductors which | # Tight hip adductors which leads to reciprocal inhibition to Gluteus medius. | ||
* When Gluteus Medius is inhibited, the body must compensate by relying on other muscles to maintain frontal plane stability and prevent the pelvis from dropping. As a result, the activity of the ipsilateral tensor fascia latae and contralateral quadratus lumborum will increase, leading these muscles to become tight and overactive.<ref>Kim H.J , Lee H.S, Jung H.G . [http://www.jkspm.org/journal/view.html?doi=10.13066/kspm.2017.12.3.59 Difference of Muscle Activity by Pelvic Tilt in Side-Lying Hip Abduction] .Journal of The Korean Society of Physical Medicine. 2017:12(3): 59-66 .</ref> Janda mentioned that quadratus lumborum and tensor fascia latae are tonic muscles that tend to be tight and overactive. | * When Gluteus Medius is inhibited, the body must compensate by relying on other muscles to maintain frontal plane stability and prevent the pelvis from dropping. As a result, the activity of the ipsilateral tensor fascia latae and contralateral quadratus lumborum will increase, leading these muscles to become tight and overactive.<ref>Kim H.J , Lee H.S, Jung H.G . [http://www.jkspm.org/journal/view.html?doi=10.13066/kspm.2017.12.3.59 Difference of Muscle Activity by Pelvic Tilt in Side-Lying Hip Abduction] .Journal of The Korean Society of Physical Medicine. 2017:12(3): 59-66 .</ref> Janda mentioned that quadratus lumborum and tensor fascia latae are tonic muscles that tend to be tight and overactive. | ||
* Weakness in this muscle has been associated with lower-limb musculoskeletal pathology<ref>Barton CJ, Lack S, Malliaras P, Morrissey D. [https://bjsm.bmj.com/content/47/4/207 Gluteal muscle activity and patellofemoral pain syndrome: a systematic review.] British journal of sports medicine. 2012 Sep 3:bjsports-2012.</ref> and gait disturbance following stroke.<ref>Buurke JH, Nene AV, Kwakkel G, Erren-Wolters V, IJzerman MJ, Hermens HJ. [https://journals.sagepub.com/doi/abs/10.1177/1545968308317972 Recovery of gait after stroke: what changes?. Neurorehabilitation and Neural Repair]. 2008 Nov 1;22(6):676-83.</ref> | * Weakness in this muscle has been associated with lower-limb musculoskeletal pathology<ref>Barton CJ, Lack S, Malliaras P, Morrissey D. [https://bjsm.bmj.com/content/47/4/207 Gluteal muscle activity and patellofemoral pain syndrome: a systematic review.] British journal of sports medicine. 2012 Sep 3:bjsports-2012.</ref> and gait disturbance following stroke. Following stroke, the patient presents with [[Gait Deviations|hemiplegic gait]]<ref>Buurke JH, Nene AV, Kwakkel G, Erren-Wolters V, IJzerman MJ, Hermens HJ. [https://journals.sagepub.com/doi/abs/10.1177/1545968308317972 Recovery of gait after stroke: what changes?. Neurorehabilitation and Neural Repair]. 2008 Nov 1;22(6):676-83.</ref> | ||
* There is a relationship between a weak or dysfunctional GM and many lower extremity injuries such as: [https://www.physio-pedia.com/Trendelenburg_Gait Trendelenburg gait][[Iliotibial Band Syndrome|, Illio-tibial band (ITB) syndrome]], [[Patellofemoral Pain Syndrome|Patellofemoral pain syndrome (PFPS)]], [https://www.physio-pedia.com/Anterior_Cruciate_Ligament_(ACL)_Injury Anterior cruciate ligament (ACL)] and other knee and ankle injuries. <ref name=":2" /> | * There is a relationship between a weak or dysfunctional GM and many lower extremity injuries such as: [https://www.physio-pedia.com/Trendelenburg_Gait Trendelenburg gait][[Iliotibial Band Syndrome|, Illio-tibial band (ITB) syndrome]], [[Patellofemoral Pain Syndrome|Patellofemoral pain syndrome (PFPS)]], [https://www.physio-pedia.com/Anterior_Cruciate_Ligament_(ACL)_Injury Anterior cruciate ligament (ACL)] and other knee and ankle injuries. <ref name=":2" /> | ||
* The [[Trendelenburg Gait|Trendelenburg sign]] occurs when the gluteus medius muscle is unable to function efficiently due to factors such as pain, poor mechanics, or weakness. In such cases, the pelvis will drop on the side opposite to the weakness. Trunk compensation is often observed with a Trendelenburg gait.<ref name="pala" /> An impressive research study on the validity of the Trendelenburg sign revealed that the test should not be applied to healthy individuals with gluteus medius strength exceeding 30% of body weight. It is most effective for assessing marked weakness in patients, highlighting the possibility of an inhibited gluteus medius even when the Trendelenburg sign appears negative.<ref>KendallK. D., Patel C., Wiley J. P., Pohl M. B., Emery C. A., etal [https://insights.ovid.com/pubmed?pmid=22797529 .''Steps Toward the Validation of the Trendelenburg Test.''] ''Clinical Journal of Sport Medicine.jan 2013: 23(1): 45–51.''</ref> | * The [[Trendelenburg Gait|Trendelenburg sign]] occurs when the gluteus medius muscle is unable to function efficiently due to factors such as pain, poor mechanics, or weakness. In such cases, the pelvis will drop on the side opposite to the weakness. Trunk compensation is often observed with a Trendelenburg gait.<ref name="pala" /> An impressive research study on the validity of the Trendelenburg sign revealed that the test should not be applied to healthy individuals with gluteus medius strength exceeding 30% of body weight. It is most effective for assessing marked weakness in patients, highlighting the possibility of an inhibited gluteus medius even when the Trendelenburg sign appears negative.<ref>KendallK. D., Patel C., Wiley J. P., Pohl M. B., Emery C. A., etal [https://insights.ovid.com/pubmed?pmid=22797529 .''Steps Toward the Validation of the Trendelenburg Test.''] ''Clinical Journal of Sport Medicine.jan 2013: 23(1): 45–51.''</ref> | ||
Revision as of 07:55, 8 January 2024
Original Editor - Alex Palmer,
Top Contributors - Alex Palmer, George Prudden, Kim Jackson, Ahmed Nasr, Joao Costa, Joanne Garvey, Candace Goh, Nupur Smit Shah, WikiSysop, Rachael Lowe, Evan Thomas, Kai A. Sigel, Vidya Acharya and Pinar Kisacik;
Description[edit | edit source]
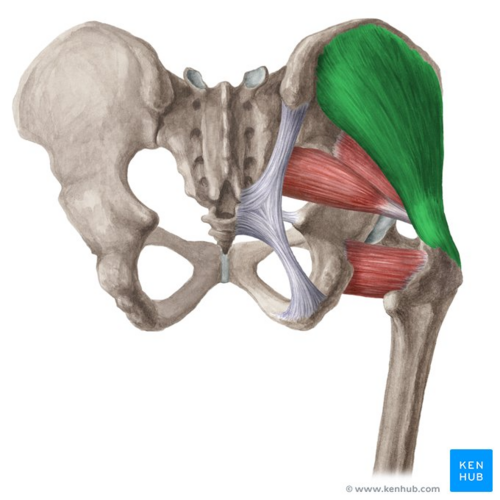
Gluteus medius is located on the lateral aspect of the upper buttock, below the iliac crest. The superior muscle is broad with the muscle narrowing towards its insertional tendon giving it a fan-shape. Gluteus maximus covers all of the gluteal muscles except for the antero-superior third of the Gluteus medius. This uncovered part of Gluteus medius is the safe area at which we should apply buttocks dorso gluteal intramuscular injections.
Image: Gluteus medius muscle (highlighted in green) - posterior view[1]
This 2 minute video is a good summary of the gluteus medius muscle.[2]
Origin[edit | edit source]
The gluteus medius muscle has its upper attachment on the gluteal, or lateral surface of the ilium between the posterior and anterior gluteal lines and gluteal aponorosis . This is a large area, reaching from the iliac crest above to the almost the sciatic notch below. The muscle adheres firmly to a strong layer of fascia, which it shares with the gluteus maximus at the posterior end.[3][4]
Insertion[edit | edit source]
The muscle fibres of the gluteus medius take distinct courses based on their position:[3]
- The fibres of the posterior portion pass forwards and downwards.
- The fibres of the middle portion pass downwards.
- The fibres of the anterior portion pass backwards and downward.
All fibres combine to form a flattened tendon which attaches to the posterior and lateral part of the superior portion of the greater trochanter of the femur. It attaches specifically to a rough area that runs downwards and forwards on the superolateral aspect of the greater trochanter. Separating the tendon and the trochanter is the trochanteric bursa of the gluteus medius.
Nerve Supply[edit | edit source]
The gluteus medius is supplied by the superior gluteal nerve (root L4, L5 and S1). Cutaneous supply is mainly provided by L1 and L2.[3][4]
Function[edit | edit source]
- Gluteus medius is the prime mover of abduction at hip joint.
- Anterior portion of Gluteus medius abduct, assist in flexion and medial rotation of the hip.[5]
- Posterior portion of Gluteus medius abduct, assist in extension and lateral rotation of the hip.
- In hip flexion all portions internally rotate the hip and it has shown that at 90 degree of hip flexion the leverage of medial rotation of Gluteus medius is increased eight folds.[3][5]
- All portions of the Gluteus medius will produce hip abduction regardless of the position of the hip. [3]
- The Gluteus medius plays a crucial role in upholding the stability of the pelvis in the frontal plane. It collaborates with the ipsilateral tensor fascia lata and contralateral quadratus lumborum, to create a lateral fascial sling. The primary function of this sling is to ensure stability in the frontal plane.
- Gluteus medius is an important muscle in walking, running, and single-leg weight-bearing because it prevents the opposite side of the pelvis from dropping during these activities. When a limb is taken off the ground, the pelvis on that side will tend to drop through a loss of support from below. Gluteus medius works to maintain the side of the pelvis that drops, therefore allowing the other limb to swing forward for the next step.[3][6]
- Gluteus medius also supports the pelvis during gait by producing hip rotation with assistance from gluteus minimus and tensor fascia lata. Conversely, the hip is supported during the stance phase by acting on the same side.
Inhibition of Gluteus Medius[edit | edit source]
As mentioned by Vladmir Janda, Gluteus Medius is one of the phasic muscles that tends to be inhibited in our body by many causes. For example:
- Standing for a prolong period of time with more body weight shifted on any one lower limb with the pelvis swayed sideways and hip joint adducted.[6]
- Sleeping in a side lying position with no pillow in between two lower extremities will lead to top leg flexion and adduction of the upper leg over the bottom leg.[6]
- Sitting with crossed legs for a long period of time will potentially weaken the hip abductor muscles as this position will elongate the gluteus medius muscle beyond resting physiological length.
- Tight hip adductors which leads to reciprocal inhibition to Gluteus medius.
- When Gluteus Medius is inhibited, the body must compensate by relying on other muscles to maintain frontal plane stability and prevent the pelvis from dropping. As a result, the activity of the ipsilateral tensor fascia latae and contralateral quadratus lumborum will increase, leading these muscles to become tight and overactive.[7] Janda mentioned that quadratus lumborum and tensor fascia latae are tonic muscles that tend to be tight and overactive.
- Weakness in this muscle has been associated with lower-limb musculoskeletal pathology[8] and gait disturbance following stroke. Following stroke, the patient presents with hemiplegic gait[9]
- There is a relationship between a weak or dysfunctional GM and many lower extremity injuries such as: Trendelenburg gait, Illio-tibial band (ITB) syndrome, Patellofemoral pain syndrome (PFPS), Anterior cruciate ligament (ACL) and other knee and ankle injuries. [6]
- The Trendelenburg sign occurs when the gluteus medius muscle is unable to function efficiently due to factors such as pain, poor mechanics, or weakness. In such cases, the pelvis will drop on the side opposite to the weakness. Trunk compensation is often observed with a Trendelenburg gait.[3] An impressive research study on the validity of the Trendelenburg sign revealed that the test should not be applied to healthy individuals with gluteus medius strength exceeding 30% of body weight. It is most effective for assessing marked weakness in patients, highlighting the possibility of an inhibited gluteus medius even when the Trendelenburg sign appears negative.[10]
Activation of Gluteus medius[edit | edit source]
There are many exercises that help in activation of Glutes medius each exercise activate Glutes medius by a certain percentage as shown by EMG activity. We divide them as following[5]:
| Level of Gluteus medius activation | Types of exercises |
|---|---|
| Moderate-level activation (21–40% MVIC) |
|
| High-level activation (41–60% MVIC) |
|
| Very high-level activation (>60% MVIC) |
|
- MVIC = maximum voluntary isometric contraction The prone bridge/plank are unique from the other exercises because of it's static nature to maintain a neutral hip and spine position during this exercise so it focuses on Gluteus Medius’s role as a hip and spine stabiliser.
Assessment[edit | edit source]
Palpation[edit | edit source]
Find the middle of iliac crest which is located above the greater trochanter and two fingers below is the bulk of gluteus medius. The contraction of the muscle can be felt by alternate single leg-stands.[3]
Power[edit | edit source]
- Hip abduction in side-lying
- Double or single-leg stance test
- Adding an upper body movement to the single-leg stance test
- Assessment of functional tasks that require single-leg stance such as step-downs, walking or running.[6]
Length[edit | edit source]
Treatment[edit | edit source]
First, you have to find the causes for inhibition or weakness of the Gluteus medius and try to prevent it and then try to activate Gluteus medius.
Pressman and colleagues describe a progressive program for strengthening gluteus medius weakness.[6]
- Non weight-bearing and basic weight-bearing exercises such as clam shell exercises, side lying hip abduction, standing hip abduction, and basic single leg balance exercises. Progress when the patient can hold their pelvis level during single leg stance for 30 seconds. Progression can vary as per the strength of the patient.
- Weight-bearing exercises and gradually progresses stability exercises by (i) translating the center of gravity horizontally via stepping and/or hopping exercises; (ii) reducing the width of the base of support, (iii) increasing the height of the center of gravity by elevating the arms and/or hand-held weights, or (iii) performing the exercises on unstable surfaces.
- Sport-specific movement patterns.
Resources[edit | edit source]
Related Pages[edit | edit source]
- Anatomy Slings and Their Relationship to Low Back Pain
- Gluteus maximus
- Greater trochanteric pain syndrone
- Trendelenburg gait
- Trendelenburg sign
- Ober's test
- Trochanteric bursitis
References[edit | edit source]
- ↑ Gluteus medius muscle (highlighted in green) - posterior view image - © Kenhub https://www.kenhub.com/en/library/anatomy/gluteus-medius-and-minimus-muscles
- ↑ Gluteus medius muscle video - © Kenhub https://www.kenhub.com/en/library/anatomy/gluteus-medius-and-minimus-muscles
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 Palastanga N, Soames R. Anatomy and Human Movement: Structure and Function. 6th ed. London, United Kingdom: Churchill Livingstone; 2012.
- ↑ 4.0 4.1 Kendall F.B , McCreary E.K ,Provance P.G .Muscles: Testing and Function, with Posture and Pain (Kendall, Muscles) Fifth, North American Edition. Philadelphia. Lippincott Williams & Wilkins, 2005. Jump up↑
- ↑ 5.0 5.1 5.2 Reiman, M. P., Bolgla, L. A., & Loudon, J. K.. A literature review of studies evaluating gluteus maximus and gluteus medius activation during rehabilitation exercises. Physiotherapy Theory and Practice,2012: 28(4): 257–268.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Presswood, L., Cronin, J., Keogh, J. W. L., & Whatman, C. . Gluteus Medius: Applied Anatomy, Dysfunction, Assessment, and Progressive Strengthening. Strength and Conditioning Journal. October 2008 : 30(5):41–53 .
- ↑ Kim H.J , Lee H.S, Jung H.G . Difference of Muscle Activity by Pelvic Tilt in Side-Lying Hip Abduction .Journal of The Korean Society of Physical Medicine. 2017:12(3): 59-66 .
- ↑ Barton CJ, Lack S, Malliaras P, Morrissey D. Gluteal muscle activity and patellofemoral pain syndrome: a systematic review. British journal of sports medicine. 2012 Sep 3:bjsports-2012.
- ↑ Buurke JH, Nene AV, Kwakkel G, Erren-Wolters V, IJzerman MJ, Hermens HJ. Recovery of gait after stroke: what changes?. Neurorehabilitation and Neural Repair. 2008 Nov 1;22(6):676-83.
- ↑ KendallK. D., Patel C., Wiley J. P., Pohl M. B., Emery C. A., etal .Steps Toward the Validation of the Trendelenburg Test. Clinical Journal of Sport Medicine.jan 2013: 23(1): 45–51.