Effective Quadriceps Training in Patellofemoral Pain: Difference between revisions
Kim Jackson (talk | contribs) m (Text replacement - "Physioplus" to "Plus ") |
Kim Jackson (talk | contribs) m (Text replacement - "Plus ." to "Plus.") |
||
| Line 7: | Line 7: | ||
Research into the cause of [[Patellofemoral Pain Syndrome|patellofemoral pain]] has been ongoing for decades. Looking back into the history of rehabilitation medicine, in the 1990's-2000's it was believed that deficits of the [[Vastus Medialis|vastus medialis oblique]] (VMO) of the [[Quadriceps Muscle|quadriceps]] was the culprit behind patellofemoral pain. Early research often used fixed cadavers rather than live subjects meaning the data had limited applicability and external validity with that literature. More recently, research has utilised electromyography (EMG) of the VMO in isolation. While studying the VMO in isolation is not entirely non useful, it limits the study's application to clinical practice. | Research into the cause of [[Patellofemoral Pain Syndrome|patellofemoral pain]] has been ongoing for decades. Looking back into the history of rehabilitation medicine, in the 1990's-2000's it was believed that deficits of the [[Vastus Medialis|vastus medialis oblique]] (VMO) of the [[Quadriceps Muscle|quadriceps]] was the culprit behind patellofemoral pain. Early research often used fixed cadavers rather than live subjects meaning the data had limited applicability and external validity with that literature. More recently, research has utilised electromyography (EMG) of the VMO in isolation. While studying the VMO in isolation is not entirely non useful, it limits the study's application to clinical practice. | ||
In more recent years, research has expanded to looking up and down the kinetic chain for a more holistic cause of patellofemoral pain. While there is a large volume of research around the quadriceps, in particular the VMO, it does not link causality to the quadriceps as the most likely problem or cause of patellofemoral pain. However, this does point to a way of predicting which rehabilitation patient will have VMO related patellofemoral pain.<ref name=":2">Robertson, C. Patellofemoral Joint Programme. Effective Quadriceps Training in Patellofemoral Pain. Plus . 2022.</ref> | In more recent years, research has expanded to looking up and down the kinetic chain for a more holistic cause of patellofemoral pain. While there is a large volume of research around the quadriceps, in particular the VMO, it does not link causality to the quadriceps as the most likely problem or cause of patellofemoral pain. However, this does point to a way of predicting which rehabilitation patient will have VMO related patellofemoral pain.<ref name=":2">Robertson, C. Patellofemoral Joint Programme. Effective Quadriceps Training in Patellofemoral Pain. Plus. 2022.</ref> | ||
== Patellofemoral Joint Biomechanics == | == Patellofemoral Joint Biomechanics == | ||
Revision as of 11:48, 18 August 2022
Top Contributors - Stacy Schiurring, Jess Bell and Kim Jackson
Introduction[edit | edit source]
Research into the cause of patellofemoral pain has been ongoing for decades. Looking back into the history of rehabilitation medicine, in the 1990's-2000's it was believed that deficits of the vastus medialis oblique (VMO) of the quadriceps was the culprit behind patellofemoral pain. Early research often used fixed cadavers rather than live subjects meaning the data had limited applicability and external validity with that literature. More recently, research has utilised electromyography (EMG) of the VMO in isolation. While studying the VMO in isolation is not entirely non useful, it limits the study's application to clinical practice.
In more recent years, research has expanded to looking up and down the kinetic chain for a more holistic cause of patellofemoral pain. While there is a large volume of research around the quadriceps, in particular the VMO, it does not link causality to the quadriceps as the most likely problem or cause of patellofemoral pain. However, this does point to a way of predicting which rehabilitation patient will have VMO related patellofemoral pain.[1]
Patellofemoral Joint Biomechanics[edit | edit source]
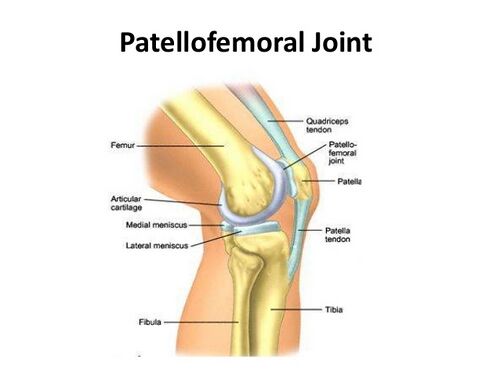
Please review this article for an overview of the patellofemoral joint.
Joint kinematics[edit | edit source]
The patella serves several mechanical functions.[2] It connects the muscles of knee extension to the tibia, and contributes to knee extension by transferring the force of the quadricep muscles to the tibia via the patellar tendon like a mechanical pulley.[3][2] The patella also alters the direction of the quadricep muscle force throughout knee range of motion (ROM).[2]
Overview of patellofemoral kinematics
- At full knee extension, the patella is located above the trochlear groove of the femur. Some of its articular surface is in contact at the distal lateral facets. The patella provides approximately 30% of the total knee extension torque at full knee extension.[2]
- During knee flexion, the patellar tendon pulls the patella into the trochlear groove which causes a slight medial translation.[3]
- At around 30° of knee flexion, the medial facets engage in the trochlear groove. Patella flexion increases with knee flexion. With increasing knee flexion, there is increasing patellar lateral translation and lateral tilt after an initial movement in the medial direction.[3]
- After 45° of knee flexion, the patella slowly moves into medial rotation.[3]
- In knee flexion greater than 90°, contact occurs on the proximal half of the medial and lateral facets.[3] The patella provides approximately 13% of total knee extension torque between 90 and 120° knee flexion.[2]
In open kinetic chain movements, the patella follows the path of the tibia due to the patellar tendon insertion at the tibial tubercle. The patella glides inferiorly during knee flexion and superiorly during knee extension. With a quadriceps set the patella should move approximately 10 mm superiorly. With knee flexion, the overall pattern of patellar contact area increases and serves to distribute joint forces over a larger surface area decreasing the likelihood of injury from repetitive high compressive forces.[2]
The patella also tracks lateral-medial-lateral during knee flexion. The patella moves approximately 3mm in each direction during medial and lateral displacement. As the knee flexes, the patella glides medially and becomes centered within the trochlear groove. During knee extension from 45° to 0° the patella tilts medially. At around 30° of flexion the patella glides back laterally and maintains this position for the remaining knee flexion. The motion has been described as a "C-curve pattern."[2]
In closed kinetic chain movements the patella remains in relatively in one place within the quadriceps tendon, this means the femur moves on the patella.
Please view the optional 11-minute video in resources section for a more detailed review of open versus closed kinetic chain exercises.
Quadriceps and patellar control[edit | edit source]
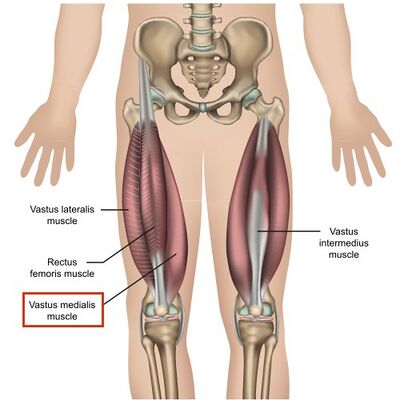
Please review the following articles for an overview of the quadricep muscles: (1) Rectus femoris, (2) Vastus lateralis, (3) Vastus medialis, and (4) Vastus intermedius.
VMO inhibition[edit | edit source]
The VMO has been the focus of much research in relation to patellofemoral pain. There are several scenarios where the VMO has no pull on the patella which causes joint dysfunction:[1]
- Swelling: Stoke and Young (1984) elegantly demonstrated that 40 mL of fluid can inhibit the vastus lateralis and only 10mL is needed to inhibit the VMO.[4] This is clinically relevant for patients who have a small effusion in the knee status post minor knee surgery. For example: a patient has undergone an arthroscopic meniscectomy then suddenly presents with post-operative patellofemoral pain. Often in those situations, an effusion has shut down the VMO which is driving some patellofemoral pain in conjunction with other risk factors.[1]
- Post-dislocation, or a heavy fall onto the knee: Approximately 50% of these patients, who do not have a patellar fracture, will have pain one year post injury, and often have an effusion as well. Situations such as surgery, dislocation, or trauma can set off an effusion which creates a dramatic change in the patient's dynamic stability.[1]
- Presence of pain: This is a similar group of patients, those which have had surgery, dislocation, fall, or other trauma. Hodges et al 2009 demonstrated that alterations in knee muscle activity can be caused by pain, even when that pain is of nonmuscle origin. The was done by injecting saline into the infrapatellar fat pad. EMG activity of the VMO was measured and found to be immediately slowed after the saline injection.[5]
It is important to remember that if a patient has a painful knee of any etiology for long enough, it will drive secondary VMO sluggishness and poor performance. In addition, the atrophy will create VMO muscle architecture change.[1]
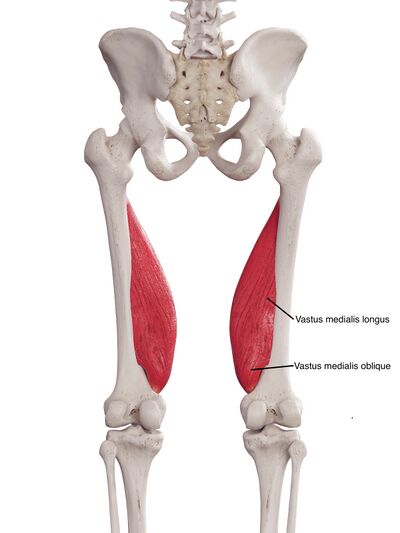
VM Muscle Architecture[edit | edit source]
Over the past few decades, rehabilitation science has been moving toward evidenced-based practice. This growing body of research provides validity to rehabilitation interventions and techniques. As recently as 2005, there was still uncertainty regarding the anatomical makeup and function of the quadriceps.
Timeline of quadricep research:
- Peeler et al 2005 performed a cadaver study to examine the anatomy and function on the VM. They observed that the VMO and the VML had different muscle fibre orientations depending on the angle of observation, but found no evidence of a fascial plane or separate innervation between the VMO and VML. They also stated that the VMO was not anatomically positioned to functional as a primary active stabiliser of the patella.[6]
- Ono et al 2005 also performed a cadaver study to examine the anatomical boundaries of the vastus medialis longus (VML) and the VMO. They observed that the line from the adductor hiatus to the medial rim of the patella are the boundary between the VMO and VML but concluded that a fascial plane was not required for a definitive separation between the VMO and VML. They confirmed different innervation of the VMO and the VML which suggested a difference in their functionality. The study also noted a difference in muscle fibre orientation between the VMO and VML.[7]
- Engelina et al 2014 performed an ultrasound investigation of the VMO in vivo. They observed that the VMO was a separate entity from the VML, confirmed the presence of a fascial plane between the VMO and the VML, and noted a difference in origin on the adductor muscles, different fibre orientation, and different nerve distribution. This study also found that the anatomy of the VM varied a great deal across the participant population.[8]
- Benjafield et al 2015 looked at how an individual's level of activity can affect the structure of the VMO. The authors utilised ultrasound (US) to assess the VMO fibre angles of both active and sedentary participants, and measured their activity level using the Tegner scoring system. They found that people classified as sedentary had a smaller fibre angle and a smaller amount of insertion onto the patella, and people classified as athletic had a large angle and a large insertion. A larger insertion onto the patella will provide a greater medial stabilizing force, this provides validity to the use of VMO strengthening exercise to management patellofemoral pain.[9]
- Khoshkhoo et al 2016 tried to determine if changes could be made to VMO architecture using a physiotherapy driven strengthening programme. Upon assessment following a 6-week quadriceps strengthening programme, participants had undergone a significant increase in VMO fibre angle and insertion length. These results are important because they support the use of skilled physiotherapy strengthening to create significant changes in VMO architecture to make it a better medial stabiliser.[10]
- Elniel et al 2017 compared the effects of closed-chain versus open-chain exercises on VMO architecture changes. They suggest that both types of exercise regimes have equal effects on the architecture of the VMO after six weeks of training.[11]
- Arnantha et al 2018 dove deeper into the details of exercise required to maintain changes in the VMO. They found that physiotherapy exercise programmes prescribed for patellofemoral pain have a positive effect on the VMO fibre angle and insertion level. However, exercises must be continued at a minimum of two times per week in order to maintain the gains achieved by the initial exercise programme. When exercises were discontinued after the initial exercise programme, participants experienced a slight reversal of the VMO architecture gains.[12]
- Hilal et al 2018 studied the effect of neuromuscular electrical stimulation (NMES) on VMO architecture. They found that the benefits of exercise can be greatly enhanced by the addition of NMES when looking at changes in the VMO architecture.[13]
This research clarifies the following:[1]
- The VMO is a separate entity from the VML
- The VMO and the VML have different muscle fibre orientations
- The VMO and the VML have different nerve distributions
- The anatomy of the VM varies across the population
- Exercise can effect the muscle architecture of the VMO
How does muscle architecture change?[edit | edit source]
The changes in VMO muscle fibre architecture is a result of muscle hypertrophy. Exercise induced hypertrophy does not change the number of fibres present, but changes the diameter of the muscle fibres. As the muscle fibre diameter increases, their orientation within the muscle changes as the fibres push against the surrounding fibres, changing their angle of pennation.[1]
Please view the following short optional video for a simple overview how muscular damage and repair result in muscular hypertrophy and growth.
Quadricep exercise theory[edit | edit source]
VMO Exercise considerations:[1]
- Focus on quadricep exercises rather than attempting to isolate the VMO individually
- Ideally do not exercise in the presence of swelling
- Do not exercise into pain beyond a 3 out of 10
- Consider icing before exercise, especially for post-surgical patients, to improve muscle fibre recruitment[15]
- Consider time of day when scheduling treatment sessions to manage soreness and or timing with pain medication
- Push to muscle fatigue on alternating days to create hypertrophy
- Consider blood flow restriction training if cannot effectively exercise to fatigue[16]
- Work synergistically with the gluteal muscles to encourage quality limb control
- Incorporate movements and activities that are meaningful to the patient and work toward their long-term goals
Closed-chain exercises[edit | edit source]
Steinkamp et al 1993 studied the knee moment, patellofemoral joint reaction force, and patellofemoral joint stress of 20 healthy adult subjects during leg press and leg extension exercises at 0°, 30°, 60°, and 90° of knee flexion. They found that all parametres were significantly greater in the leg extension exercise at 0°and 30° knee flexion; and that all parametres were significantly greater in the leg press exercise at 60°and 90° knee flexion. Patellofemoral joint stresses for exercises intersected at approximately 50° knee flexion. This study demonstrates that patients with patellofemoral joint arthritis may tolerate leg press exercise better than with leg extension exercise within functional ROM because of lower patellofemoral joint stresses as part of a rehabilitation programme.[17]
Progression of closed-chain exercises such as squats, lunges, or the leg press does not necessarily mean moving into deeper flexion, which is more likely to cause irritation. Progression can be modifying the activity by changing the load, the support surface, length of isometric hold, etc. Once the patient has improve their strength and endurance, it is appropriate to increase the depth of movement. Building their exercise tolerance slowly will decrease the likelihood of exercise induced muscle soreness.[1]
Early exercise progression example:[1]
- Limit ROM 0° to 50°, but increase the weight load
- Start with the double leg wall squat to 45°
- Stand with the majority of weight one leg, off-load the other foot on a step or ball, and perform isometric holds
- Increase the length of the isometric hold
- Come away from the wall, double leg squat but with some weight on a barbell or dumbbells
- Progress to double leg squat on unstable surface such a foam or a BOSU
Further progression of exercise can include close-chain between 0° and 45° and open-chain between 90° and 45°, to encourage work throughout the entire knee ROM. Vary the exercises and modify as appropriate to ensure the patient is achieving muscle fatigue. This is important because if the muscle does not work to fatigue, the patient does not get the recovery and will not achieve the desired muscle hypertrophy.[1]
Example of exercise prescription: [1]
- 4 sets of 8 reps to fatigue, alternate days
- Once the patient has achieved VMO architecture change, 3 or 4 sets of 20, with increased reps to fatigue
Open-chain exercises[1][edit | edit source]
- Perform in earlier stages of rehabilitation
- Limit ROM between 90° and 45°
- Seated exercises, with or without a therapy band
- Open chain leg extension machine
Resources[edit | edit source]
Optional Additional Reading:
- Barber-Westin S, Noyes FR. Blood flow–restricted training for lower extremity muscle weakness due to knee pathology: a systematic review. Sports Health. 2019 Jan;11(1):69-83.
- Loro WA, Thelen MD, Rosenthal MD, Stoneman PD, Ross MD. The effects of cryotherapy on quadriceps electromyographic activity and isometric strength in patient in the early phases following knee surgery. Journal of Orthopaedic Surgery. 2019 Feb 25;27(1):2309499019831454.
- Wheatley MG, Rainbow MJ, Clouthier AL. Patellofemoral mechanics: a review of pathomechanics and research approaches. Current Reviews in Musculoskeletal Medicine. 2020 Jun;13(3):326-37.
Optional Video:
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 Robertson, C. Patellofemoral Joint Programme. Effective Quadriceps Training in Patellofemoral Pain. Plus. 2022.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Loudon JK. Biomechanics and pathomechanics of the patellofemoral joint. International journal of sports physical therapy. 2016 Dec;11(6):820.
- ↑ 3.0 3.1 3.2 3.3 3.4 Wheatley MG, Rainbow MJ, Clouthier AL. Patellofemoral mechanics: a review of pathomechanics and research approaches. Current Reviews in Musculoskeletal Medicine. 2020 Jun;13(3):326-37.
- ↑ Stokes M, Young A. Investigations of quadriceps inhibition: implications for clinical practice. Physiotherapy. 1984 Nov;70(11):425-8.
- ↑ Hodges PW, Mellor R, Crossley K, Bennell K. Pain induced by injection of hypertonic saline into the infrapatellar fat pad and effect on coordination of the quadriceps muscles. Arthritis Care & Research. 2009 Jan 15;61(1):70-7.
- ↑ Peeler J, Cooper J, Porter MM, Thliveris JA, Anderson JE. Structural parameters of the vastus medialis muscle. Clinical Anatomy: The Official Journal of the American Association of Clinical Anatomists and the British Association of Clinical Anatomists. 2005 May;18(4):281-9.
- ↑ Ono T, Riegger-Krugh C, Bookstein NA, Shimizu ME, Kanai S, Otsuka A. The boundary of the vastus medialis oblique and the vastus medialis longus. Journal of Physical Therapy Science. 2005;17(1):1-4.
- ↑ Engelina S, Antonios T, Robertson CJ, Killingback A, Adds PJ. Ultrasound investigation of vastus medialis oblique muscle architecture: an in vivo study. Clinical Anatomy. 2014 Oct;27(7):1076-84.
- ↑ Benjafield AJ, Killingback A, Robertson CJ, Adds PJ. An investigation into the architecture of the vastus medialis oblique muscle in athletic and sedentary individuals: an in vivo ultrasound study. Clinical Anatomy. 2015 Mar;28(2):262-8.
- ↑ Khoshkhoo M, Killingback A, Robertson CJ, Adds PJ. The effect of exercise on vastus medialis oblique muscle architecture: an ultrasound investigation. Clinical anatomy. 2016 Sep;29(6):752-8.
- ↑ Elniel AR, Robertson C, Killingback A, Adds PJ. Open-chain and closed-chain exercise regimes: an ultrasound investigation into the effects of exercise on the architecture of the vastus medialis oblique. Phys Ther Rehabil. 2017;4:3.
- ↑ Arnantha, Harry, C. Robertson, A. Killingback and Philip J. Adds. “Maintenance of exercise-induced changes in the architecture of the VMO: how much is enough? An in-vivo ultrasound study.” (2018)
- ↑ Hilal Z, Robertson CJ, Killingback A, Adds PJ. The Effect of Exercise and Electrical Muscle Stimulation on the Architecture of the Vastus Medialis Oblique - The ‘Empi’ Electrotherapy J Ortho & Sport Med. 2018. (1)1-5.
- ↑ YouTube. What makes muscles grow? - Jeffrey Siegel| TED Ed. Available from: https://www.youtube.com/watch?v=2tM1LFFxeKg [last accessed 16/08/2022]
- ↑ Loro WA, Thelen MD, Rosenthal MD, Stoneman PD, Ross MD. The effects of cryotherapy on quadriceps electromyographic activity and isometric strength in patient in the early phases following knee surgery. Journal of Orthopaedic Surgery. 2019 Feb 25;27(1):2309499019831454.
- ↑ Barber-Westin S, Noyes FR. Blood flow–restricted training for lower extremity muscle weakness due to knee pathology: a systematic review. Sports Health. 2019 Jan;11(1):69-83.
- ↑ Steinkamp LA, Dillingham MF, Markel MD, Hill JA, Kaufman KR. Biomechanical considerations in patellofemoral joint rehabilitation. The American journal of sports medicine. 1993 May;21(3):438-44.
- ↑ YouTube. CLOSED VS OPEN KINETIC CHAIN MOVEMENTS. WHAT'S THE DIFFERENCE ? CKC Vs OKC !!! Available from: https://www.youtube.com/watch?v=3wwEyV5CdBM [last accessed 16/08/2022]