Duchenne Muscular Dystrophy: Difference between revisions
m (Text replace - ''''Lead Editors'''' to ''''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}') |
No edit summary |
||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- [[User:Rachael Lowe|Rachael Lowe]] | '''Original Editor '''- [[User:Rachael Lowe|Rachael Lowe]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
| Line 18: | Line 18: | ||
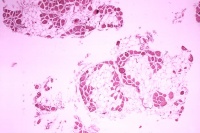
[[Image:Duchenne-muscular-dystrophy.jpg|thumb|right|200px|Histopathology of gastrocnemius muscle from patient who died of pseudohypertrophic muscular dystrophy, Duchenne type. Cross section of muscle shows extensive replacement of muscle fibers by adipose cells]] | [[Image:Duchenne-muscular-dystrophy.jpg|thumb|right|200px|Histopathology of gastrocnemius muscle from patient who died of pseudohypertrophic muscular dystrophy, Duchenne type. Cross section of muscle shows extensive replacement of muscle fibers by adipose cells]] | ||
The cause is a genetic change which affects the muscles. Muscles contain a protein (chemical) called dystrophin, which is necessary for muscles to function properly. People with DMD have a shortage of dystrophin in their muscles. The lack of dystrophin leads to muscle fibre damage and a gradual weakening of the muscles. The shortage of dystrophin is caused by a faulty gene.<br> | The cause is a genetic change which affects the muscles. Muscles contain a protein (chemical) called dystrophin, which is necessary for muscles to function properly. People with DMD have a shortage of dystrophin in their muscles. The lack of dystrophin leads to muscle fibre damage and a gradual weakening of the muscles. The shortage of dystrophin is caused by a faulty gene.<br> | ||
== Clinical Presentation == | == Clinical Presentation == | ||
| Line 26: | Line 26: | ||
The symptoms usually start around age 1-3 years, and may include: | The symptoms usually start around age 1-3 years, and may include: | ||
*Difficulty with walking, running, jumping and climbing stairs. Walking may look different with a 'waddling' type of walk. The boy may be late in starting to walk (although many children without DMD also walk late). | *[[Duchenne_gait|Difficulty with walking]], running, jumping and climbing stairs. Walking may look different with a 'waddling' type of walk. The boy may be late in starting to walk (although many children without DMD also walk late). | ||
*When you pick the child up, you may feel as if he 'slips through your hands', due to looseness of the muscles around the shoulder. | *When you pick the child up, you may feel as if he 'slips through your hands', due to looseness of the muscles around the shoulder. | ||
*The calf muscles may look bulky, although they are not strong. | *The calf muscles may look bulky, although they are not strong. | ||
| Line 33: | Line 33: | ||
*Sometimes, a delay in development may be the first sign of DMD. The child's speech development may also be delayed. Therefore, a boy whose development is delayed, may be offered a screening test for DMD. However, DMD is only one of the possible causes of developmental delay - there are many other causes not related to DMD.<br> | *Sometimes, a delay in development may be the first sign of DMD. The child's speech development may also be delayed. Therefore, a boy whose development is delayed, may be offered a screening test for DMD. However, DMD is only one of the possible causes of developmental delay - there are many other causes not related to DMD.<br> | ||
{| cellspacing="1" cellpadding="1 | {| width="100%" cellspacing="1" cellpadding="1" | ||
|- | |- | ||
| {{#ev:youtube|o1uhhpjmzkw|250}} <ref>armando hasudungan. Muscular Dystrophy - Duchenne, Becker and Mytonic. Available from: http://www.youtube.com/watch?v=o1uhhpjmzkw[last accessed 25/05/13]</ref> | | {{#ev:youtube|o1uhhpjmzkw|250}} <ref>armando hasudungan. Muscular Dystrophy - Duchenne, Becker and Mytonic. Available from: http://www.youtube.com/watch?v=o1uhhpjmzkw[last accessed 25/05/13]</ref> | ||
| Line 72: | Line 72: | ||
==== Age 5-8 years ==== | ==== Age 5-8 years ==== | ||
At this age, some support may be needed for the legs and ankles. For example, using night time ankle splints, or with a knee-ankle-foot orthosis. There is no evidence of significant benefit from any intervention for increasing ankle range of motion<ref>Rose KJ, Burns J, Wheeler DM, North KN. [http://www.cochrane.org/reviews/en/ab006973.html Interventions for increasing ankle range of motion in patients with neuromuscular disease]. Cochrane Database Syst Rev. 2010 Feb 17;2:CD006973. | At this age, some support may be needed for the legs and ankles. For example, using night time ankle splints, or with a knee-ankle-foot orthosis. There is no evidence of significant benefit from any intervention for increasing ankle range of motion<ref>Rose KJ, Burns J, Wheeler DM, North KN. [http://www.cochrane.org/reviews/en/ab006973.html Interventions for increasing ankle range of motion in patients with neuromuscular disease]. Cochrane Database Syst Rev. 2010 Feb 17;2:CD006973.fckLR.</ref>. | ||
.</ref>. | |||
Treatment with corticosteroids can help to maintain the child's muscle strength. This involves taking medication such as prednisolone or deflazacort as a long-term treatment, either continuously or in repeated courses. <br> | Treatment with corticosteroids can help to maintain the child's muscle strength. This involves taking medication such as prednisolone or deflazacort as a long-term treatment, either continuously or in repeated courses. <br> | ||
==== 8 years-late teenage years ==== | ==== 8 years-late teenage years ==== | ||
| Line 105: | Line 104: | ||
Muscle weakness can result in joint contractures. In DMD, it is often the ankle joint and Achilles' tendon which become tight. This can be treated either using orthotic devices or by surgical release of the tendon. | Muscle weakness can result in joint contractures. In DMD, it is often the ankle joint and Achilles' tendon which become tight. This can be treated either using orthotic devices or by surgical release of the tendon. | ||
[[Scoliosis|Scoliosis]] can occur due to muscle weakness. Usually this happens sometime after the child needs a wheelchair. The scoliosis can cause discomfort and is not helpful for posture and breathing. Treatments which can help are a spinal brace, or surgery to the spine. Surgery has been shown to improve function and quality of life<ref>Takaso M, Nakazawa T, Imura T, Okada T, Fukushima K, Ueno M, Takahira N, Takahashi K, Yamazaki M, Ohtori S, Okamoto H, Okutomi T, Okamoto M, Masaki T, Uchinuma E, Sakagami H. | [[Scoliosis|Scoliosis]] can occur due to muscle weakness. Usually this happens sometime after the child needs a wheelchair. The scoliosis can cause discomfort and is not helpful for posture and breathing. Treatments which can help are a spinal brace, or surgery to the spine. Surgery has been shown to improve function and quality of life<ref>Takaso M, Nakazawa T, Imura T, Okada T, Fukushima K, Ueno M, Takahira N, Takahashi K, Yamazaki M, Ohtori S, Okamoto H, Okutomi T, Okamoto M, Masaki T, Uchinuma E, Sakagami H.fckLR[http://www.springerlink.com/content/e3t255860636tt2g/?p=db2743826c244dfc9be65b4887e83987&amp;pi=0 Surgical management of severe scoliosis with high risk pulmonary dysfunction in Duchenne muscular dystrophy: patient function, quality of life and satisfaction]. Int Orthop. 2010 Feb 16. [Epub ahead of print]</ref>.<br> | ||
[http://www.springerlink.com/content/e3t255860636tt2g/?p=db2743826c244dfc9be65b4887e83987&pi=0 Surgical management of severe scoliosis with high risk pulmonary dysfunction in Duchenne muscular dystrophy: patient function, quality of life and satisfaction]. Int Orthop. 2010 Feb 16. [Epub ahead of print]</ref>.<br> | |||
==== Nutrition and digestion ==== | ==== Nutrition and digestion ==== | ||
| Line 156: | Line 154: | ||
<references /> | <references /> | ||
[[Category:Neurology]] [[Category:Paediatrics]] | |||
Revision as of 17:05, 4 July 2013
Original Editor - Rachael Lowe
Top Contributors - Pacifique Dusabeyezu, Alyssa Aquino, Rachael Lowe, Kim Jackson, Nikhil Benhur Abburi, Rucha Gadgil, Admin, Shaimaa Eldib, Laura Ritchie, Faye Underwood, WikiSysop, Vidya Acharya, Evan Thomas, Naomi O'Reilly, Michelle Lee, Lucinda hampton, 127.0.0.1 and Audrey Brown
Introduction[edit | edit source]
Duchenne's muscular dystrophy (DMD) is a genetic condition which affects the muscles, causing muscle weakness. It is a serious condition which starts in early childhood. The muscle weakness is not noticeable at birth, even though the child is born with the gene which causes it. The weakness develops gradually. It usually shows up in early childhood. Symptoms are mild at first, but increase as the child gets older.
It is one of more than 20 types of muscular dystrophy. All the muscular dystrophies are caused by faults in genes (the units of inheritance that parents pass on to their children) and they cause progressive muscle weakness because muscle cells break down and are gradually lost. The Duchenne type affects only boys (with extremely rare exceptions) and a problem in this gene is known to result in a defect in a single important protein in muscle fibres called dystrophin. It is named after Dr Duchenne de Boulogne who worked in Paris in the mid-19th century who was one of the first people to study the muscular dystrophies.
Clinically Relevant Anatomy
[edit | edit source]
add text here relating to clinically relevant anatomy of the condition
Mechanism of Injury / Pathological Process
[edit | edit source]
The cause is a genetic change which affects the muscles. Muscles contain a protein (chemical) called dystrophin, which is necessary for muscles to function properly. People with DMD have a shortage of dystrophin in their muscles. The lack of dystrophin leads to muscle fibre damage and a gradual weakening of the muscles. The shortage of dystrophin is caused by a faulty gene.
Clinical Presentation[edit | edit source]
The muscle weakness is mainly in the 'proximal' muscles, which are those near the trunk of the body, around the hips and the shoulders. This means that fine movements, such as those using the hands and fingers, are less affected than movements like walking.
The symptoms usually start around age 1-3 years, and may include:
- Difficulty with walking, running, jumping and climbing stairs. Walking may look different with a 'waddling' type of walk. The boy may be late in starting to walk (although many children without DMD also walk late).
- When you pick the child up, you may feel as if he 'slips through your hands', due to looseness of the muscles around the shoulder.
- The calf muscles may look bulky, although they are not strong.
- As he gets older, the child may use his hands to help him get up, looking as if he is 'climbing up his legs'. This is called 'Gower's sign'.
- Some boys with DMD also have a learning difficulty. Usually this is not severe.
- Sometimes, a delay in development may be the first sign of DMD. The child's speech development may also be delayed. Therefore, a boy whose development is delayed, may be offered a screening test for DMD. However, DMD is only one of the possible causes of developmental delay - there are many other causes not related to DMD.
| [1] | [2] [3] |
Diagnostic Procedures[edit | edit source]
The diagnosis may be suspected because of the child's symptoms (above). When looking for signs of DMD, it is important to watch the child running and getting up from the floor - the muscle weakness is more noticeable during these activities.
Tests are needed before DMD can be diagnosed. The first step in making the diagnosis is a blood test. This tests for creatine kinase. Children with DMD always have a very high level of creatine kinase (about 10-100 times normal). Therefore if a child's creatine kinase level is normal, then DMD is ruled out. If the creatine kinase level is high, further tests are needed to see whether this is due to DMD or to some other condition.
The next step in diagnosing DMD involves either a muscle biopsy and/or genetic tests:
- A muscle biopsy involves taking a small sample of a muscle, under local anaesthetic. The sample is examined under a microscope using special techniques to look at the muscle fibres and the dystrophin protein.
- Genetic tests are done using a blood sample. The DNA in the blood is tested to look at the dystrophin gene. This test can diagnose most cases of DMD.
Outcome Measures[edit | edit source]
add links to outcome measures here (see Outcome Measures Database)
Management / Interventions
[edit | edit source]
There is no cure for DMD at present. The proactive symptom-based multidisciplinary team (MDT) management and access to non-invasive ventilation have enabled improved survival into adulthood[4].
Preschool age[edit | edit source]
Usually, at this stage, the child will be well and not need much treatment. What you will usually be offered is:
- Provide information about DMD and patient support groups.
- Referral to a specialist team (for example, a paediatrician or neurologist, physiotherapist and a specialist nurse) to monitor child health.
- Advice about the right level of exercise.
- Genetic advice for the family.
Age 5-8 years[edit | edit source]
At this age, some support may be needed for the legs and ankles. For example, using night time ankle splints, or with a knee-ankle-foot orthosis. There is no evidence of significant benefit from any intervention for increasing ankle range of motion[5].
Treatment with corticosteroids can help to maintain the child's muscle strength. This involves taking medication such as prednisolone or deflazacort as a long-term treatment, either continuously or in repeated courses.
8 years-late teenage years[edit | edit source]
At some time after the age of 8 years, the child's leg muscles become significantly weaker. Walking gradually gets more difficult, and a wheelchair is needed. The age at which this happens varies from person to person. Often it is around age 9-11 years, although with corticosteroid treatment, some boys can walk for longer.
After the child starts needing a wheelchair, this is also the time that complications tend to begin, so it is important to monitor the boy's health and to treat any complications early.
Practical support and equipment will be needed at this stage, for example, wheelchairs and adaptations to the child's home and school.
Counselling and emotional support for child and family may be helpful.
Late teenage years-twenties[edit | edit source]
At this stage, muscle weakness becomes more problematic. Increasing help and adaptations are needed. Complications such as chest infections are likely to increase, so more medical monitoring and treatment are required.
Complications
[edit | edit source]
Anaesthetics[edit | edit source]
People with DMD need extra care if they have a general anaesthetic. Certain anaesthetic medicines can cause a harmful reaction for people who have DMD. Also, extra care for the chest and breathing is needed. It is important to have a pre-operative assessment and a senior anaesthetist providing the anaesthetic care.
Osteoporosis[edit | edit source]
People with DMD may develop osteoporosis. This is due to lack of mobility and also to steroid treatment. It is important to prevent osteoporosis as far as possible. A good intake of vitamin D and calcium can help. Sometimes a blood test to check vitamin D levels is advised, and vitamin D supplements may be offered.
Joint and spinal complications[edit | edit source]
Muscle weakness can result in joint contractures. In DMD, it is often the ankle joint and Achilles' tendon which become tight. This can be treated either using orthotic devices or by surgical release of the tendon.
Scoliosis can occur due to muscle weakness. Usually this happens sometime after the child needs a wheelchair. The scoliosis can cause discomfort and is not helpful for posture and breathing. Treatments which can help are a spinal brace, or surgery to the spine. Surgery has been shown to improve function and quality of life[6].
Nutrition and digestion[edit | edit source]
Some children with DMD are prone to being overweight, especially if taking steroid treatment. Teenagers and adults with DMD may be underweight, due to loss of muscle bulk. Dietary advice can be helpful in these situations.
Constipation can be a symptom for anyone who is not mobile. This can be treated with laxatives and a high fibre diet.
In the later stages of DMD (as a young adult and older), people with DMD may have difficulty with chewing and swallowing food. They may need a careful assessment and nutritional advice or supplements. If the problem is severe, then a gastrostomy may be needed.
Chest and breathing complications[edit | edit source]
During the teenage years, the breathing muscles weaken, causing shallow breathing and a less effective cough mechanism which can lead to chest infections. Clearance techniques and non-invasive ventilation may help.
As the breathing muscles get weaker, oxygen levels in the blood may be reduced, more so while sleeping. Because this develops gradually, the symptoms may not be obvious. Possible symptoms are tiredness, irritability, morning headaches, night time waking and vivid dreams.
It is helpful if breathing problems are detected and treated early; so patients with DMD will usually be offered regular lung function tests once they start to have significant muscle weakness.
Cardiac (heart) complications[edit | edit source]
Teenagers and adults with DMD may develop cardiomyopathy. With DMD, the cardiomyopathy does not usually cause much in the way of symptoms. Possible symptoms are tiredness, leg swelling, shortness of breath or an irregular heart beat. Cardiomyopathy can be helped by medication which seems to work best if started at an early stage, before symptoms are noticed. So people with DMD are usually offered regular heart check-ups, starting from early childhood. The check-ups usually involve an ECG and Echocardiogram.
Differential Diagnosis
[edit | edit source]
add text here relating to the differential diagnosis of this condition
Key Evidence[edit | edit source]
add text here relating to key evidence with regards to any of the above headings
Resources
[edit | edit source]
Duchenne Muscular Dystrophy Factsheet
Case Studies[edit | edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1rswI4Lv9k94Zah_6R5ZDG1tEdtin6N47-HpgRWVIOSmhgo195|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
- ↑ armando hasudungan. Muscular Dystrophy - Duchenne, Becker and Mytonic. Available from: http://www.youtube.com/watch?v=o1uhhpjmzkw[last accessed 25/05/13]
- ↑ lucasramirez125. duchenne muscular dystrophy.wmv. Available from: http://www.youtube.com/watch?v=_aIAErxBskc [last accessed 25/05/13]
- ↑ ilm kidunya. Duchenne Muscular Dystrophy by Dr Khalid Jamil Akhtar. Available from: http://www.youtube.com/watch?v=vbz6UG4iHhs [last accessed 25/05/13]
- ↑ Manzur AY, Muntoni F; Diagnosis and new treatments in muscular dystrophies. J Neurol Neurosurg Psychiatry. 2009 Jul;80(7):706-14.
- ↑ Rose KJ, Burns J, Wheeler DM, North KN. Interventions for increasing ankle range of motion in patients with neuromuscular disease. Cochrane Database Syst Rev. 2010 Feb 17;2:CD006973.fckLR.
- ↑ Takaso M, Nakazawa T, Imura T, Okada T, Fukushima K, Ueno M, Takahira N, Takahashi K, Yamazaki M, Ohtori S, Okamoto H, Okutomi T, Okamoto M, Masaki T, Uchinuma E, Sakagami H.fckLRSurgical management of severe scoliosis with high risk pulmonary dysfunction in Duchenne muscular dystrophy: patient function, quality of life and satisfaction. Int Orthop. 2010 Feb 16. [Epub ahead of print]