Deep Gluteal Pain Syndrome: Difference between revisions
No edit summary |
No edit summary |
||
| Line 46: | Line 46: | ||
This entrapment can be triggered by prolonged sitting especially on the bike or a recent change of the bike saddle. Usually, the symptoms could be aggravated by sitting, however, sitting on the toilet seat is reported to ease the pain due to the release of pressure off the nerve. | This entrapment can be triggered by prolonged sitting especially on the bike or a recent change of the bike saddle. Usually, the symptoms could be aggravated by sitting, however, sitting on the toilet seat is reported to ease the pain due to the release of pressure off the nerve. | ||
== Ischiofemoral | == Ischiofemoral Impingement == | ||
Following hip operations especially total hip replacement, some patients were reported to complain of posterior leg and deep buttock ache, especially with hip extension and adduction<ref name=":0" />. Ischiofemoral pain is a rare cause of hip pain first described in three patients after total hip arthroplasty and proximal femoral osteotomy<ref>Johnson KA. Impingement of the lesser trochanter on the ischial ramus after total hip arthroplasty. Report of three cases. J Bone Joint Surg Am 1977; 59: 268–9.</ref> | |||
The | The Ischiofemoral space is very small space bordered by the Ischial Tuberosity and the lesser trochanter. Quadratus Femoris<ref>Taneja AK, Bredella MA, Torriani M. Ischiofemoral impingement. Magn Reson Imaging Clin N Am 2013; 21: 65–73.</ref> tightness/thickness or inflammation such as bursitis can cause narrowing and impingement on the nociceptive structures in that region. A study linked symptoms to the shortened distance between the bony margins of the ischium and the femur as measured on axial magnetic resonance imaging (MRI) sequences<ref>Gollwitzer H, Banke IJ, Schauwecker J, Gerdesmeyer L, Suren C. How to address ischiofemoral impingement? Treatment algorithm and review of the literature. Journal of Hip Preservation Surgery. 2017 Dec;4(4):289-98.</ref> | ||
Symptoms: | '''Symptoms:''' | ||
* Deep-seated buttock pain often described as a deep ache, sometimes radiates to the knee | |||
* Short strides are often easier than long strides when running. This is due to the narrowing of the Ischiofemoral space with hip extension and adduction increased with the stride length | |||
* Facet type pain at L3-4, or L4-5 which could be confused with a primary lumbar problem. Back pain could be due to the loss of hip extension | |||
* Ischiofemoral Impingement pain is worse with terminal hip extension and adduction | |||
* Tenderness on palpation of the ischium during passive provocative movement <ref>Wilson MD, Keene JS. Treatment of ischiofemoral impingement: results of diagnostic injections and arthroscopic resection of the lesser trochanter. J Hip Preserv Surg 2016; 3: 146–53</ref> | |||
* Snapping, clicking or locking sensation of the hip joint during long-stride walking caused by the lesser trochanter forcefully bypassing the ischium | |||
Physical examination findings are not conclusive on the diagnosis of Ischiofemoral Impingement. The combination of passive extension, adducting and external rotation the hip is used to provoke the symptoms<ref>Safran M, Ryu J. Ischiofemoral impingement of the hip: a novel approach to treatment. Knee Surg Sports Traumatol Arthrosc 2014; 22: 781–5.</ref>. | |||
The long stride walking test (walking with large steps) has a sensitivity of 92% and a specificity of 82% <ref>4. Gomez-Hoyos J, Martin RL, Schroder R et al. Accuracy of 2 clinical tests for ischiofemoral impingement in patients with posterior hip pain and endoscopically confirmed diagnosis. Arthroscopy 2016; 32: 1279–84</ref> | |||
== Hamstring tendinopathy == | == Hamstring tendinopathy == | ||
Revision as of 20:37, 22 October 2020
Introduction[edit | edit source]
The deep buttock area has complicated anatomy and hasn't been explored in-depth in the litreature[1]. Symptoms of pain and dysfunction in this area can be manifestations of different conditions such as Sacroiliac JointDysfunciton, Gluteal Tendinopathy, Lumbar Radiculopathy and Piriformis Syndrome. Recent literature has investigated the involvement of various structures in the development of symptoms.
Gluteal Pain Syndrome (DGS) is defined as pain or numbness in the buttock[2], the hip, or the posterior thigh with radiation or radicular pain in the Sciatic verve distribution[3]. This condition is characterized by being[4]:
- Non-discogenic
- A Sciatic nerve disorder
- Nerve entrapment in the deep gluteal space. The most common sites of entrapment are: piriformis muscle (67.8%), sciatic foramen (6%), ischial tunnel (4.7%)[5]
Gluteal Pain Syndrome is an umbrella of different conditions with similar and overlapping symptoms.
Symptoms of Gluteal Pain Syndrome[3]:
- Buttock and often retro greater trochanter pain
- Bilateral but usually unilateral symptoms
- Pain with prolonged sitting (longer than 20-30 minutes)
- Pain with stride into a terminal extension
- Patients could be limp with walking
- Neurological sensory changes
- Severe night pain with disturbed sleep
Anatomy[edit | edit source]
The deep gluteal space has a unique anatomy. Understanding of its boundaries and contacts help in improving the clinicians' palpation skills and the diagnosis of patients symptoms and presentation.
The deep gluteal space is bounded by:
- Posteriorly, the gluteus maximus
- Anteriorly, posterior acetabular column, hip joint capsule and proximal femur
- Laterally, lateral lip of linea aspera and gluteal tuberosity
- Medially, sacrotuberous ligament and falciform fascia
- Superiorly, inferior margin of the sciatic notch
- Inferiorly, proximal origin of the hamstrings at ischial tuberosity[6]
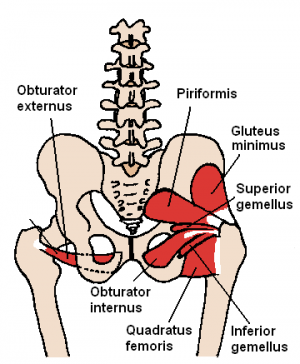
The deep Six are important structures that lie underneath Underneath the Glutes Maximus and Medius. The deep six are the Piriformis muscle, the Superior Gemelli, Obturator nternis, Obturator Externus,[7] Inferior Gemelli and Quadratus Femoris[8]. The Piriformis and the Quadratus Femoris are the easiest to palpate[3].
The Sciatic Nerve lies over the Obturator and Gemelli complex[9] then it sits laterally to the Ischial Tuberosity where the Biceps Femoris attaches. It is bound on the medial side, by the Ischial Tuberosity and on the lateral side, by the lesser trochanter of the femur.
Pudendal Nerve Entrapment[edit | edit source]
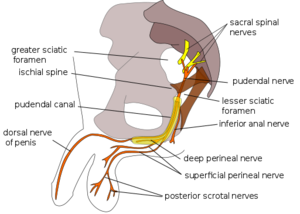
The Sacrotuberous Ligament comes from the Ischial Tuberosity and inserts onto the sacrum and the coccyx while the Sacrospinous Ligament lies at 90 degrees to it, deep to the Sacrotuberous Ligament and attaches onto the Ischial Spine. The thickness of these ligaments could result in entrapment of the Pudendal Nerve, often referred to as Alcock Canal Syndrome or Cyclist Syndrome[3].
In addition to the buttock pain, symptoms of the pudendal nerve include sexual dysfunction, rectal pain, faecal incontinence, and urinary incontinence. Pudendal Nerve entrapment could significantly affect the quality of life.
This entrapment can be triggered by prolonged sitting especially on the bike or a recent change of the bike saddle. Usually, the symptoms could be aggravated by sitting, however, sitting on the toilet seat is reported to ease the pain due to the release of pressure off the nerve.
Ischiofemoral Impingement[edit | edit source]
Following hip operations especially total hip replacement, some patients were reported to complain of posterior leg and deep buttock ache, especially with hip extension and adduction[3]. Ischiofemoral pain is a rare cause of hip pain first described in three patients after total hip arthroplasty and proximal femoral osteotomy[10]
The Ischiofemoral space is very small space bordered by the Ischial Tuberosity and the lesser trochanter. Quadratus Femoris[11] tightness/thickness or inflammation such as bursitis can cause narrowing and impingement on the nociceptive structures in that region. A study linked symptoms to the shortened distance between the bony margins of the ischium and the femur as measured on axial magnetic resonance imaging (MRI) sequences[12]
Symptoms:
- Deep-seated buttock pain often described as a deep ache, sometimes radiates to the knee
- Short strides are often easier than long strides when running. This is due to the narrowing of the Ischiofemoral space with hip extension and adduction increased with the stride length
- Facet type pain at L3-4, or L4-5 which could be confused with a primary lumbar problem. Back pain could be due to the loss of hip extension
- Ischiofemoral Impingement pain is worse with terminal hip extension and adduction
- Tenderness on palpation of the ischium during passive provocative movement [13]
- Snapping, clicking or locking sensation of the hip joint during long-stride walking caused by the lesser trochanter forcefully bypassing the ischium
Physical examination findings are not conclusive on the diagnosis of Ischiofemoral Impingement. The combination of passive extension, adducting and external rotation the hip is used to provoke the symptoms[14].
The long stride walking test (walking with large steps) has a sensitivity of 92% and a specificity of 82% [15]
Hamstring tendinopathy[edit | edit source]
The insertion point of the Hamstring is on the Ischial Tuberosity, which is very close to the Sciatic Nerve is also in that region. This condition has different symptoms.
Patients have increased the loading of flexion. So they've maybe done deadlifts or some flexion activity, that is compressing the, or tensioning the Hamstring tendon on the Ischial Tuberosity.
Pain gets worse with sitting.
They may have worse pain running uphill when they flex their trunk, which is causing more compression on the Hamstring tendon, on the Ischial Tuberosity.
They can have pain with driving because the Sciatic Nerve is very closely related to the Hamstring tendon.
They might have a positive straight leg raise.
They will almost definitely have a positive slump because it's very hard to differentiate out Sciatic Nerve path from this region from the Hamstring tendinopathy. And they really feel like they're sitting on a boggy mass. And they might feel like if they sit on a doughnut or something to take the pressure off that area, they feel a lot more comfortable.
And you'll often feel a thickening on palpation, if you feel around that Ischial Tuberosity, just lateral to the Ischium.
In all of the above conditions, patients can have positive neurodynamic tests as they experience pain with flexion and with terminal hip extension.
A history of repetitive Hamstring loading with hip flexion, such as with uphill running or picking up boxes, or maybe they moving house. Then we think it could be a reactive Hamstring tendon, or possibly bursitis. Similarly, if they feel like they're sitting on a boggy mass, along with that history that I've just described to you think Hamstring tendinopathy or bursitis.
Proximal hamstring tendinopathy (PHT) is common among distance runners and athletes performing either primarily sagittal plane (eg, sprinting, hurdling) or change-of-direction activities (eg, various football codes and hockey)[16]
The condition may also affect people who do not participate in sport ot uncommonly, presents bilaterally in this demographic. Characteristics of PHT include deep, localized pain in the region of the ischial tuberosity that often worsens during or after running, lunging squatting, and sitting.
The hamstring muscles have a common origin on the lateral aspect of the ischial tuberosity. Semitendinosus and the long head of the biceps femoris share a conjoined tendon originating from the lateral facet, whereas the semimembranosus origin is deeper,67 although anatomical variation is reported.
Proximal hamstring tendinopathy is considered to be an insertional tendinopathy, and compression of the tendon at its attachment during hip flexion/adduction is thought to be a key etiological factor
Shear force between the hamstring attachment and ischial tuberosity has been reported when replicating in vivo loading,36 as well as increased displacement of the proximal hamstring tendon with increased hip flexion angle.3
Etiology of tendinopathy is multifactorial, involving load-related extrinsic and intrinsic factors. Extrinsic factors include training errors, such as increasing volume or intensity too quickly, particularly the sudden introduction of sprinting, lunging, hurdles, or hills sprinting, lunging, hurdles, or hills. Several case series42,95 have been identified that report these training errors to precede PHT. These activities require the hamstring to contract or lengthen while in hip flexion and may result in provocative tensile and compressive load at the tendon insertion
An understanding of hamstring muscle function is important in PHT rehabilitation. In upright running, which can be a key aggravating factor in athletic populations, the hamstrings eccentrically decelerate knee extension in the terminal swing phase. Peak force occurs in late swing, with a second peak reported in early stance.
Energy storage in the late swing to early stance stretch/shorten cycle is likely to be a major contributor to hamstring origin overuse injury, and eccentric/ concentric transition is associated with higher hamstring loads.79 Elastic energy storage in the tendons and aponeuroses increases efficiency of locomotion at higher speeds in animals. 2 The hamstring origin may be subject to higher energy storage loads in greater hip or trunk flexion, for example, when running with forward trunk lean, overstriding, and during uphill running. Given these functional requirements, eccentric bias and stretch/shorten cycle exercise have been recommended by some authors for hamstring muscle injury to facilitate muscle hypertrophy, strength, and length-tension changes (greater strength nearer to end range),55 as well as return to sport.8,88
iagnosis of PHT is complex, requiring careful elucidation of subjective history, screening of other potential pathology, and utilization of commonly advocated diagnostic tests. Subjective assessment of typical tendon pain behavior should confirm well-localized ischial tuberosity pain that becomes less symptomatic after a few minutes of activity (eg, “warm-ups” when running) but is worse afterward.
Activities requiring deeper hip flexion, such as squatting or lunging and sitting for long periods, especially on harder surfaces, are often provocative. Proximal hamstring tendinopathy is rarely painful during activities that do not involve energy storage or compression, such as slow walking on a level surface, standing, and lying. There may be stiffness in the morning or when starting to move after prolonged rest. Some pain provocation after energy storage activities may be acceptable during rehabilitation, providing it lasts no longer than 24 hours
specific differential palpation, and imaging. Not uncommonly in more chronic presentations, apparent isolated hamstring pathology may coexist with other pathologies, adding further complexity to both diagnosis and management.
An example of a load test assessment for these patients may consist of progression from the single-leg bent-knee bridge (a low-load clinical test; FIGURE 1A) to the long-lever bridge (moderate-load test; FIGURE 1B) to arabesque (FIGURE 1C) movements and the single-leg deadlift (high-load clinical tests).24 These motions may be initiated slowly, adding speed if asymptomatic. The pain score should increase with load across these tests.
Three passive stretch tests (bent-knee stretch, modified bent-knee stretch, and Puranen-Orava test) have moderate to high validity and high sensitivity and specificity for diagnosis of PHT
Sciatic Nerve[edit | edit source]
Pain radiating down their leg with hip flexion or with a neurodynamic test.
Could be from the deep gluteal space or discogenic pathology.
Pain with increased time on a bike, change of saddle, and sitting on a toilet seat eases, think Pudendal Nerve entrapment
Pain with hip extension or long-striding, think Ischiofemoral impingement, or Sacroiliac joint pathology or lumbar spine.
History of trauma or hip surgery, pain with extension after hip arthroscopy or a hip replacement could be Ischiofemoral Impingement.
Pain with sitting for a while and getting up with limp could be different things a Hamstring tendon problem, Gluteal tendinopathy, Obturator-Gemelli insertional tendinopathy. That sort of limping after you get up from prolonged sitting is a very common symptom of that entire buttock area, including the lateral hip.
The Sciatic Nerve
The Sciatic Nerve could be possibly trapped at different sites by different muscles:
Underneath the Piriformis muscle [17]
the nerve kinematics is a crucial aspect of the entrapment’s pathophysiology[6].
Deep hip flexion, abduction and external rotation, the sciatic nerve glide across the posterior border of the greater trochanter. Additionally, in the full flexed, abducted externally rotated state, the semimembranosus origin and the posterior edge of the greater trochanter can come into contact
Excursion of the nerve is dependent upon the flexion of the knee. When the knee is flexed, the nerve moves posterolateral and when the knee is extended the nerve moves deep into the tunnel[18]
Examination[edit | edit source]
Lumbar spine pathology has to be ruled out. Palpation it, but see if you can rule out your lumbar spine pathology. Tests of the pelvic girdle type or SI-joint type pain, such as the March test and the active straight leg raise test.
Patients with sciatic nerve entrapment often have previous history of trauma and symptoms of sit pain, radicular pain of the lower back or hip and paresthesias of the affected leg[19]
The problem is that no studies have ever been done, as yet, looking to see what happens in somebody with deep gluteal pain when you perform an active straight leg raise test, and you provide force closure or compression by approximating the ASIS or the PSIS. A positive March test or active straight leg raise test, indicate poor motor control and failed load transfer, but don't rule out the source of the patient's presentation.
The total arc of motion of the hip, FADIR test to rule out OA. FADIR. A negative FADIR can rule out intra-articular pathology of the hip, such as labral damage or osteoarthritis of the hip.
The FABER test is validated for SI-joint dysfunction. A positive Faber test, remember also that when you do that test the Sciatic Nerve glides across the posterior border of the greater trochanter in that position. So a positive test could actually implicate Sciatic Nerve path.
FADER, FADER with a resisted internal rotation could be positive in somebody with Gluteal tendinopathy, Piriformis or a deep buttock symptom. Pain felt directly on the greater trochanter could be more Gluteal tendinopathy. Pain deep in the buttock is more likely to be compression or tendinopathy or irritation around the Piriformis muscle or some of the deep six.
Patients with Deep Gluteal Pain Syndrome, you can have altered nerve conduction tests. So you can have changes in reflexes, motor weakness[20], and sensation changes. So those tests again, will not help you differentiate out lumbar spine from the buttock.
Palpation can be extremely helpful. The referred symptoms can be confusing because there's an overlap around all these nociceptive structures. But your palpation skills can help you differentiate out more of an Obturator-Gemelli primary problem. Pain at the posterior hip Versus Gluteal tendinopathy.
The worst pain would be on the superior aspect of the greater trochanter versus Hamstring tendinopathy where you would palpate a boggy mass around the Ischial tuberosity itself.
So if you can become familiar with the anatomy, it will mean that your palpation skills may add value when you assess using all the clinical pictures that we've discussed.
https://www.youtube.com/watch?v=IhvVoKGyl8E
A five-level examination is mandatory in the diagnosis of complex disorders of the hip. The examination will adequately assess the osseous (level 1), capsulolabral (level 2), musculotendinous (level 3), neurovascular (level 4) and kinematic chain (level 5) helping to direct appropriate tests and treatment modalities[21]
Some specific tests are especially helpful when evaluating a patient with posterior hip pain. The seated piriformis stretch test (Fig. 2) is a passive flexion, adduction with internal rotation test performed as the examiner palpates the deep gluteal region. The active piriformis test (Fig. 3) is an active abduction and external rotation test while the examiner monitors the piriformis. The combination of the seated piriformis stretch test with the piriformis active test has shown a sensitivity of 91% and specificity of 80% for the endoscopic finding of sciatic nerve entrapment[22]
The palpation of the gluteal structures is fundamental for the diagnosis of gluteal pain. Using the ischial tuberosity as a reference, the production of pain by palpation can guide the probable source of symptoms as follows: at the sciatic notch, piriformis syndrome (Fig. 4A); lateral to the ischium, ischial tunnel syndrome or ischiofemoral impingement (Fig. 4B); and medial, pudendal nerve entrapment
ischiofemoral impingement and ischial tunnel syndrome (also known as hamstring syndrome). In the first case, a provocative test should be performed with the patient in the contralateral decubitus position and taking the affected hip into passive
Ischiofemoral impingement test. (A) The symptomatic hip is passively taken into extension with zero abduction or adduction. A positive test is the recreation of the posterior hip pain. (B) The symptomatic hip is passively taken into extension with abduction without pain.
In the first case, a provocative test should be performed with the patient in the contralateral decubitus position and taking the affected hip into passive extension. The findings of this test are considered positive when the symptoms are reproduced in adduction or the neutral position, whereas extension with abduction does not reproduce the symptoms
During active hamstring test muscle strength shows marked weakness and pain at 30-degree knee flexion, whereas strength is normal and pain is improved at 90-degree knee flexion (Fig. 6A and B). Differential diagnoses of deep gluteal pain are summarized in Table I
Examination:
we found fve diagnostic procedures: (1) history taking, (2) physical examination, (3) imaging tests, (4) response-to-injection, and (5) nerve-specifc tests[4]
For that reason the term ‘deep gluteal syndrome’ instead of ‘piriformis syndrome’ is now preferred to describe the presence of pain in the buttock caused from non-discogenic and extrapelvic entrapment of the sciatic nerve [23]
Management[edit | edit source]
Try and make as clear a diagnosis as possible, because you can see that the symptomatology can be so different.
Patient education, show them the anatomy, the structures that could be causing their symptoms and try and get them to understand the possible pathogenesis of their condition.
If I think there's chronic pain or central mediated component,
I'll educate them on that and discuss things such as fear-avoidance or catastrophisation as appropriate.
Advise the patient on the management of the condition.
Hamstring tendinopathy:
Avoid deadlifts and other exercises that compress the Hamstring tendon, and the Sciatic Nerve.
Avoid Hamstring stretches such as straightening the leg at 90 degrees of hip flexion, because that's going to compress the Hamstring tendon onto the Ischial tuberosity.
Sciatic Nerve involvement and you have positive neurodynamic tests, you can advise the patient:
Put the car seat closer to the steering wheel when driving to take that neural tension off the Sciatic Nerve.
If they're a runner and they have pain with hip extension, you may instruct them to reduce their stride length to relieve those symptoms.
If they have Pudendal Nerve type symptoms, you may refer the patient to a woman or men's health physiotherapist to assist you with the symptoms such as rectal pain or faecal incontinence or urinary incontinence, for example.
And if they are a female and they're over 50, you may refer them to the gynaecologist to assist their hormonal status.
And if you think that they are overweight, you may discuss weight management or a healthy lifestyle with the patient.
You may discuss sleep hygiene as a good seven to eight hours of sleep can really be helpful.
And you may discuss the risk factors of smoking and all the other ancillaries that you need to you look at to try and get the best outcome with these patients.
Myofascial release can be helpful with these patients. It can be a very helpful manual therapy type tool in conjunction with the appropriate rehabilitation and advice.
But good palpation skills in this region are helpful diagnostically and can really help release thickened areas, especially around the Sacrotuberous Ligament or Sacrospinous Ligament.
Exercises[edit | edit source]
The purpose of rehabilitation is to gain mobility and maintain movement of the hip joint and avoid any type of stretching of the nerve that can produce neuralgia or neuropraxy[23]
Try and limit the exercises to 15 or 20 minutes a day to improve your compliance and your adherence
And certainly, for tendinopathy in the short-term, avoid stretching and compressive or tensile loading until the symptoms reduce then you can introduce those type of exercises to their programme.
Tendinopathy rule of thumb is that you shouldn't really push tendon pain to more than a four out of ten pain and no worse at 24 hours afterwards. And those are recognised tendinopathy principles for the lower limb. It's different for the upper limb. So for the lower limb, no more than a build-up to a four out of ten pain. However, if your patient is performing a functional loading exercise, such as a step-down or one-legged squat, a dynamic lunge, for example, a split squat. Then no pain should be allowed at that, while doing that exercise. Because pain during a functional loading exercise may imply that the patient's biomechanics are incorrect and they're going into medial collapse. So be very cautious of that.
Piriformis is a hip abductor and external rotator below 45 to 60 degrees of hip flexion. Once it goes above 60 degrees of hip flexion, Piriformis becomes an internal rotator. So if you want to stretch Piriformis with the hip at 90 degree, the hip needs to be at an external rotation position, not internally rotated. So understand the anatomy so you can specifically direct your stretches to the structures that are, you are trying to target. So Piriformis becomes an internal rotator once the hip is flexed to 60 degrees or more.
Neurodynamic gliding techniques, such as a Sciatic Nerve slider.
Gluteal strengthening and buttock strengthening such as bird-dog, split squats, and functional loading exercises.
Progressive loading with emphasis on hip extensors, abductors and lateral rotators as a general rule.
Sometimes with these patients, the pain is just so severe, the Sciatic Nerve referral and the radicular pain is unbearable and we aren't getting a good outcome with good conservative measures. And for some of these patients, then an image-guided anaesthetic block or steroid might be effective. Some of the surgeons are now doing rhizotomies on these regions, which can be effective[5].
Some surgeons are doing partial lesser trochanteric plastics for Ischiofemoral Impingement.
Arthroscopic or endoscopic releases of adhesions between Hamstring tendons, or of the Piriformis tendon as it relates to the Sciatic Nerve. So there are some surgical options that have been recognised[24][17].
Graphs from slides
Table:
•History of repetitive hamstring loading with hip flexion (Reactive hamstring tendon, bursitis)
•Uphill running
•Deadlifts
•Picking up boxes / other loading flexion activity
•Feels like is sitting on a boggy mass (Reactive hamstring tendon, bursitis)
•Pain radiates down leg with hip flexion (Sciatic N – from buttock or discogenic?)
•Increased time on the bike / change in saddle (Pudendal N)
•Sitting on a toilet seat eases (Pudendal N)
•Pain with hip extension or long strides (IFI, lumbar facet, SIJ)
•History of trauma or hip surgery (IFI)
•Limping after prolonged sitting (GT , obturator / gemelli tendinop)
•Lumbar spine pathology ruled out
•No studies relating March test to DGS
•No Studies relating ASLR test to DGS
•Test Hip Total arc of motion (TAM) to differentiate from intra-articular hip.
•FADIR: A negative test rules OUT OA hip
•FADER-Resisted isometric IR
•Pain deep buttock, not lateral hip
•FABER
•Sciatic Nerve glides across posterior border of greater trochanter.
•Pain with resisted hamstring tests
•Ischiofemoral impingement test
•+ Slump test
•Possible abnormal reflexes or motor weakness
•+ Nerve Conduction test, MRI
•Palpation – site of pain assists diagnosis as well as palpable feeling of tissue swelling
•
References[edit | edit source]
- ↑ McCrory P, Bell S (1999) Nerve entrapment syndromes as a cause of pain in the hip, groin and buttock. Sports Med 27(4):261–274
- ↑ Frank RM, Slabaugh MA, Grumet RC, Virkus WW, Bush-Joseph CA, Nho SJ (2010) Posterior hip pain in an athletic population: differential diagnosis and treatment options. Sports Health 2(3):237–246
- ↑ 3.0 3.1 3.2 3.3 3.4 Bell-Jenje T. Differentiating Buttock Pain (Part 3). Physioplus Course 2020
- ↑ 4.0 4.1 Kizaki K, Uchida S, Shanmugaraj A, Aquino CC, Duong A, Simunovic N, Martin HD, Ayeni OR. Deep gluteal syndrome is defined as a non-discogenic sciatic nerve disorder with entrapment in the deep gluteal space: a systematic review. Knee Surgery, Sports Traumatology, Arthroscopy. 2020 Apr 3:1-1.
- ↑ 5.0 5.1 Filler AG, Haynes J, Jordan SE, et al. Sciatica of nondisc origin and piriformis syndrome: diagnosis by magnetic resonance neurography and interventional magnetic resonance imaging with outcome study of resulting treatment. J Neurosurg Spine 2005; 2: 99–115
- ↑ 6.0 6.1 Martin HD, Shears SA, Johnson JC, et al. The endoscopic treatment of sciatic nerve entrapment/deep gluteal syndrome. Arthroscopy 2011; 27: 172–81
- ↑ Meknas K, Christensen A, Johansen O (2003) The internal obturator muscle may cause sciatic pain. Pain 104(1–2):375–380
- ↑ Vicentini JR, Martinez-Salazar EL, Simeone FJ, Bredella MA, Palmer WE, Torriani M. Kinematic MRI of ischiofemoral impingement. Skeletal Radiology. 2020 Jul 7:1-0.
- ↑ Cox JM, Bakkum BW. Possible generators of retrotrochanteric gluteal and thigh pain: the gemelli-obturator internus complex. J Manipulative Physiol Ther 2005; 28: 534–8
- ↑ Johnson KA. Impingement of the lesser trochanter on the ischial ramus after total hip arthroplasty. Report of three cases. J Bone Joint Surg Am 1977; 59: 268–9.
- ↑ Taneja AK, Bredella MA, Torriani M. Ischiofemoral impingement. Magn Reson Imaging Clin N Am 2013; 21: 65–73.
- ↑ Gollwitzer H, Banke IJ, Schauwecker J, Gerdesmeyer L, Suren C. How to address ischiofemoral impingement? Treatment algorithm and review of the literature. Journal of Hip Preservation Surgery. 2017 Dec;4(4):289-98.
- ↑ Wilson MD, Keene JS. Treatment of ischiofemoral impingement: results of diagnostic injections and arthroscopic resection of the lesser trochanter. J Hip Preserv Surg 2016; 3: 146–53
- ↑ Safran M, Ryu J. Ischiofemoral impingement of the hip: a novel approach to treatment. Knee Surg Sports Traumatol Arthrosc 2014; 22: 781–5.
- ↑ 4. Gomez-Hoyos J, Martin RL, Schroder R et al. Accuracy of 2 clinical tests for ischiofemoral impingement in patients with posterior hip pain and endoscopically confirmed diagnosis. Arthroscopy 2016; 32: 1279–84
- ↑ Goom TS, Malliaras P, Reiman MP, Purdam CR. Proximal hamstring tendinopathy: clinical aspects of assessment and management. journal of orthopaedic & sports physical therapy. 2016 Jun;46(6):483-93.
- ↑ 17.0 17.1 Aguilera-Bohorquez B, Cardozo O, Brugiatti M, Cantor E, Valdivia N. Endoscopic treatment of sciatic nerve entrapment in deep gluteal syndrome: clinical results. Revista Española de Cirugía Ortopédica y Traumatología (English Edition). 2018 Sep 1;62(5):322-7.
- ↑ Martin R, Kivlan B, Martin HD. Greater Trochanter-Ischial Impingement: A Potential Source of Posterior Hip Pain. Rio de Janeiro: International Society for Hip Arthroscopy, 2014.
- ↑ Benson B, Schutzer SF. Posttraumatic Piriformis syndrome: diagnosis and results of operative treatment. J Bone Joint Surg Am 1999; 81: 941–9
- ↑ Papadopoulos EC, Khan SN. Piriformis syndrome and low back pain: a new classification and review of the literature. Orthop Clin North Am 2004; 35: 65–71
- ↑ Martin HD, Palmer IJ. History and physical examination of the hip: the basics. Curr Rev Musculoskelet Med 2013; 6: 219–25
- ↑ Martin HD, Kivlan BR, Palmer IJ, et al. Diagnostic accuracy of clinical tests for sciatic nerve entrapment in the gluteal region. Knee Surg Sports Traumatol Arthrosc 2014; 22: 882–8.
- ↑ 23.0 23.1 Martin HD, Reddy M, Gómez-Hoyos J. Deep gluteal syndrome. Journal of hip preservation surgery. 2015 Jul 1;2(2):99-107.
- ↑ Kay J, Morrison L, Fejtek E, Simunovic N, Martin HD, Ayeni OR. Surgical management of deep gluteal syndrome causing sciatic nerve entrapment: a systematic review. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2017 Dec 1;33(12):2263-78.